Comparison in Mandibular Movements Between Subjects with Deep Bite and Normal Occlusion
Pao-Chieh Lee, Heng-Li Huang, Yu-Fen Li
Affiliation
- 1School of Dentistry, College of Medicine, China Medical University, Taichung, Taiwan, R.O.C
- 2School of Dentistry, College of Medicine, China Medical University, Taichung, Taiwan, R.O.C
- 3Department of Dentistry, China Medical University Hospital, Taichung, Taiwan, R.O.C
- 4School of Dentistry, College of Medicine, China Medical University, Taichung, Taiwan, R.O.C
- 5Department of Public Health, College of Public Health, China Medical University, Taichung, Taiwan, R.O.C
Corresponding Author
Jian-Hong, Yu, Dean of Orthodontics, Department of Dentistry, China Medical University Hospital, Taichung, Taiwan, Republic of China. Tel: +886-4-22053366 # 2315; Fax: +886-4-2230-4333; E-mail: kenkoyu@mail.cmu.edu.tw
Citation
Jian-Hong, Yu. et al. Comparison in Mandibular Movements between Subjects with Deep Bite and Normal Occlusion. (2015) J Dent & Oral Care 1(1): 1- 9.
Copy rights
©2015 Jian-Hong Yu. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Dental casts; Mandibular Movements; Deep Bite; Normal Occlusion
Abstract
Introduction: Orthodontic treatment in-deep bite subjects has generally been focused on the correction of excessive vertical coverage (overbite); however, the impact on functional problems following treatment has not been well evaluated. This study aimed to investigate the differences in mandibular movements between deep bite and normal occlusion, and to compare the functional changes of mandible in the subjects with deep bite before and after treatment.
Methods: This study included students from School of Dentistry, China Medical University (CMU), and employees from CMU Hospital. The participants were categorized into normal bite (n = 11) and deep bite (n = 16) groups. Considering the clinical practicability, convenience and affordability, Digi Gnatho software (Japan), was used to analyze mandibular movements recorded by digital video camera.
Results: No significant difference was observed in the left side masticatory movements between two groups. Significant difference was only detected in the horizontal direction of right side mastication. All of the velocities and masticatory cycle duration of both sides showed no difference. In the mandibular border movements, protrusive movements in deep-bite group were distinct from normal occlusion group. Normal occlusion group had a larger range of mandibular movements compared to deep bite group.
Conclusions: Different degrees of vertical coverage of the incisors not only presented differences in the ranges of masticatory movements and border movements, but also had an impact on the final occlusal phase of mastication.
Introduction
Dental arch forms can be evaluated by using dental casts, static two-dimensional (2D) and three-dimensional (3D) techniques, such as intraoral, facial photographs, cephalometric radiography and panoramic radiography, and 3D computer tomography. However, static images and dental casts provide only limited information about occlusal function and temporo mandibular joint (TMJ) movements. More evaluations are necessary to determine mandibular movements, biting forces, food breakdown or food processing capacities of mastication. Various methods for the assessment of TMJ movements or occlusal functions have been proposed by many scientists. Of which, assessments of chewing performance and chewing efficiency are related to the occlusal contact area of teeth. Jankelson et al. in 1975[1] suggested that the functions of chewing system can be evaluated by mandibular movement trajectories, such as changes in mandibular displacement and velocity observed during chewing. This method has been widely used for analyzing the masticatory system function by many scientists[2,3]. Furthermore, studies also reported the relationship between occlusal patterns and masticatory system functions[2,3]. However, further studies are warranted to clarify the effects of occlusal pattern on masticatory and TMJ movements, as well as the interactions between each other. Previous studies have reported that deep bite can contribute to gingival trauma[4], periodontal destruction, severe attrition of the front teeth, and may serve as a cofactor accounting for temporo mandibular disorder[5]. Another study also indicated that maxillary incisors with a more upright position could result in a limited motion of mandibular condyle head, and consequently caused abnormal movements of mandible[6]. However, the other studies suggested that deep bite was not significantly associated with condylar position[7], or caused TMJ disorders[8].
