A New Simple, Tactile, Laryngeal Manoeuver, to Confirm Correct Placement of an Endotracheal Tube
Seyed Ali Emami Meybodi, M.D2, Pooya Kalani, M.D3, Farhad Tavakoli, M.D3 Mohammad Taghi Beigmohammadi, M.D4, Mir Saeed Yekaninejad Ph.D5
Affiliation
- 1Professor of Anesthesiology & Intensive Care, Department of Anesthesiology & Intensive Care, Imam Khomeini Medical Complex, Tehran University of Medical Sciences, Iran
- 2Assistant Professor of Anesthesiology & Intensive Care, Imam Khomeini Medical Complex, Tehran University of Medical Sciences, Iran
- 3Anesthesiologist, Tehran University of Medical Sciences, Iran
- 4Associate Professor of Anesthesiology & Intensive Care, Imam Khomeini Medical Complex, Tehran University of Medical Sciences, Iran
- 5Assistant Professor of Biostatistics, Tehran University of Medical Sciences, Iran
Corresponding Author
Zahid Hussain Khan, Professor of Anesthesiology & Intensive Care, Department of Anesthesiology & Intensive Care, Imam Khomeini Medical Complex, Tehran University of Medical Sciences, Iran, Tel. +982166581576; E-mail: khanzh51@yahoo.com
Citation
Khan, Z.H., et al. A New Simple, Tactile, Laryngeal Manoeuver, to Confirm Correct Placement of an Endotracheal Tube. (2017) J Anesth Surg 4(1): 39- 44.
Copy rights
© 2017 Khan, Z.H. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Paradoxical movement; Endotracheal tube; Laryngeal maneuver; Cricothyroid complex; Tracheal intubation; Esophageal intubation.
Abstract
Background: Confirmation of correct placement of the endotracheal tube is vitally important when performing endotracheal intubation. Most of the tests used to confirm the correct location of the tracheal tube have their own inherent drawbacks. Herewith, we introduce a new method which we hypothesize possesses high reliability when securing the airway.
Methods: One hundred and seventy eight patients, ASA 1, non-pregnant and without head and neck abnormality were studied. Anesthesia technique and monitoring were the same for all the patients. The cricothyroid complex was manipulated using a digital maneuver both after esophageal and endotracheal intubation, for all the patients and any paradoxical movement of the endotracheal tube was recorded during the maneuver to confirm either endotracheal intubation or esophageal intubation. The test parameters included true positive, false positive, true negative, false negative, sensitivity, specificity and accuracy for paradoxical motion, based on the tracheal tube position. The relationship between the extent of tracheal tube movement and the position of tracheal tube was analyzed and a p value < 0.05 was considered to be statistically significant.
Results: The mean age of the patients was 40.5 ± 14.6. The paradoxical motion test was 93.3% sensitive, and 77.5% specific, in the diagnosis of correct anatomical placement of the tracheal tube. One hundred and sixty six (93.2%) patients were diagnosed as true positive. Positive and negative predictive value of paradoxical motion was 80.6% and 92.0%, respectively, with an accuracy rate of 85.4%.
Conclusions: Paradoxical movement of the endotracheal tube after digital cricothyroid complex movement, is an appropriate and a diagnostic test to confirm the insertion of the tube in the trachea, and is an additional important test to ensure correct placement of the endotracheal tube.
Introduction
Tracheal intubation is one of the most commonly performed medical procedures in operating rooms, emergency departments and in pre-hospital setting resuscitations all over the world. End-tidal CO2 monitoring (capnography) has become the gold standard measurement used to confirm that the endotracheal tube (ETT) is indeed in the trachea[1]. Although not 100% reliable most clinicians agree that ETCO2 monitoring is the most reliable method to confirm tracheal placement of an ETT. However in many parts of the world this technology is not available especially in a pre-hospital setting, therefore in those settings clinical methods are still used to confirm endotracheal placement. The most frequently used clinical method, in the absence of advanced technology, is auscultation of the chest bilaterally. Although not totally reliable it is a very useful method of confirming endotracheal tube placement. One of the main disadvantages of the auscultatory method of confirming ETT placement is that in order to confirm correct placement of an ETT, the lungs must be ventilated using several liters of oxygen enriched gases. Unfortunately if the ETT is in the esophagus, this large quantity of gas will be discharged in to the gastrointestinal tract, thereby exposing patients to an increased risk of regurgitation of acid rich gastric contents. Ideally we need a rapid, reliable method of confirming ETT placement before insufflation in order to reduce the risk of regurgitation of gastric contents.
