Asymptomatic Zinner's Syndrome Diagnosed during the Sixth Decade of Life: Case Report and Review of the Literature
Diminutto Alberto, Tafuri Alessandro, Porcaro Antonio Benito, Balzarro Matteo, Siracusano Salvatore, Artibani Walter
Affiliation
Urology Clinic, Department of Surgery, Dentistry, Paediatrics and Gynaecology, University of Verona, Italy
Corresponding Author
Maria Angela Cerruto, MD, Urology Clinic, Department of Surgery, Dentistry, Paediatrics and Gynaecology, University of Verona, Italy Borgo Trento Hospital, Piazzale Stefani, 1, 37126, Verona Tel: +390458127701; E-mail: mariaangela.cerruto@univr.it
Citation
Cerruto, M.A., et al. Asymptomatic Zinner’s Syndrome Diagnosed during the Sixth Decade of Life: Case Report and Review of the Literature. (2017) J Anesth Surg 4(2): 97- 99.
Copy rights
© 2017 Cerruto, M.A. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Zinner's syndrome, Seminal vesicle cysts, Ipsilateral renal agenesia
Abstract
Seminal vesicle cysts combined with genitourinary anomalies, named since 1914 Zinner’s syndrome, are rare. We present a case of asymptomatic 61-year-old married man, with known left kidney agenesia and a previous ultrasound history negative for vesicle cyst since one year before. Digital rectal examination was normal. Diagnostic imaging (both ultrasound and magnetic resonance imaging) showed left seminal vesicle cyst without any intravesical protrusion. In the absence of symptoms, a conservative treatment was decided, with a strict clinical and ultrasonographic follow-up. The diagnosis of Zinner’s syndrome was made later, by ultrasound and magnetic resonance imaging, with the development of multilocular seminal vesicle cystic lesion, with a rapid onset (within one year). This malformation should be considered in the differential diagnosis of a pelvic cyst in male patients with renal agenesis.
Introduction
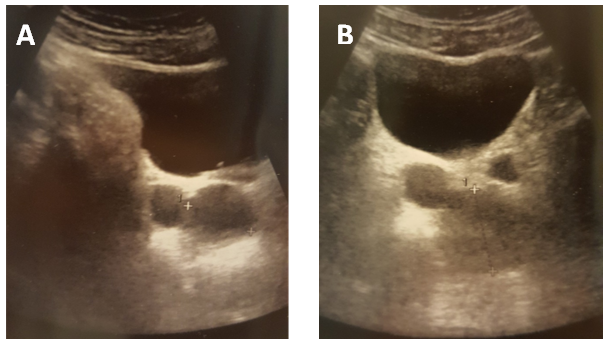
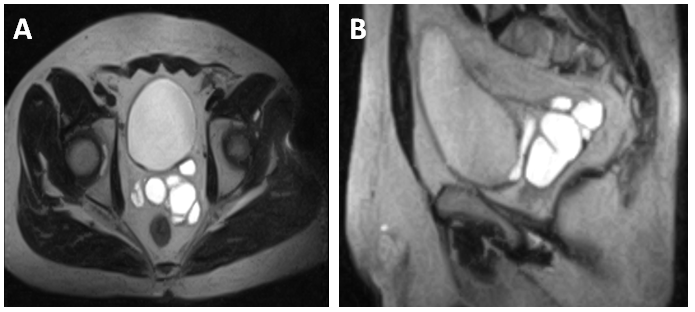
A 61 year-old male with a history of metabolic syndrome (hypertension, obesity, dyslipidemia), left kidney agenesia, compensatory hypertrophy and previous stone disease of the contralateral kidney, was sent by his general practitioner to our department because the incidental diagnosis of left seminal vesicle cyst lesion, not documented in the previous annual ultrasound control. He was father of 2 children and did not complain any lower urinary tract symptoms (LUTS) with a satisfied sexual life. He had a previous history negative for urinary tract infections (UTIs), dysuria, hematuria, ejaculatory pain, prostatitis, epididymitis. The examination revealed a patient in good general condition with body mass index of 29.07. The abdomen was soft with no palpable mass. Digital rectal examination was a normal prostate according with age. Laboratory tests including urine culture and PSA showed no abnormality. Transabdominal ultrasound scan (US) confirmed left kidney agenesia with compensatory hypertrophy and revealed for the first time (not documented in the transabdominal US performed one year before) multiple hypoechoic formations in the site of the left seminal vesicle, the largest with 3.5 cm in diameter, accompanied by a posterior enhancement evoking impure fluid collection, without any intravesical protrusion (Figure 1A - 1B). The radiological assessment was completed by pelvic magnetic resonance imaging (MRI) showing, laterally and posterior located multiloculated cyst lesion in the region of the left seminal vesicle. The diameters of this lobulated multiloculated cystic lesion of the left seminal vesicle was approximately 5.91 x 4.26 cm (Figure 2A - 2B). No sign of bladder involvement was documented.