Other than causing dental trauma and damaging malocclusion, whether deep bite can lead to mandibular deficiency remain unclear. The findings related to cross bite and open bite were described in most of previous studies investigating the relationships between malocculsion and mandibular movements. To our knowledge, only few literatures involving deep bite and masticatory movements provided with limited information. Excessive overbite was reported to be a significant factor causing vertical masticatory patterns, such as chopping pattern[9]. However, other studies considered that lateral collisions in mandibule occurred more frequently during chewing, but vertical collisions were relatively rare[10]. In addition to the masticatory movements observed in deep bite, Alexander et al.[11] compared the mandibular movements and border movements in 5 patients with a deep bite malocclusion and found no significant difference in smoothness and regularity before and after orthodontic treatment. In recent years, Buschang et al.[3] indicated that deep bit contributed to more anterior and posterior displacements in the masticatory path during mouth opening and a lower velocity during mouth closing.
Deep bite is commonly considered to be one of malocclusions in clinical practice. A greater vertical coverage of the front teeth can affect the range and path of mandibular movements and is more likely to lead to interference or a steeper movement path. Due to the limitations of oral anatomy, maxillary anterior teeth almost cover the entire mandibular front teeth in the condition of deep bite, where the teeth are in the centric occlusion, so that teeth hard tissues were rarely used as reference points in the studies investigating mandibular movements in deep bite. However, the use of hard tissue as markers can not only provide a more faithful representation for mandibular movements, but is also more practical for clinicians. Therefore, accuracy in tracking movement, ease of use, availability, and affordability are important factors for treating patients with deep bite.
Based on the considerations mentioned above and experiences reported in previous literatures, this study applied an optical tracking device and used mandibular incisors as tracking reference markers to break through the barriers in previous work. We aimed to compare the differences in mandibular movements between patients with deep bite and normal bite, to provide the parameters associated with masticatory cycles, patterns and mandibular movements for objectively comparing the differences between deep bite and normal deep bite, and to provide a better understanding about deep bite for contributing to clinical practice improvement.
Materials and Methods
Subjects
This study included students from School of Dentistry, China Medical University (CMU), and employees from CMU Hospital. A total of 27 subjects aged 21-35 years were categorized into two groups. The normal bite group (NB or control group) consisted of 11 subjects with an average age of 23.9 ± 3.0 years and 16 subjects with deep bite (DB group) with a mean age of 26.6 ± 5.0 years.
The inclusion criteria for subjects with normal bite were as the follows: (1) occlusal teeth contacts in centric occlusion and diagnosed as having Angle class I malocclusions of the first molars, (2) centric occlusion, but without open bite, deep bite, cross bite, or any obvious malocclusion, (3) with intact permanent teeth, no missing teeth except the third molars, no unfilled cavity in any tooth, without obvious periodontitis or fixed partial denture, (4) without significant TMJ disorders, no present pain in masticatory muscles or past medical history, (5) no systematic disease, endocrine disorders or history of allergies, and (6) no craniofacial skeletal abnormality in the (facial) appearance.
As deep bite is commonly related to Angle class I and Angle class II occlusions of the first molars, we defined the inclusion criteria for deep bite malocclusion as follows: (1) deep bite with the teeth contacts in centric occlusions and diagnosed as having Angle class I and Angle class II malocclusions of the first molars, (2) centric occlusion was accompanied by a deep bite between the maxillary and mandibular incisors, and the length of vertical coverage was 50% greater than the clinical crown length, (3) other criteria were the same as for control group described in (3) – (6). Among the 16 subjects with deep bite, 10 were Angle class I and 6 were class II.
Prior to initiating this study, the study protocol was reviewed and approved by the Institutional Review Board of China Medical University & Hospital (project number: CMUH103-REC3- 045). After all subjects were trained to have understanding about mandibular movements and specific precautions, they provided the informed consent before participated in this study.
Mandibular Movements
Border movements of the mandible and chewing movements were conducted in all subjects sitting in a chair without a headrest in order to allow the head to reflex naturally. Before testing, all subjects were firstly taught to sit with a natural resting posture in the chair and the front side of forehead facing the camera. To observe the position and motion of head, the subjects were arranged into appropriate position without their heads up or down. The videos of mandibular movements were taken only after the subjects understood and were familiar with the testing procedures.
