Cerebral Infarction Caused by Cerebral Venous Thrombosis Associated with Iron Deficiency Anemia
Eun Hye Jeong1, Ku-Eun Lee1, Hyun-Soon Jang1, Mun Kyung Sunwoo1, Byung-Su Kim1, Hyun-Jeung Yu1, Sook Young Roh1, Im-Seok Koh2*
Affiliation
- 1Department of Neurology, Bundang Jesaeng General Hospital, Seongnam, Korea
- 2Department of Neurology, National Medical Center, Seoul, Korea
Corresponding Author
Im-Seok Koh, Department of Neurology, National Medical Center, 245 Euljiro, Jung-gu, Seoul, 100-799, Korea, Tel: 82-2-2260-7290; Fax: 82-2-2272-7540; E-mail: neukoh@naver.com
Citation
Koh. S.I., et al. Cerebral Infarction caused by Cerebral Venous Thrombosis associated with Iron Deficiency Anemia (2015) Int J Neurol Brain Disord 2(2): 1-3.
Copy rights
© 2015 Koh. S.I. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Cerebral infarction; Cerebral venous thrombosis; Iron deficiency anemia
Abstract
Cerebral venous thrombosis (CVT) is a rare condition and has a wide spectrum of symptoms, which makes it difficult to diagnose. CVT has been reported to be associated with various etiologies. However, there are few reported cases of CVT in association with iron deficiency anemia (IDA). Here we report a case of venous infarction caused by CVT associated with IDA. The patient had a good prognosis after iron supplementation and anticoagulation therapy. Since IDA can potentially cause CVT, treatment for IDA may be an important strategy to prevent cerebral infarction caused by CVT.
Introduction
Cerebral venous thrombosis (CVT) is a rare cause of cerebral stroke, contributing less than 1%[1]. The exact incidence is not well known, but the annual incidence is approximately 3 or 4 cases per million[2]. Unlike other causes of stroke, patients show nonspecific symptoms such as headache, vomiting, drowsiness, and lethargy, making it difficult to diagnose[3]. Therefore, imaging with magnetic resonance (MR) venography or CT is recommended for diagnosis in patients with suspected CVT by the American Heart Association[4].
There are many causative conditions for CVT, and the predisposing conditions may be single or multifactorial. Coagulation disorders, oral contraceptives, pregnancy and infection are the most common etiologies. Other causes include trauma, surgery, sinusitis, dehydration, and malignancy[3]. However, there are few reported cases of CVT in association with iron deficiency anemia (IDA), especially in adults.
Here, we report a case of a patient with venous infarction caused by CVT associated with IDA.
Case Report
A 51-year-old woman admitted to hospital with mild headache and left-sided paresthesia starting a day ago. The patient had no specific past or family histories of coagulation abnormalities. But, she had a history of menorrhagia and uterine myoma diagnosed 1 year before admission. She complained of crawling and tingling sensation especially on her left arm. Physical examination revealed pale conjunctivas. There were no definite motor weakness or hypesthesia on neurological examination.
Laboratory test revealed microcytic hypochromic anemia with initial hemoglobin level of 6.6 g/dL (normal range: 12-16 g/dL), a mean corpuscular volume of 62.4 fL and a hematocrit at 25.2% (normal range: 33-51%). Serum iron concentration was 15 ug/dL (normal range: 31-180 ug/dL) and ferritin concentration was 3.02 ng/mL (normal range: 13-150 ng/mL). The results of coagulation studies, autoimmune profiles, homocysteine and tumor markers were normal except for increased D-dimer (0.62 mg/L FEU; normal range: 0-0.49 mg/L FEU) and low level of protein S (52.0%; normal range: 65~140%).