Following is a description of this new method of confirming ETT placement in the trachea.
Description of a new clinical method of confirming endotracheal tube placement
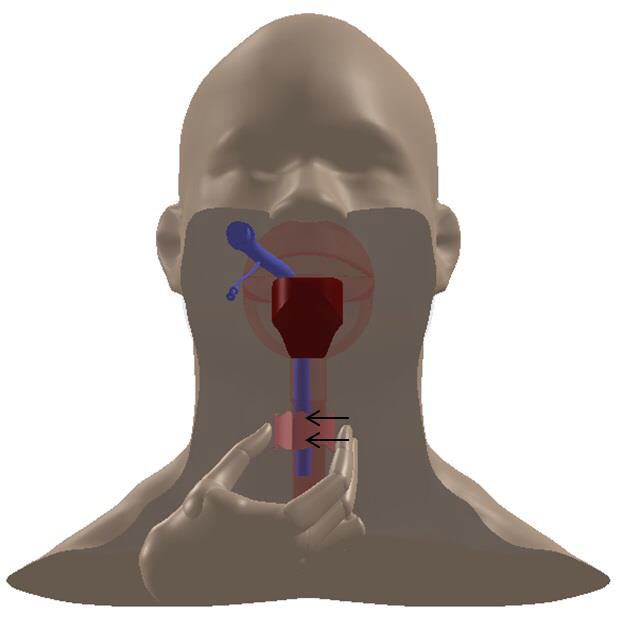
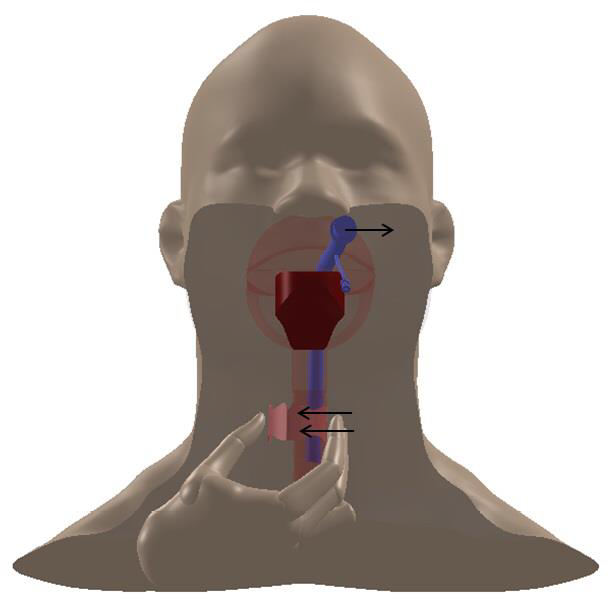
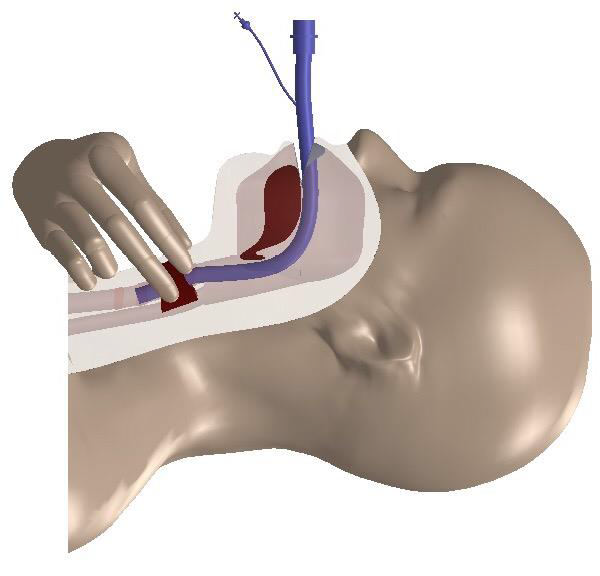
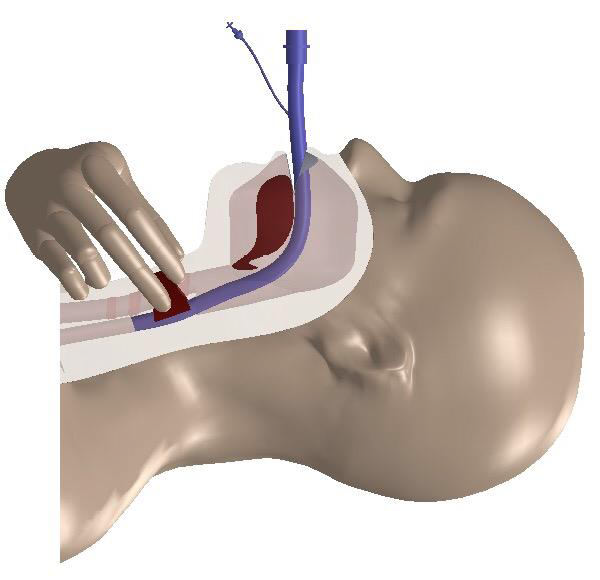
In our practice we routinely manipulate the crico-thyroid complex in the process of ETT intubation (Figure 1). We recently observed, in the process of performing tracheal intubation, that the tracheal tube moved to the opposite side of the mouth(paradoxical movement) when the crico-thyroid complex was displaced to one or other side in a significant number of patients. In other words if the crico-thyroid complex was displaced to the right side following intubation we observed that the endotracheal tube paradoxically moved to the left side of the mouth in a significant number of cases as depicted in anteroposterior and lateral views (Figure 2A and 2B). We also observed that this paradoxical movement of the endotracheal tube did not occur, to any significant degree when the ETT tube was inadvertently placed in the oesophagus(Figure 3). In order to test the value of this new test we designed and completed the following study
Figure 1: Manipulation of the crico-thyroid complex after endotracheal intubation.
Figure 2A: Movement of the ETT to the left side during digital laryngeal manipulation to the right side reflecting its correct placement in the trachea (true positive) in anteroposterior view.
Figure 2B: Pronounced paradoxical motion of the ETT after DLM reflecting its correct placement in the trachea (true positive) in lateral (B) view.
Figure 3: Despite digital laryngeal maneuver (DLM), there was little or no motion of the ETT reflecting esophageal intubation.
Materials and Methods