Masticatory movements were tested by using the commercially available chewing gums with length, width, and thickness of 22.2 mm, 10.9 mm, and 6.0 mm, and a weight of about 1.5g, respectively. Before each masticatory movement, chewing gums were placed on the back of the tongue in all subjects with their teeth in centric occlusion. They were then asked to complete masticatory movements within a specified time. Two types of masticatory movements were conducted: chewing a piece of defined soft chewing gum on the left side (LS) and right side (RS), and 30 seconds were recorded for each side.
For mandibular border movements, the subjects performed 4 types of movements, including maximum mouth opening and closing, left-side border movements, right-side border movement, and protrusive border movement. The start and end points were always in centric occlusion for each mouth opening and closing cycle. To avoid errors as a consequence of muscle exhaustion, 11 subjects performed each movement for 10 times and had sufficient rest intervals between each independent type of movement.
Tracking Device
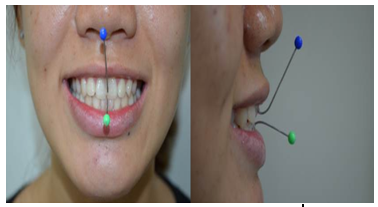
In this study, the maxillary central incisor was used as a reference point on the moving path during mandibular movements and the mandibular central incisor was the reference point for maxillary movements (Figure 1). Stainless steel straight arch wire for dental orthodontic use, incisors, and ball hooks were connected by adhesive (4-META / MMA-TBB system, Sun Medical Company, Kyoto, Japan). For deep bite with an overbite, the buccal surfaces of mandibular premolars or molars were used to adhere the stainless steel wire that a crossed the lower lip and passed through the mandibular central incisor below the forehead, in order to ensure no occlusal interference.
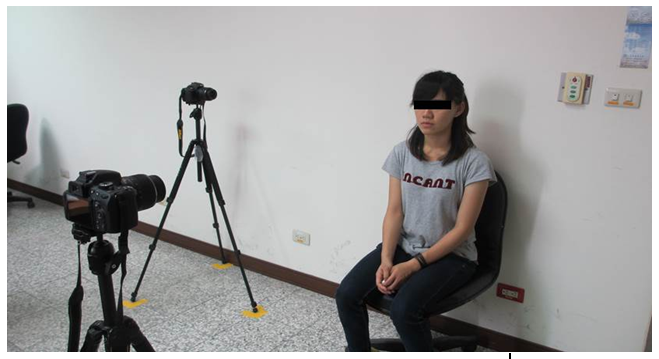
Mandibular movements were recorded by a video camera (NIKON D5100) used at the dental outpatient clinics. Two videos cameras were placed in the frontal and sagittal planes, and set with a linear distance of 1.2 m from the subjects. The fixed angle was 90º between the two cameras (Figure 2). Recording was conducted using autofocus to capture images up to 1920*1080 pixels at a full 30fps. The average pixel sizes for frontal and sagittal planes were 0.26 ± 0.02 mm and 0.27 ± 0.01 mm, respectively.
Analysis of Movement Paths and Patterns
Analysis of images of movement paths and patterns was conducted using the software, Digi Gnatho (Ver 1.3, Rise Corporation, SENDAI, JAPAN). This software enabled us to divide the cycling path into 20 sections/segments based on the vertical distance. The positions of centric occlusion and maximum vertical distance were defined as the 0 (original) and the 10th points, giving a total of 20 points for a cycle. Of which, 10 sections were included in each of the mouth opening and closing paths. All of the coordinates, vertical distance, average velocity and standard deviation, the average velocity and the average duration taken to complete a single cycle and the entire movement process can be obtained by using this software to calculate automatically.
