Comparative Study of Obstetric and Neonatal Outcome between Spontaneous and Induced Labor In Gravid Women After 41 Completed Weeks Of Gestation
Dr. Nabendu Bhattacharjee² , Dr. Apurba Mandal² , Dr. Suchita Kocher² , Dr. Piklu Chaudhury² , Dr. Ranjan Pal¹
Affiliation
1Department of Obstetrics & Gynaecology, North Bengal Medical College, Darjeeling, India
2Department of Obstetrics & Gynaecology, N R S Medical College, Kolkata, India
Corresponding Author
Saha, S. P.Department of Obstetrics & Gynaecology,North Bengal Medical College, Sushsrutanagar,Siliguri, West Bengal, India. Tel:(+91)-(0353)-2585433; E-mail: drsps94@gmail.com
Citation
Saha, S. P., et al. Comparative Study of Obstetric and Neonatal Outcome Between Spontaneous and Induced Labor in Gravid Women after 41 Completed Weeks of Gestation. (2015) J Gynecol Neonatal Biol 1(1): 9-13.
Copy rights
©2015 Saha, S. P. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Pregnancy; Post term; Expectant; Induction
Abstract
Objective: Both the mother and the infant are at increased risk of adverse outcomes when the pregnancy continues beyond term. The problems include induction of labor, caesarean section, prolonged labor, postpartum hemorrhage and traumatic birth. This study compared the results of elective induction versus expectant management of pregnancies at 41 completed weeks.
Material & Method: In a randomized comparative trial 1136 women with 41 completed weeks of gestation, were randomly assigned to either immediate induction with dinoprostone gel or expectant management till 42 completed weeks. Primary outcome measure was caesarean section rate and secondary outcome measures were perinatal outcomes and maternal morbidities.
Results: Cesarean section rate was significantly low in induction group when compared to expectant group (23.06% vs 30.58%, p = 0.039, CMLE OR = 0.758). Maternal morbidities and labor events were comparable in both groups. There was no significant difference in neonatal outcomes between the two groups. Mean maternal hospital stay was significantly less in study group (p < 0.0001, 95% CI = -3.917 to -3.462) but NICU stay of neonates were similar in both groups.
Conclusion: Induction of labor at 41 weeks of gestation for otherwise uncomplicated singleton pregnancies significantly reduce cesarean delivery rates without affecting perinatal outcomes.
Introduction
Both the mother and the infant are at increased risk of adverse outcomes when the pregnancy continues beyond term. Gülmezoglu et al. in their "Cochrane Database Systematic Review 2006", opined that no tests can clearly predict if a baby would be better to be left in the womb or labor induced and the baby be born, so arbitrary time limits for intervention have been suggested[1]. The reported frequency of post-term pregnancy is approximately 7%[2]. The obstetric problems associated with post-term pregnancy include induction of labor with an unfavorable cervix, cesarean section, prolonged labor, postpartum hemorrhage and traumatic birth. Routine early pregnancy ultrasound examination and subsequent adjustment of delivery date appear to reduce the incidence of post-term pregnancy. Hilder in 1998 reported that neonatal and post neonatal death risk is increased after 41 weeks[3]. In a cross-sectional study of birth registry data between 1978 to 1993 in Denmark, Olesen, et al[4] concluded that post term delivery was associated with significantly increased risks of perinatal and maternal complications, the risk of perinatal death was 1.33 (adjusted odds ratio, 95% CI = 1.05 - 1.68).
Induction of labor is widely practiced to try and prevent the problems mentioned above and improve the health outcome for women and their infants. Unfortunately, labor induction may itself cause problems especially when the cervix is not favorable. Furthermore, the ideal timing for induction of labor is not clear. In the past there was a tendency to await spontaneous labor until 42 completed weeks. Some reviews have suggested that routine induction of labor after 41 weeks of gestation appears to reduce perinatal mortality without increasing the incidence of cesarean section[5]. Sanchez-Ramos in 2003 have concluded that labor induction at 41 weeks or more is associated with a reduced cesarean section rate and no difference in perinatal mortality[6]. Hannah in 1993[7] did similar study (inducing labor at > 41 weeks) and found significantly lower cesarean section rates (OR 0.85; 95% CI -0.74 to 0.94), lower PMR than expectant management group (OR 0.23). The SOGC guidelines 1997 advocate elective delivery for women who reach 41 to 42 weeks of gestation[8]. Most recent COCHRANE review demonstrated a lower PMR for induction at 41 weeks and beyond[1].