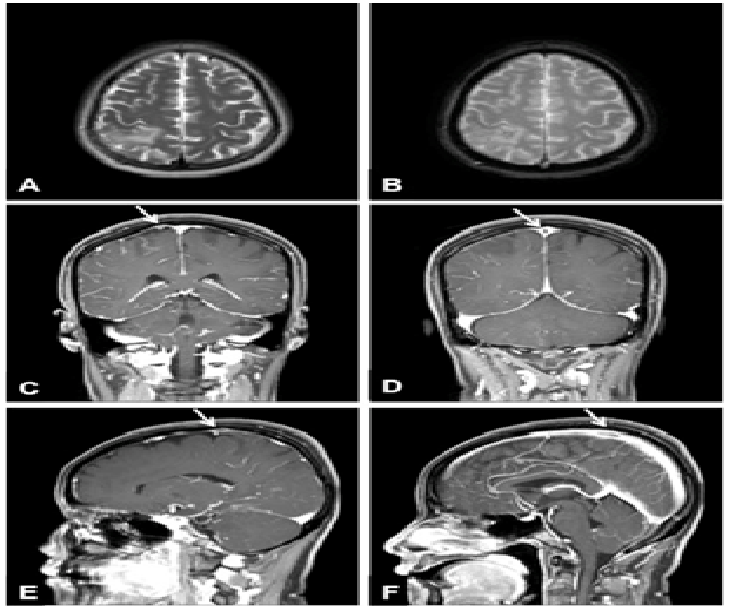
Brain computed tomography (CT) showed focal cortical edema with loss of normal gray matter-white matter distinction and mild gyral swelling in the right parietal lobe. Brain magnetic resonance imaging (MRI) was performed 3 days after admission and showed edematous infarcted lesions with multifocal petechial hemorrhages in the right parietal cortex and subcortical white matter involving post-central gyrus [Figure 1A-1B]. Gadolinium-enhanced T1-weighted MRI revealed filling defect in the superior sagittal sinus and asymmetric engorgement of cortical vein around the infarcted lesions. These findings suggest thrombosis of dural sinus and cortical vein, resulting in venous infarction [Figure 1C-F]. Magnetic resonance angiography (MRA) showed no steno-occlusive lesions or aneurysms.
Figure 1: T2-weighted (A) and gradient-echo images (B) of brain magnetic resonance imaging (MRI) showed edematous infarcted lesions with multifocal petechial hemorrhages in the right parietal cortex and subcortical white matter involving post-central gyrus. Gadolinium-enhanced T1-weighted coronal (C, D) and sagittal (E, F) images of MRI revealed filling defect in the superior sagittal sinus and asymmetric engorgement of cortical vein (arrows), suggesting thrombosis of dural sinus and cortical vein.
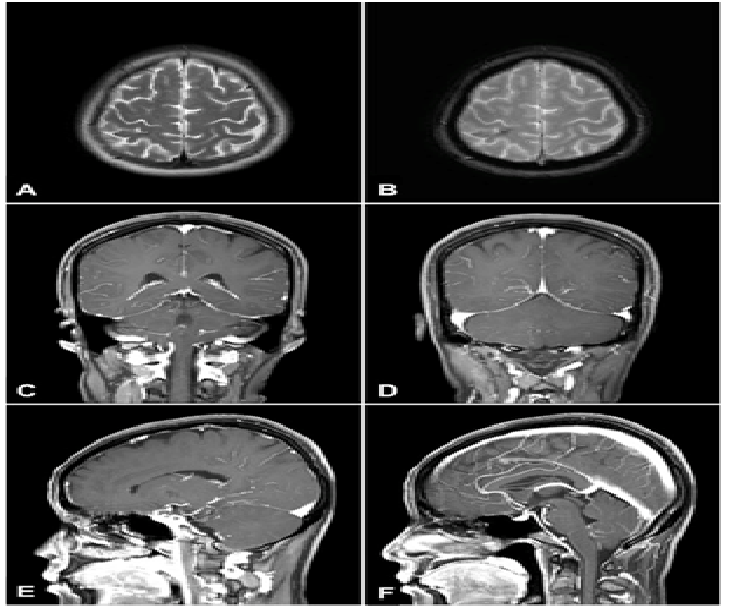
The patient was treated by transfusion with packed red blood cells and oral iron supplementation. Initial anticoagulation with intravenous heparin was followed by oral warfarin. After 10 days, the patient’s symptoms improved completely. After 6 months, MRI showed no definite filling defect in the superior sagittal sinus and cortical vein[Figure 2].
Figure 2: After 6 months, follow-up MRI showed resolved infracted lesions and hemosiderin deposition in the right parietal cortex (A, B). There were no definite filling defects in the superior sagittal sinus and cortical vein on Gadolinium-enhanced T1-weighted images (C-F).