Following ethics approval (‘’IRCT2015031320676N2” code) and informed consent, 178 healthy patients (ASA 1), scheduled for elective surgery, under general anesthesia, participated in this study. Pregnant patients and those with anatomic or pathologic abnormalities of the head, neck or upper chest region or patients with known airway abnormalities were excluded from the study. An informed consent was obtained from all the patients recruited in the study. All patients were NPO (nil per os) for at least 8 hours prior to the procedure. Routine monitors were applied and preoxygenation was performed prior to induction. Fentanyl 2 micrograms per kilogram was administered prior to induction and patients were induced with thiopental 3 - 5 mgs/kg and atracurium 0.5 - 0.6 mg/kg was administered to provide neuromuscular blockade. An appropriate sized endotracheal tube was inserted first into the esophagus in each patient using the Glidescope for visualization. Then the digital laryngeal maneuver (DLM) was performed by moving the crico-thyroid complex to the right side. If there was little or no movement of the ETT in the mouth this observation was recorded as a True Negative (TN). If there was significant movement of the tube in the mouth to the opposite side of the mouth(paradoxical movement) this was considered to be a False Positive(FP). The tube was then removed from the esophagus and the patient was reoxygenated. Then the airway was once again exposed using the glidescope and an appropriate sized ETT was inserted into the trachea and the DLM was again performed and the results tabulated as described above. If the ETT moved significantly in the mouth to the opposite side this was considered to be a True Positive (TP) and if not it was recorded as a True Negative(TN). These same procedures were carried out on each patient until the study was completed. In order to remove bias from the observers, the individual performing the intubations was not the person observing the results of the DLMs. There was some variation in the movement of the ETT with the DLM therefore we used a simple grading system to record our observations: If the ETT did not move at all with the DLM it was graded 0. If the ETT moved but did not reach the center of the philtrum it was graded as a 1. If the ETT moved to the center of the philtrum it was graded as a 2 and if the ETT crossed the midline of the mouth it was graded as a 3.