Fundamentally, there are only 2 overall reasons for a cesarean delivery in labor: cephalopelvic disproportion (commonly diagnosed as failure to progress in labor) or fetal intolerance of labor, which may be due to reduced utero–placental blood flow. Because fetuses continue to grow and placentas continue to age throughout term pregnancies, it is not surprising that these indications might increase with gestational age. The competing risk is failed induction of labor, which probably varies from institution to institution[9]. As a pregnancy continues beyond term the risks of fetus dying inside the womb or in the immediate newborn period increase[10]. Thus there is a need to have studies which will accurately demarcate when the risk of perinatal mortality begins. Our study was a step to evaluate whether induction between 41 to 42 weeks reduces cesarean section and perinatal mortality rates or not.
Aims and objectives
The aim of present study was directed to evaluate the results of elective induction versus expectant management of pregnancies at 41 completed weeks of gestation.
Materials and Methods
This was a prospective randomized comparative clinical trial. We conducted the study over a period of one and half years, from July, 2012 to December, 2013 in two teaching institutions of West Bengal, India viz. North Bengal Medical College and Hospital, Darjeeling and N R S Medical College and Hospital, Kolkata, simultaneously.
1356 pregnant women, who had completed 41 weeks of gestation as calculated by LMP and confirmed by ultrasonography findings, were assessed for enrolment in the study. After going through exclusion criteria a total of 1136 women were ultimately included in the study. Exclusion criteria were (a)Non cephalic presentation (b)Gestational diabetes mellitus (c)PIH (d) Pregnancy with medical disorders such as heart disease, abnormal liver functions, chronic renal disease, pre pregnancy DM severe anemia etc. (e)IUGR and Oligohydroamnios, (f)PROM (g)Presence of contraindications for vaginal delivery (h)Previous CS
Patients were divided into two groups (A and B) using a computer-generated randomization protocol having 581 women in group A (study group) and 582 women in group B (control group). After allocation, relevant history and patient particulars were recorded for each patient. Women in group A received dinoprostone gel (0.5mg) intracervically for induction of labor. Maximum of 3 such gels were given within 24 hrs period with a gap of 8 hours between two doses. Cesarean section was performed in case of failed induction or for any other indication that arose during induction in this group. Expectant management protocol was followed for women in group B. Pregnancy was monitored with daily fetal movement count by mother and serial monitoring by USG, NST and Doppler velocimetry till 42 completed weeks of gestation. In this group of women, pregnancy was terminated by cesarean section if indicated or induction of labor was performed on completion of 42 weeks of gestation.
We used a computer-generated randomization sequence to assign participants into two treatment groups and the allocation was concealed in sealed, sequentially numbered, brown envelopes (opaque), which had been prepared by the statistician of each Centre and handed over to the sister-in-charge of antenatal ward, department of Obstetrics and Gynecology of respective Institutions. The researchers responsible for treating the pregnant women allocated the next available number on entry into the trial in the department of Obstetrics and Gynecology and the treating doctors collected the corresponding sealed envelope directly from sister-in-charge and followed the protocol accordingly. On duty doctors in the labor room, closely monitored maternal and fetal condition during induction. Intervention by cesarean section or instrumental vaginal delivery was performed by on duty resident surgeons according to the needs. The maternal and fetal outcomes were recorded in details. Because of the nature of the study, participants and those administering the interventions were not blinded but those assessing the outcomes were blinded to group assignment.
Primary outcome measure was cesarean section rate and secondary outcome measures were perinatal outcomes and maternal morbidities.
In a systematic review with meta-analysis on management of pregnancies reaching 41 weeks or more[6], the reported rate of cesarean section in women managed expectantly management was 22%. A difference of 7% in cesarean section rate in induction group was used to calculate the sample size having a power of 80 setting alpha error at 0.05. The minimum sample size thus calculated was 496 in each arm for power based on normal approximation and 524 in each arm for power based on normal approximation with continuity correction (Fleiss, Statistical Methods for Rates and Proportions, formulas 3.18 &3.19).
All data entries were visually double checked by an independent second investigator. The data were analyzed using Open Source Epidemiologic Statistics for Public Health (Open Epi, version 2.3.1; updated on 2011/23/06) to compare the outcomes between the study group and the control group. A p-value less than 0.05 were considered as statistically significant. Statistical methods included the two samples independent "t" tests, mid-p exact tests, maximum likelihood odds ratio estimate with confidence limits produced by several methods.