Discussion
CVT is an uncommon disorder usually affecting young individuals, but needs careful approach and consideration due to its potential morbidity[5]. In a multicenter prospective study, 13.4% of patients had residual symptoms resulting in dependency, with a mortality rate of 8.3%[6]. However, because of its variable causes and predisposing conditions, delay in diagnosis is common. Such predisposing conditions for CVT are prior medical conditions (eg, thrombophilias, antiphospholipid syndrome, cancer, inflammatory bowel disease), transient situations (eg, surgery, pregnancy, puerperium, dehydration, infection), selected medications (eg, oral contraceptives, exogenous hormones, substance abuse), and unpredictable events (eg, head trauma)[3]. However, CVT in association with IDA is rare in adults, and there are only few reported cases of CVT in association with IDA[7-10].
We present a case of a female patient presenting with mild headache and left-sided paresthesia, diagnosed of venous infarction due to thrombosis of superior sagittal sinus and cortical vein. She had severe microcytic hypochromic anemia due to iron deficiency, without any other risk factors for CVT such as trauma history, infections, coagulation disorders, or autoimmune diseases. She had good prognosis after iron supplementation and anticoagulation therapy.
IDA has been suggested to be associated with stroke, although it is still difficult to provide direct evidence. There are 3 possible mechanisms by which IDA is suggested to cause thrombosis[11]. First, iron deficiency may cause secondary thrombocytosis because iron is considered to be a regulator of thrombopoiesis. Second, IDA may result in a hypercoagulable state due to reduced red blood cell deformability and increased viscosity. Third, anemic hypoxia may occur in situations with increased metabolic demands in the brain and cause ischemic damage in the area of the brain supplied by the terminal arteries. In our case, the number of platelets was not increased, but the measurement of coagulation parameters suggested the possibility of hypercoagulable state.
Unlike children, in which the major cause of IDA is insufficient dietary iron intake, blood loss is the most common cause of IDA in adults. Blood loss may result from menstruation in premenopausal women, chronic gastrointestinal loss, urine loss (hemoglobinuria, hemosiderinuria) and hemoptysis[12]. One study reported two women with hemorrhagic infarctions due to thrombosis of the superior sagittal and transverse sinus[7]. The severe IDA secondary to uterine myoma seen in those two patients was suggested to play a significant role. Our patient also had uterine myoma and severe IDA, and it was the only precipitating factor of CVT. In conclusion, IDA can cause CVT, and when cerebral infarctionoccurs, anticoagulation therapy with iron supplementation must be done immediately. Furthermore, treatment for IDA may be an important strategy to prevent CVT and subsequent cerebral infarction.
References
- 1. Masuhr, F., Mehraein S., Einhaupl, K. Cerebral venous and sinus thrombosis. (2004) J Neurol 251(1): 11-23.
- 2. Stam, J. Thrombosis of the cerebral veins and sinuses. (2005) N Engl J Med 352(17): 1791- 1798.
- 3. Saposnik, G., Barinagarrementeria, F., Brown, R. D., et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. (2011) Stroke 42(4): 1158- 1192.
- 4. Piazza G. Cerebral venous thrombosis. (2012) Circulation 125(13): 1704- 1709.
- 5. Bousser, M. G., Ferro, J. M. Cerebral venous thrombosis: an update(2007) Lancet Neuro l6(2): 162- 170.
- 6. Ferro, J. M., Canhao, P., Stam. J., et al. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). (2004) Stroke 35(3): 664- 670.
- 7. Aoki, N., Sakai, T. Cerebral sinus thrombosis in patients with severe iron deficiency anaemia due to myoma uteri. (1989) ActaNeurochir 97(3-4): 131- 134.
- 8. Balci K., Utku U., Asil T., et al. Deep cerebral vein thrombosis associated with iron deficiency anaemia in adults. (2007) J Clin Neurosci 14(2): 181- 184.
- 9. Ogata, T., Kamouchi, M., Kitazono T. et al. Cerebral venous thrombosis associated with iron deficiency anemia. (2008) J Stroke Cerebrovasc Dis 17(6): 426- 428.
- 10. Huang, P. H., Su, J. J., Lin P. H. Iron deficiency anemia - a rare etiology of sinus thrombosis in adults. (2010) Acta Neurol Taiwan 19(2): 125- 130.
- 11. Hartfield, D. S., Lowry .N. J., Keene D. L., et al. Iron deficiency: a cause of stroke in infants and children. (1997) Pediatr Neurol 16(1): 50- 53.
- 12. Alleyne, M., Horne, M. K., Miller, J. L. Individualized treatment for iron-deficiency anemia in adults. (2008) Am J Med 121(11): 943- 948.