So far, the patient was asymptomatic and had never presented with dysuria, signs of bladder obstruction or urinary tract infection. He had neither any perineal discomfort nor pain; he described normal ejaculation without pain, no hematospermia, and had never experimented any urinary infection or prostatitis. He also had a normal sexual activity. In this particular case, in the absence of symptoms a conservative treatment was decided, with a strict clinical and transrectal US follow-up, at least until the first symptoms appear.
Figure 1: A-B: The left seminal vesicle cystic lesion at pelvic ultrasound.
Figure 2: The left seminal vesicle cystic lesion in axial (A) and sagittal (B) MRI image.
Discussion
Zinner’s syndrome is an unusual congenital malformation, first described in 1914 by Zinner, characterised by renal agenesis associated with ipsilateral seminal vesicle cysts and obstruction of the ejaculatory duct[1]. Less than 250 cases are reported in the literature[1]. This malformative association is explained by the common embryogenetic origin of the involved organs (mesonephric Wolffian duct)[2].
The pathophysiology of the malformation is explained by an insult occurred during the 4th and 13th week of gestation. From the distal mesonephric duct arise the ureteral bud which induces the differentiation and development of the kidney. The mesonephric duct will differentiate also to epididymis, ejaculatory duct, vas deferens, seminal vesicle, and hemitrigone. Complete failure of the mesonephric duct results to absence of ipsilateral kidney, ureter, hemitrigone, and seminal vesicle. Anomalous development of the distal mesonephric duct results to atresia of the ejaculatory ducts and abnormal ureteral budding; the latter leads to renal agenesis or dysplasia, the former leads to obstruction and cystic dilatation of the seminal vesicles with development of seminal cysts. The development of seminal vesicle cysts is variable along the time life and this variability is not still well explained[3].
Actually seminal vesicle cysts could be congenital or acquired[4]. Acquired cyst usually are found in adults during 2nd to the 5th decade of life, mainly at the time of greatest sexual and reproductive activity[5-7]. It was not the case of our patient that was older with a sudden and late onset of the seminal vesicle occurrence. A cyst is formed when secretions in the gland owing to insufficient drainage, caused to atresia, causes distention of the seminal vesicles. The cysts that were acquired are often bilateral and are discovered after a history of chronic prostatitis or even a prostate surgery[8].
The natural history of congenital seminal vesicle cysts is not well known. Kanavaki et al documented an 11-year history of this malformation from childhood to adolescence with a slow and gradual increase in size of the cyst, from 0.8 cm up to 1.9 cm[9].
Although acquired seminal vesicle cysts usually develop in elderly, they are often bilateral and occur in patients with history of prostatitis or prostate surgery. In the present case, it is unlikely that the cystic lesion is acquired because, despite its rapid onset, there are no obvious causes that might justify its secondary nature.
Usually cyst less than 5 cm in diameter remains asymptomatic and are incidentally discovered by pelvic imaging made for other reasons[10]. The most common symptoms are abdominal, perineal or pelvic pain with or without LUTS, UTIs, and sexual problems. Cysts exceed 12 cm, classified as “giant” cyst, could led LUTS and pelvic pain due to their “mass effect”[10]. Our patient, having a seminal vesicle cystic lesion more than 5 cm but less than 12 cm, never experimented any of these symptoms.
The diagnostic workups include physical examination, transabdominal or transrectal US, computed tomography, and MRI. Both CT and MRI allow to properly investigating renal and seminal vesicles anomalies, which are often combined. MRI exceeds CT in studying abdomen and pelvis not only for the absence of ionizing radiation but also for its imaging capability and soft tissue contrast which are crucial features in the assessment of relations between pelvic organs and structures[11]. In our patient, we performed both transabdominal US and pelvic MRI. Patients without clinical symptoms should not be treated and they can be monitored by transrectal US. Symptomatic seminal vesicle cysts often need mini-invasive surgical treatments such as percutaneous drainage with injection of sclerosing agents[12], laparoscopic[13] or robotic excision[14]. Our case is original as it shows a late and sudden onset of this malformation in the 6th decade of life, usually uncommon, without any symptom.