The study was approved by "The Medical Ethical Committee for Human research", North Bengal Medical College & Hospital and "The Committee for Ethical Consideration and Approval for Human Research", N R S Medical College & Hospital, as required by Indian law. Before enrolments for the study entry, all women provided a written informed consent meeting all local institutional requirements.
Results
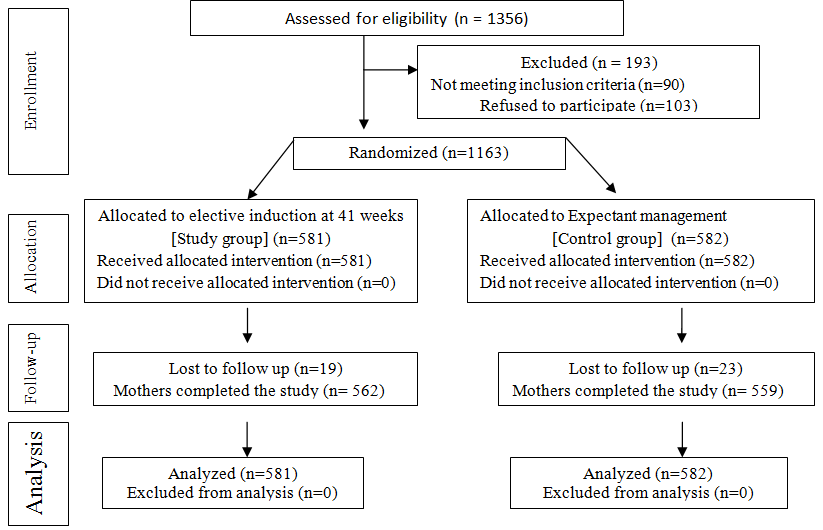
Initially 1356 women were assessed for eligibility criteria to include in this study. 193 women were excluded from the study due to either not meeting the inclusion criteria (n= 90) or refusal for participation (n= 103). 1163 women were thus randomized into two groups (A and B) having 581 patients in study group (Group A) and 582 mothers in control group (Group B). Induction with dinoprostone gel was performed in group A and expectant management protocol was followed in group B. Subsequently 19 women from group A and 23 from group B were lost in follow up. Hence 562 women in group A and 559 in group B completed the study. But all women in both groups who received allocation intervention were analyzed as we adopted the intention to treat protocol (Fig.1).
Demographic profiles of the patients in both groups were comparable in relation to age, parity, BMI, gestational weight gain and AFI (Table 1). From Table 2, it is evident that cesarean section rate was significantly low in induction group when compared to expectant group (134/581 vs 165/582, p = 0.039, CMLE OR= 0.758 and 95% CI = 0.581 to 0.986). Maternal morbidities and labor events were comparable in both groups (Table 3). There was no significant difference in neonatal outcomes between the two groups (Table 4). Mean stay of mothers in hospital was significantly less in study group (p < 0.0001, 95% CI= -3.917 to -3.462) but NICU stay of neonates were similar in both groups (Table 5).