Table 1: Frontal view of chewing gum
| Left side | Difference | Right side | Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deep bite | Control | Deep bite | Control | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Horizontal position at the maximum mouth opening (mm) | 3.73 | 1.92 | 3.32 | 2.17 | ns | -3.1 | 2.6 | -3.99 | 2.52 | ns |
| Vertical position at the maximum mouth opening (mm) (vertical amplitude of masticatory cycle) | 18.89 | 4.02 | 20.12 | 4.21 | ns | 19.45 | 5.77 | 22.17 | 4.47 | ns |
| The most anterior horizontal position in the mouth opening path (mm) | 0.12 | 1.51 | -0.3 | 2.61 | ns | 0.3 | 1.27 | 0.65 | 1.47 | ns |
| The most anterior vertical position in the mouth opening path (mm) | 2.23 | 4.29 | 6.43 | 6.66 | ns | 4.52 | 6.02 | 5.27 | 6.9 | ns |
| The most posterior horizontal position in the mouth closing path (mm) | 4.32 | 2.22 | 4.46 | 3.04 | ns | -4.21 | 2.53 | -6 | 2.52 | ns |
| The most posterior vertical position in mouth closing path (mm) | 13.87 | 5.37 | 11.65 | 6.59 | ns | 13.28 | 6.21 | 15.6 | 7.01 | ns |
| Horizontal amplitude between the most anterior and most posterior positions in mouth opening and closing paths | 5.65 | 3.65 | 6.17 | 3.45 | ns | 4.95 | 2.3 | 7.11 | 2.23 | * |
| Maximal velocity of the mouth opening path (mm/s) | 101.87 | 31.97 | 113.72 | 45.99 | ns | 105.98 | 36.03 | 128.46 | 45.17 | ns |
| Vertical position at the maximum velocity in the mouth opening path (mm) | 11.54 | 3.01 | 12.6 | 2.9 | ns | 11.59 | 4.1 | 13.79 | 2.63 | ns |
| Maximum velocity of the mouth closing path (mm/s) | 127.3 | 36.58 | 138.44 | 43.41 | ns | 131.37 | 44.34 | 155.39 | 52.96 | ns |
| Vertical position at maximal velocity in the mouth closing path (mm) | 7.21 | 2.11 | 6.7 | 2.46 | ns | 7.62 | 2.81 | 7.99 | 3 | ns |
| Average duration of masticatory cycle (sec) | 0.82 | 0.11 | 0.8 | 0.16 | ns | 0.82 | 0.12 | 0.8 | 0.16 | ns |
| Average velocity of masticatory cycle (mm/s) | 44.42 | 10.66 | 48.96 | 12.89 | ns | 45.2 | 13.37 | 54.11 | 12.87 | ns |
ns, not significant; * P < 0.05
Table 2: Sagittal view of chewing gum
| Left side | Difference | Right side | Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deep bite | Control | Deep bite | Control | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Horizontal position at the maximum mouth opening (mm) | -3.88 | 3.37 | -4.35 | 3.53 | ns | -3.95 | 3.27 | -4.39 | 3.1 | ns |
| Vertical position at the maximum mouth opening (mm) (vertical amplitude of masticatory cycle) | 20.61 | 3.97 | 21.15 | 4.11 | ns | 20.74 | 5.76 | 23.03 | 4.03 | ns |
| The most anterior horizontal position in the mouth opening path (mm) | 0.22 | 0.53 | 0.46 | 0.43 | ns | -0.1 | 0.84 | 0.58 | 0.54 | * |
| The most anterior vertical position in the mouth opening path (mm) | 3.23 | 5.74 | 2.13 | 1.61 | ns | 3.77 | 7.07 | 2.01 | 1.41 | ns |
| The most posterior horizontal position in the mouth closing path (mm) | -3.9 | 3.22 | -4.4 | 3.47 | ns | -3.68 | 3.53 | -4.43 | 3.08 | ns |
| The most posterior vertical position in mouth closing path (mm) | 16.14 | 8.01 | 20.48 | 4.13 | ns | 17.96 | 8.48 | 22.43 | 4.38 | ns |