Conclusion
Zinner’s syndrome is unusual but this syndromic association is known and should be considered in the differential diagnosis of cystic pelvic masses also in males aged over 60 with renal agenesis or dysplasia. Ultrasound is useful for preliminary diagnosis but MRI provides a more detailed analysis and accurate diagnosis. Treatment is considered only for symptomatic patients. A strict follow-up should be proposed for asymptomatic cysts with a sudden onset. We recommend to follow patients with renal agenesia without a previous history of seminal vesicles cysts with a scheduled ultrasound according to patients symptoms. In the case of cyst occurrence we advised to shorten the follow-up (advisable every 6 months).
Sources of funding:
The authors received no external financial support for this study
Conflict of interest:
The authors have no conflicts of interest to declare in relation to this study.
References
- 1. Pereira, B.J., Sousa, L., Azinhais, P., et al. Zinner’s syndrome: an up-todate review of the literature based on a clinical case. (2009) Andrologia 41(5): 322–330.
Pubmed || Crossref || Others - 2. Rappe, B.J.M., Meuleman, E.J.H., Debruyne, F.M.J. Seminal vesicle cyst with ipsilateral renal agenesis. (1993) Urol Int 50: 54–56.
Pubmed || Crossref || Others - 3. Ghonge, N.P., Aggarwal, B., Sahu, A.K. Zinner syndrome: A unique triad of mesonephric duct abnormalities as an unusual cause of urinary symptoms in late adolescence. (2010) Indian J Urol 26(3): 444-447
Pubmed || Crossref || Others - 4. King, B.F., Hattery, R.R., Lieber, M.M., et al. Congenital cystic disease of the seminal vesicle. (1991) Radiology 178(1): 207–211.
Pubmed || Crossref || Others - 5. Liatsikos, E.N., Lee, B., Filos, K.S., et al. Congenital seminal vesicle cyst and coexisting renal agenesis: laparoscopic approach. (2004) Urology 63(3): 584–586.
Pubmed || Crossref || Others - 6. King, B.F., Hattery, R.R., Lieber, M.M., et al. Congenital cystic disease of the seminal vesicle. (1991) Radiology 178: 207–211.
Pubmed || Crossref || Others - 7. Livingston, L., Larsen, C.R. Seminal vesicle cyst with ipsilateral renal agenesis. (2000) AJR Am J Roentgenol 175: 177–180.
Pubmed || Crossref || Others - 8. Kanavaki, A., Vidal, I., Merlini, L., et al. Congenital Seminal Vescicle Cyst and Ipsilaterla Renal Agenesis (Zinner Syndrome): A Rare Association and Its Evolution from Early Childhood to Adolescece. (2015) Eurpean J Pediatr Surg Rep 03(02): 098–102.
Pubmed || Crossref || Others - 9. Slaoui, A., Regragui, S., Abdelouahad, L., et al. Zinner’s syndrome: report of two cases and review of the literature. (2016) Basic and Clinical Andrology 26: 10.
Pubmed || Crossref || Others - 10. Heaney JA, Pfister RC, Meares EM Jr. Giant cyst of seminal vesicle with renal agenesis. (1987) AJR Am J Roentgenol 149:139–40.
Pubmed || Crossref || Others - 11. Fiaschetti, V., Greco, L., Giuricin, V., et al. Zinner syndrome diagnosed by magnetic resonance imaging and computed tomography: role of imaging to identify and evaluate the uncommon variation in development of the male genital tract. (2016) Radiol Case Rep 12(1): 54-58.
Pubmed || Crossref || Others - 12. Cheng, D., Amin, P., Van Ha, T. Percutaneous sclerotherapy of cystic lesions. (2012) Semin Intervent Radiol 29(4): 295–300.
Pubmed || Crossref || Others - 13. Jarzemski, P., Listopadzki, S. Kowalski, M. Laparoscopic Removal of a Congenital Seminal Vesicle Cyst in Zinner's Syndrome. (2014) JSLS 18(2): 367–371.
Pubmed || Crossref || Others - 14. Sridhar, A.N., Zacharakis, E., Dudderidge, T., et al. Robot-assisted management of Zinner’s syndrome: report of seminal vesicle sparing technique and review of literature. (2014) Journal of Robotic Surgery 8(2): 185-187.
Pubmed || Crossref || Others