Table 1: Demographic profile
| Characteristics | Study group (n= 581) | Control group(n= 582) | P value (95% CI) |
|---|---|---|---|
| Age in yrs(mean ± sd) | 24.01 ± 3.44 | 23.98 ± 3.31 | 0.353¹(-0.428 to 0.348) |
| BMI | 22.19 ± 1.62 | 22.08 ± 1.53 | 0.168¹(-0.071 to 0.291) |
| Parity | |||
| Nulipara | 468 (80.55%) | 455 (78.18%) | 0.318²(-2.277 to 7.021) |
| Para 1 or more | 113 (19.45%) | 127 (21.82%) | |
| Socio-economic status | |||
| APL* | 354(60.93% ) | 361(62.03%) | 0.701²(-6.691 to 4.495) |
| BPL** | 227(39.07%) | 221(37.97%) | |
| AFI ( mean±sd) | 8.34 ± 0.78 | 8.25 ± 0.81 | 0.363¹(-0.001 to 0.181) |
| Gestational weight gain in Kg (mean ± sd) | 11.89 ± 1.16 | 12.01 ± 0.99 | 0.134¹(-0.249 to 0.009) |
¹ p-value (two-tailed)
²Mid-P exact
Table 2: Labor events, mode of delivery and birth weight distribution between two groups
| Outcome | Study group (n= 581) | Control group (n= 582) | P Value ( 95% CI ) | CMLE OR*( 95% CI ) |
|---|---|---|---|---|
| Vaginal Delivery | 447(76.94%) | 417(69.42%) | 0.039² (0.273 to 10.3) | 1.32(1.013 to 1.72) |
| Spontaneous | 410/447(91.72%) | 389/417(93.28%) | 0.388²(-5.069 to 1.943) | 0.797(0.475 to 1.329) |
| Instrumental | 37/447(8.28%) | 28/417(%) | 0.388²(-1.943 to 5.069) | 1.253(0.752 to 2.105) |
| Cesarean Delivery | 134(23.06%) | 165(30.58%) | 0.039² (-10.3, -0.2732) | 0.758(0.581 to 0.986) |
| Birth Weght in gm(mean ± sd) | 2943±296 | 2967±281 | 0.162¹(-57.65 to 96.58) |
*Conditional maximum likelihood estimate of Odds Ratio
¹ p-value (two-tailed)
² Mid-P exact
Table 3: Condition associated with labor/delivery
| Outcome | Study group(n= 581) | Control group(n= 582) | P Value #( 95% CI ) | CMLE OR*( 95% CI ) |
|---|---|---|---|---|
| Labor Dystocia | 54(9.29%) | 69(11.86%) | 0.157(-6.093 to 0.97) | 0.762(0.521 to 1.11) |
| Fetal intolerance of labor | 51(8.78%) | 49(8.42%) | 0.828 (-2.863 to 3.581) | 1.047 (0.693 to 1.581) |
| Maternal infectious morbidities | 24(4.13%) | 27(4.64%) | 0.675(-2.862 to 1.845) | 0.885(0.501 to 1.56) |
| PPH | 21(3.61%) | 25(4.29%) | 0.556 (-2.921 to 1.559) | 0.835(0.457 to 1.516) |
*Conditional maximum likelihood estimate of Odds Ratio
# Mid-P exact
Table 4: Neonatal Morbidity
| Variable | Study group (n= 581) | Control group(n=582) | P value¹(95% CI) | CMLE OR *(95% CI) |
|---|---|---|---|---|
| Sepsis | 17 (%) | 21(%) | 0.519(-2.725 to 1.361) | 0.805(0.414 to 1.549) |
| Fever | 9(%) | 12(%) | 0.522(-2.043 to 1.017) | 0.747( 0.301 to 1.806) |
| Poor feeding | 13 (%) | 15(%) | 0.711(-2.101 to 1.422) | 0.865(0.399 to 1.854) |
| Perinatal asphyxia | 7(%) | 9(%) | 0.629(-1.68 to 0.997) | 0.766(0.272 to 2.141) |
| NICU admission | 46(%) | 51(%) | 0.604(-4.023 to 2.332%) | 0.895(0.588 to 1.359) |
| Perinatal mortality | 2 | 5 | 0.288(-1.403 to 0.373) | 0.398(0.053 to 2.031) |
¹ Mid-P exact
* Conditional maximum likelihood estimate of Odds Ratio
Table 5: Hospital Stay of mother & NICU Stay of neonate
| Study group(n= 581) | Control group(n= 582) | P value (two-tailed) | 95% CI Of difference | |
|---|---|---|---|---|
| Maternal Stay in days* Mean ± SD | 4.45 ± 1.6 | 8.14 ± 2.3 | < 0.0001 | -3.917 to -3.462 |
| NICU Stay in Days(Mean ± SD) | 5.63 ± 3.59 | 5.71 ± 3.46 | 0.374 | -0.485 to 0.325 |
* Calculated from 41 completed weeks.
Discussion
The risk of perinatal and obstetric complications is high in postdated delivery compared with term deliver. There is a significant increase in the risk of stillbirth, neonatal and post-neonatal mortality in prolonged pregnancy. There is a lack of consensus regarding the management of pregnancy reaching or exceeding 41 weeks. Induction of labor is among the most common obstetric interventions to reduce such risks. The prevailing belief that induction of labor increases the risk of cesarean delivery likely stems from observational studies that compared women who had induction of labor to women with spontaneous labor at a particular gestational age[11]. This association has not been validated by prospective trials. A systematic review of existing literature identified nine randomized controlled trials that reported an overall decreased risk of cesarean section in women who were induced in comparison to those who were expectantly managed, particularly at gestational age (GA) ≥ 41 weeks; evidence is less clear at GA< 41 weeks[11]. In our randomized controlled trial we evaluated whether elective induction of labor between 41 to 42 weeks of gestation reduces cesarean section rate; perinatal mortality and morbidities or not when compared to expectant management.