Statistical Analysis
We used the tracheal tube position or location as our gold standard to calculate test parameters including true positive (TP), false positive (FP), true negative (TN), false negative (FN), sensitivity (Se), specificity (Sp), and accuracy (Acc) for paradoxical motion in a standard 2 × 2 table. A p value < 0.05 was considered to be statistically significant. According to our hypothesis, the extent of tracheal tube movement is important for diagnosing the status and location of the tracheal tube. If the tube is in the trachea, it shows substantial paradoxical movement at higher grades; on the other hand if the tube is in the esophagus, it moves less or not at all. We used Chi-square test of trend for finding the relationship between the extent of tracheal tube movement and the anatomical location and position of the tracheal tube.
Results
One hundred and seventy eight patients were studied. The mean age of the patients was 40.5 years (SD = 14.6) with the male gender comprising 76 (39.2%) of the patients. Paradoxical motion showed a 93.3% sensitivity, (95% CI; 88.5 – 96.5) and 77.5% specificity, (95% CI; 70.7 – 83.4) in verifying the diagnosis that the tracheal tube was in its correct anatomical position i.e. the trachea. One hundred and sixty six patients were diagnosed as positive (TP rate = 93.2%). Thirty eight patients were graded as Ι (22.9 %), 73 patients as grade ΙΙ (44.0 %) and fifty five patients were confirmed as grade ΙΙΙ (33.1%). Positive predictive Value (PPV) of paradoxical motion was high i.e., 80.6% (95% CI; 74.5 – 85.7) and so was the Negative predictive value (NPV) i.e., 92.0% (95% CI; 86.4 – 95.8). The accuracy rate was found to be 85.4% in this study (Table 1). When the tracheal tube is in the trachea, 77.1% of the movements are grade two or three, whereas, this movement is seen in just 22.5% of cases to be two or three plus when the tracheal tube is in the esophagus. In other words, the movement is more marked and pronounced in true positive cases and less so in false positive cases (p < 0.001) (Table 2).
Table 1: Diagnostic test statistics for paradoxical motion in predicting endotracheal tube position.
| Predicting test | TP | FP | TN | FN | Acc% (95% CI) | Se% (95% CI) | Sp% (95% CI) | PPV% (95% CI) | NPV% (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Paradoxical motion | 166 | 40 | 138 | 12 | 85.4(81.3 - 88.9) | 93.3(88.5 - 96.5) | 77.5(70.8 - 83.4) | 80.6(74.5 - 85.7) | 92(86.4 - 95.8) |
Acc: accuracy or total correct prediction; Se: sensitivity; Sp: specificity; PPV: positive predictive value; NPV: negative predictive value; CI: confidence interval. TP: true positive; FP: false positive. TN: true negative; TP : true positive.
Table 2: Relationship between grade of paradoxical motion test and status of tracheal Tube.
| Status of Tracheal tube | Grade | Total | |||
|---|---|---|---|---|---|
| 0 | † | †† | ††† | ||
| Tracheal | 12 (6.7%) | 28(21.3%) | 73(41.1%) | 55(39.9%) | 178(100%) |
| Esophageal | 138(77.5%) | 31(17.4%) | 6 (3.4%) | 3 (1.7%) | 178(100%) |
Discussion
Endotracheal intubation is a relatively simple technique in most circumstances and the rapid evolution of technology to enhance our ability to make this technique easy to achieve often overshadows the importance of verifying that the tube is not just in the trachea but appropriately positioned in the trachea. In the developed world we have all sorts of devices to facilitate endotracheal intubation and to verify correct placement of the tube such as capnography and capnometry but in many parts of the world we do not have these technologies. This is particularly true in the pre-hospital setting where most of the resuscitations are carried out by non-MD personnel who have to deal with airway problems in very difficult circumstances. In these situations they must rely on clinical methods to verify correct endotracheal tube placement. Bilateral auscultation of the lungs is the most reliable technique in those circumstances. In this study we have introduced a relatively simple test that can be used to verify endotracheal tube placement. This new test offers some advantages. Although like most of the tests we use, it is not 100% reliable. However the test itself is very simple to perform and the time it takes to determine the result is less than 10 seconds and can be performed before you attempt to inflate the lungs or the stomach. The sensitivity of this test is comparable, within one percentage point of auscultation of the lungs[1] but the advantage it has over auscultation is the speed of execution. In most circumstances it takes much longer to perform auscultation than it does to perform the DLM test and if the tube is located in the esophagus extensive insufflation of the gastrointestinal tract with large volumes of gas occurs. This study however, has a few limitations. The first limitation is that this study was undertaken in elective surgeries when patients had received full doses of muscle relaxants which does not simulate intubations in the field in a pre-hospital setting, and secondly the pediatric population and obstetric patients were not included in the study. It could be argued that the placement of two ETTs, one in the esophagus and the other in the trachea, was against ethical standards and contrary to acceptable medical practice. We informed the Ethics Committee that elective esophageal intubation, carried out in patients who were NPO for at least 8 hours, was entirely safe and the best way to test our hypothesis. The Ethics Committee agreed with our proposal and approved the study. Our justification for placing two endotracheal tubes, one in the esophagus and one in the trachea of each patient was twofold. First each patient was used as their own control and second, it would require a very extensive study to accumulate 178 esophageal intubations in a regular operating room practice.
Our new maneuver is the fastest method for determining correct placement of the tracheal tube after intubation and statistically confirms a correlation between paradoxical motion and the location of the tracheal tube. However, we do not advocate the placement of an ETT in the esophagus in non- fasting patients and pregnant patients if a future research is to be conducted and the study replicated. Nevertheless, if the care provider wants only to confirm that the ETT inserted into the trachea is in fact in the trachea and not in the esophagus, he should simply perform this simple and quick maneuver to confirm the right location of the ETT and thus avoid catastrophic complications. The paradoxical motion of the ETT thus obtained would guarantee that the ETT has been correctly placed in the trachea. However, if a capnograph is available, it should be utilized to further confirm the correct placement of the ETT. Our simple maneuver instantaneously reveals results. Thus in case of absent paradoxical movements, the ETT should be immediately removed and a second ETT introduced into the trachea utilizing a glidescope or a fiberoscope whichever is available and feasible. If none is available and mask ventilation is possible, a face mask ventilation should be initiated till such time that the patient awakens or a laryngeal mask airway can be inserted. In our study, 12 cases had false negative results and the maneuver failed to determine the tracheal position of tube because of obesity, short neck and broken teeth. Because of trachea- esophageal interconnections, false positives might be observed in some cases.
We also hypothesized that the extent of tracheal tube movement was also important in diagnosing the tracheal ETT placement. Thus, when the ETT is correctly placed in the trachea a higher score is achieved during paradoxical motion, and on the contrary when there is sluggish movement or no movement at all then the tube is more likely to be in the esophagus. To arrive at a possible relationship between the extent of tracheal tube movement and its position in the trachea, we used Chi-square test. Applying this statistical test, we observed that when the ETT was inserted in the patient’s trachea 77.1% of the movements were graded as 2 or 3 i.e., showing higher grades. On the other hand, when the ETT was in the esophagus, only 22.5% of the cases scored higher grades i.e., 2 or 3 in terms of tracheal movement were observed. In other words, the tracheal movement shows larger swings in true positive cases and significantly lesser swings in false positive cases (p < 0.001) (Table2). Thus we could predict with a higher degree of certainty that the ETT is in the trachea when higher grades of paradoxical movements were observed, and were cautious when the endotracheal movements were less or lower grades were observed.