The cesarean section rate in our study was 23.06% in women who were induced at 41 weeks compared to 28.35 % in those managed expectantly, which was statically significant (p = 0.039, CMLE OR = 0.758 and 95% CI = 0.581 to 0.986). In a Canadian study[13] the cesarean section rate was 21.2% in the induction group compared to 24.5% in the monitoring group for management of pregnancy at 41 weeks or more. The difference was statically significant (p = 0.03).
In a study by Cheng et al[11], risks of cesarean delivery for induction at 40 weeks (aOR, 0.88; 95% CI, 0.86–0.92) and 41 weeks (aOR, 0.89; 95% CI, 0.83–0.95) were lower which was similar to our study. Similarly, in a systematic review with meta-analysis on 'labor induction versus expectant management for post-term pregnancies' Sanchez-Ramos, et al[11] reported that compared with women allocated to expectant management, those who underwent labor induction had lower cesarean delivery rates (OR 0.88; 95% CI 0.78, 0.99). But in study, conducted by the national institute of child health and human development network of maternal-fetal medicine units[13], the cesarean delivery rate was not significantly different in the expectant and induction groups for managing pregnancies reaching 41 weeks. In a Cochrane systematic database review (2006), the authors opined that there was no evidence of a statistically significant difference in the risk of caesarean section (RR 0.92; 95% CI 0.76 to 1.12; RR 0.97; 95% CI 0.72 to 1.31) for women induced at 41 and 42 completed weeks respectively[1].
Though operative vaginal delivery in our study was slightly higher in induction group when compared to expectant group (28/417; 8.28% vs 37/447; 6.72%), the difference was not statistically significant which was in contrast to the findings reported by Cheng et al. in their study in 2012[11] where they had found a significantly higher risk of having an operative vaginal delivery for induction at 41 weeks compared to delivery later.
The difference in mean birth weight between two groups in our study was statistically insignificant (2943 gm vs 2967 gm; p = 0.162; 95% CI= -57.65 to 96.58) which is similar to the findings of the study conducted by The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units in 1994[13].
Labor characteristics in terms of development of labor dystocia and fetal intolerance to labor did not differ in women who were induced from those who were managed expectantly in our study. Cheng, et al[11] reported similar rates labor dystocia in women either induced or managed expectantly at 41 weeks. They also reported that the diagnosis of fetal intolerance of labor was less frequent in women who had induction at 39 weeks (6.15%) compared to delivery later (7.12%; aOR, 0.86; 95% CI, 0.81– 0.92), while no statistically significant differences were seen for 40 or 41week comparisons.
In our study there were no statistically significant differences in rates of perinatal mortalities and morbidities when both groups were compared. The rates of perinatal mortality and morbidities were similar in both induction and expectant management group in the Canadian study done by Hannah et al (1992) which were similar to our observations[12].
Sanchez-Ramos et al in their review in 2003[6] observed that although subjects whose labor was induced experienced a lower perinatal mortality rate (0.09% versus 0.33%, OR 0.41; 95% CI 0.14 to 1.18), the difference was not statistically significant. Similarly, no significant differences were noted for NICU admission rates, meconium aspiration, meconium below the cords, or abnormal Apgar scores. Cheng et al. observed that induction of labor at 41 weeks, compared to expectant management, is associated with decreased risk of composite perinatal morbidity[11].
In our study mean maternal hospital stay in induction group was significantly less when compared to that of expectantly managed group (p < 0.0001, 95% CI = -3.917 to -3.462). But NICU stay of neonates did not vary when both groups were compared.
In our study we could analyze a reasonably large sample size for obstetric and neonatal outcome between spontaneous and induced labor in gravid women after 41 completed weeks of gestation. In this study there was not a single case of discontinued intervention after randomization because of the nature of selection. Number of patients lost in follow up was few and we also adopted the intention to treat principle for analyzing the results. Due to nature of the study it could not be a double blinded method. Another weakness of this study was non implementation of long term follow up of the babies of both groups.