Confirmation of the ETT in its right place i.e. the trachea is of vital importance following intubation and in this regard inexpensive tools or tests should preferably be used. Standard monitoring is currently employed to achieve this goal but in some LMICs, they are not available[2,3]. To overcome the paucity of these tools, an additional simple maneuver correctly diagnosing the placement of the ETT could be of potential value and benefit in places or locations where the more sophisticated tools are not available and specially so in pre-hospital settings where the paramedics perform the intubation. The CO2 waveform during the first few breaths does not indicate correct ETT placement, and at least one minute is needed to closely watch the waveform[4]. Also, capnography has other limitations like warm up and calibration time and the requirement for an external power source. In order for a test to be ideal for confirming ETT placement, it should be reliable, simple, quick, safe, and inexpensive; it should also require minimal training, and be functional in patients of different age groups, in various locations, and during difficult intubation scenarios. Unfortunately for these purposes, no single test exists[5]. Verifying proper ETT placement is necessary for all patients after they have been intubated. A large number of methods of verification of correct endotracheal tube placement have been described.
The list is as follows:
• Direct visualization of the tube as it enters the trachea using a laryngoscope[6]
• Abdominal and chest auscultation[7-9]
• Auscultation of epigastric sounds[6]
• Identical excursion of both lungs on auscultation[10]
• Compliance of the Bag-Valve-Mask[6,10]
• Abnormal vital signs[6,10]
• Signs of hypoxemia or cyanosis[11]
• Palpation of the trachea[11,12]
• Tactile digital palpation[13]
• Compression of the chest[14]
• Flexible Fiberoptic Bronchoscopy[15]
• Suction esophageal detection devices[16]
• Pulse oximetry[8,17]
• Lighted stylet[9]
• ETT Cuff volume[18]
• Chest X-ray[14,19]
• Ultrasound[20]
• Trans Thoracic Impedance[21]
• Exhaled Gas Volume[22]
• ETT Condensation[14]
• Infrared sensor stylet[23]
• Capnography and Capnometry[1]
Although listed last, capnography is the most reliable method of detecting incorrect placement of ETTs and should be utilized whenever possible but as mentioned previously this technology is not available to many LMICs especially in a pre-hospital setting where clinicians must rely on auscultation as the most practical method to verify ETT placement. This new test, involving digital, manual displacement of the crico-thyroid cartilages to the right or left side immediately following endotracheal intubation, has been shown to be a very useful way to determine whether an endotracheal tube is correctly placed in the trachea or is in the esophagus and should be added to the long list of methods used to verify endotracheal tube placement, especially in the pre-hospital setting where capnography is not available. The test is simple and requires no additional equipment. It can be executed within seconds of completing intubation. It is reliable and highly sensitive and is a very useful test when capnometry is not available.
Conclusion
Paradoxical movement of the endotracheal tube after its placement with digital laryngeal maneuver of the cricothyroid complex is in fact a litmus test that the tube is in the trachea and nowhere else.
Acknowledge:
We are grateful to Professor Brendan Finucane for having edited the manuscript and suggested changes in it.
Clinical trial number: IRCT2015031320676N2
Registry URL: http://www.irct.ir/searchresult.php?keyword=& id=20676&number=2&prt=8264&total=10&m=1
Conflict of interest:The authors declare no conflicts of interest.
References
- 1. Grmec, S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. (2002) Intensive Care Med 28(6): 701-704.
Pubmed || Crossref || Others - 2. Notrica, M.R., Evans, F.M., Knowlton, L.M., et al. Rwandan surgical and anesthesia infrastructure: a survey of district hospitals. (2011) World J Surg 35(8): 1770-1780.
Pubmed || Crossref - 3. Chao, T.E., Burdic, M., Ganjawalla, K., et al. Survey of surgery and anesthesia infrastructure in Ethiopia. (2012) World J Surgery 36(11): 2545-2553.
Pubmed || Crossref || Others - 4. Sum-Ping, S.T., Mehta, M.P., Symreng, T. Reliability of capnography in identifying esophageal intubation with carbonated beverage or antacid in the stomach. (1991)Anesth Analg 73(3): 333-337.
Pubmed || Crossref || Others - 5. Salem, M.R., Baraka, A. Confirmation of tracheal inubation. In: Hagberg, C.A., edition, Benumof’s airway management, 6th edition Philadelphia. (2013)Mosby Elsevier 657-682.
- 6. Pollard, B.J., Junius, F. Accidental intubation of the oesophagus. (1980) Anaesth Intensive Care 8(2):183-186.
Pubmed|| Others - 7. Andersen, K.H., Hald, A. Assessing the position of the tracheal tube: The reliability of different methods. (1989) Anaesthesia 44(12): 984-985.
Pubmed || Crossref || Others - 8. Guggenberger, H., Lenz, G., Federle, R. Early detection of inadvertent esophageal intubation: Pulse oximetry vs capnography. (1989) Acta Anaesth Scan 33(2): 112-115.
Pubmed || Crossref || Others - 9. Stewart, R.D., Larosee, A., Stoy, W.A. Use of a lighted stylet to confirm correct endotracheal tube placement. (1987)Chest 92(5): 900-904.
Pubmed || Crossref - 10. Howells, T.H., Riethmuller, R.J. Signs of endotracheal intubation. (1980) Anaesthesia 35(10): 984-986.
Pubmed || Crossref || Others - 11. Triner, L. A simple maneuver to verify proper position of an endotracheal tube. (1982) Anesthesiology 57(6): 548-549.
Pubmed || Crossref - 12. Horton, W.A., Ralston, S. Cuff palpation does not differentiate esophageal from tracheal placement of tracheal tubes. (1988) Anaesthesia 43: 803-804.
Crossref - 13. Charters, P., Wilkinson, K. Tactile orotracheal tube placement test. (1987) Anesthesia 42: 801-807.
Crossref || Others - 14. Bissinger, U., Lenz, G., Kuhn, W. Unrecognized endobronchial intubation of emergency patients. (1989) Ann Emerg Med 18(8): 853-855.
Pubmed || Crossref - 15. Vioneswaran, R., Whitfield, J.M. The use of a new ultrathin fiberoptic bronchoscope to determine ET tube position in the sick newborn infant. (1981) Chest 80(2): 174-177.
Pubmed || Crossref || Others - 16. Wee, M.K. Esophageal detection device. Assessment of a new method to distinguish oesophageal from tracheal intubation. (1988) Anaesthesia 43(1): 27-29.
Pubmed || Crossref - 17. McShane, A.L., Martin, J.L. Preoxygenation and pulse oximetry delay detection of esophageal intubation. (1987) J Natl Med Assoc 79(9): 987-992.
Pubmed - 18. Jarvis, D., Russell, D.J. Cuff seal volumes and esophageal intubation. (1988) Anaesth Intensive Care 16(3): 378.
Pubmed - 19. Goodman, L.R., Puttman, E.C. Radiologic evaluation of patients receiving assisted ventilation. (1981) JAMA 245(8): 858-860.
Pubmed || Crossref - 20. Rapheal, D.T., Conrad, F.U. Ultrasound confirmation of endotracheal tube placement. (1987) J Clin Ultrasound 15(7): 459-462.
Pubmed || Crossref - 21. Absolom, M., Roberts, R., Bahlmann, U.B., et al. The use of impedance respirometry to confirm tracheal intubation in children. (2006) Anaesthesia 61(12):1145-1148.
Pubmed || Crossref - 22. Stirt, J.A. Endotracheal tube misplacement. (1982) Anaesth Intensive Care 10(3): 274-276.
Pubmed - 23. Song, Y., Oh, J., Chee, Y., et al. A novel method to position an endotracheal tube at the correct depth using an infrared sensor stylet. (2013) Can J Anaesth 60(5): 444-449.
Pubmed || Crossref || Others