This research focuses on induction of labor without medical indication and expectant management at 41 completed weeks of gestation. We improve our work by using a transparent method to classify inductions as non-medically indicated and the clinically relevant comparison group, expectant management. We stratify and test the association of induction without a medical indication and cesarean delivery, operative vaginal delivery, labor events, neonatal morbidities, NICU admission and maternal hospital stay.
In conclusion, we present evidence that induction without medical indication at 41 completed weeks is associated with reduced odds of cesarean delivery among both nulliparous and multiparous women with a previous vaginal delivery. We find no evidence of any other increased adverse maternal or neonatal outcomes with elective induction. In our study mean maternal hospital stay in induction group was significantly less when compared to that of expectantly managed group which is very much helpful in reducing national cost of medical treatment in developing countries. Focus on induction of labor as a quality metric in obstetrics must be evidence-based. Our research is one step forward in this regard and it will add evidence in the armamentarium of obstetric management in favor of medically non indicated induction particularly in management of post dated pregnancy.
A policy of labor induction at 41 weeks of gestation for otherwise uncomplicated singleton pregnancies significantly reduces cesarean delivery rates without compromising perinatal outcomes. This is also likely to be cost effective considering the significant reduction in maternal hospital stay.
Acknowledgments:
The contributions of the staffs of Pharmacy Departments of North Bengal Medical College, West Bengal and N R S Medical College, India who had been of immense help in conduction of present study, are acknowledged with thanks.
Conflicts of Interest
The authors have no commercial or other conflicts of interest i.e. of financial or other nature. The authors also have no commercial affiliations to disclose also.
References
- 1. Gülmezoglu, A.M., Crowther, C.A., Middleton, P., et al. A study on Induction of labour for improving birth outcomes for women at or beyond term. (2006) Cochrane Database Syst Rev 18(4): CD004945.
- 2. Neff, M.J. ACOG Releases Guidelines on Management of Post-term Pregnancy. (2004) Am Fam Physician 70(11): 2221- 2225.
- 3. Hilder, L., Costeloe, K., Thilaganathan, B. Prolonged pregnancy: evaluating gestation-specific risks of fetal and infant mortality. (1998) Br J Obstet Gynaecol 105(2): 169- 173.
- 4. Olesen, A.W., Westergaard, J.G., Olsen, J. Perinatal and maternal complications related to postterm delivery: a national register-based study, 1978-1993. (2003) Am J Obstet Gynecol 189(1): 222- 227.
- 5. Nielsen, P.E., Howard, B.C., Hill, C.C., et al. Comparison of elective induction of labor with favorable Bishop scores versus expectant management: a randomized clinical trial. (2005) J Matern Fetal Neonatal Med 18(1): 59- 64.
- 6. Sanchez-Ramos, L., Olivier, F., Delke, I., et al. Labor induction versus expectant management for postterm pregnancies: a systematic review with meta-analysis. (2003) Obstet Gynecol 101(6): 1312- 1318.
- 7. Hannah , M. E., Huh, C., Hewson, S.A., et al. Postterm pregnancy: putting the merits of a policy of induction of labor into perspective. (1996) Birth 23(1): 13- 19.
- 8. Delaney, M., Roggensack. A., Leduc, D.C., et al. Guidelines for the Management of Pregnancy at 41+0 to 42+0 Weeks. (2008) J obset Gynaecol Can 30(9): 800- 823.
- 9. Caughey, A.B., Sundaram, V., Kaimal, A.J., et al. Systematic Review: Elective Induction of Labor Versus Expectant Management of Pregnancy. (2009) Ann Intern Med 151(4): 252- 263.
- 10. Menticoglou, S.M, Hall, P.F. Routine induction of labour at 41 weeks gestation: nonsensus consensus. (2002) BJOG 109(5): 485– 91.
- 11. Cheng, Y.W., Kaimal, A.J, Snowden, J.M., et al. Induction of labor compared to expectant management in low-risk women and associated perinatal outcomes. (2012) Am J Obstet Gynecol 207(6): 502.e1– 502.e8.
- 12. Hannah, M.E., Hannah, W.J, Hellmann, J., et al. Induction of labor as compared with serial antenatal Monitoring in Post –term pregnancy. A randomized controlled trail. The Canadian multicenter post- term pregnancy trail group. (1992) N Engl J Med 326(24): 1587- 1592.
- 13. A clinical trial of induction of labor versus expectant management in postterm pregnancy. The National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. (1994) Am J Obstet Gynecol 170(3): 716- 723.