| Horizontal amplitude between the most anterior and most posterior positions in mouth opening and closing paths | 4.27 | 2.85 | 4.86 | 3.2 | ns | 4.19 | 3.07 | 5.01 | 2.75 | ns |
| Maximal velocity of the mouth opening path (mm/s) | 108.55 | 30.29 | 119.71 | 46.07 | ns | 110.77 | 35.35 | 133.54 | 46.85 | ns |
| Vertical position at the maximum velocity in the mouth opening path (mm) | 12.6 | 3.23 | 13.44 | 2.62 | ns | 13.07 | 4.22 | 14.19 | 2.27 | ns |
| Maximum velocity of the mouth closing path (mm/s) | 142.31 | 44.63 | 146.24 | 48.4 | ns | 137.17 | 47.13 | 166.4 | 54.78 | ns |
| Vertical position at maximal velocity in the mouth closing path (mm) | 7.64 | 2.48 | 7.72 | 2.22 | ns | 8.19 | 3.6 | 8.98 | 2.8 | ns |
| Average duration of masticatory cycle (sec) | 0.81 | 0.09 | 0.8 | 0.17 | ns | 0.83 | 0.12 | 0.79 | 0.16 | ns |
| Average velocity of masticatory cycle (mm/s) | 48.53 | 10.02 | 52.17 | 15.29 | ns | 48.07 | 13.62 | 56.94 | 13.67 | ns |
ns, not significant; * P < 0.05
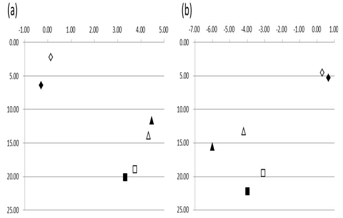
Figure 3: Frontal views of the average border movements of chewing patterns. (a) Left side chewing; (b) Right side chewing
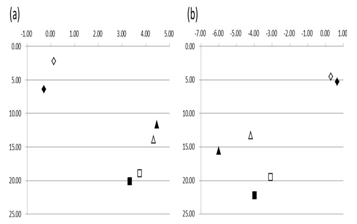
Figure 4: Sagittal view of the average border movements of chewing patterns (a) Left side chewing; (b) Right side chewing
The most anterior position in the mouth opening path; The position at the maximum mouth opening; The most posterior position in the mouth closing path. Symbols: unfilled square, deep bite group; Black Square, control group. Unit, in mm.
As shown in Figure 5 and Figure 6, the average masticatory patterns are presented by superimposing all cycles of mastication. The mouth opening and closing paths near to centric occlusion were more cnetralized in deep bite group compared to the control group.
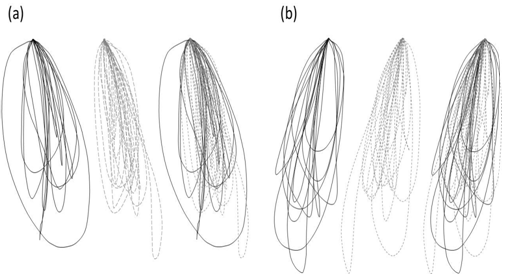
Figure 5: Frontal views of the average masticatory patterns presented by superimposing all cycles of mastication. Black line, control group; dash line, deep bite group. (a) Left side chewing; (b) Right side chewing
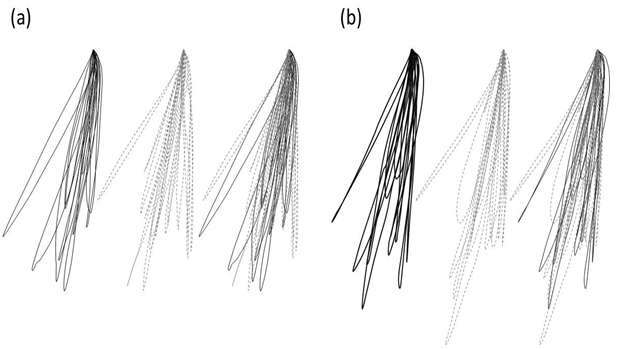
Figure 6: Sagittal views of the average masticatory patterns presented by superimposing all cycles of mastication. Black line, control group; dash line, deep bite group. (a) Left side chewing; (b) Right side chewing
In Table 3, the deep bite group had a smaller range of motion in mandibular border movements compared with the control group. No difference was detected in three parameters, including the maximum vertical range of motion of mandibular border movements during mouth opening in the frontal plane, the maximum horizontal range of motion of left side border movements, and the maximum horizontal range of motion of right side border movements. However, a significant difference was shown in the horizontal displacement between the anterior and posterior positions in mandibular protrusion movements.
Table 3: Sagittal view of chewing gum.
| Deep bite | Control | Difference | |||
| Mean | SD | Mean | SD | ||
| Frontal plane- the maximum vertical range of motion of mandibular border movements during mouth opening (mm) | 68.74 | 10.35 | 77.57 | 10.44 | ns |
|---|---|---|---|---|---|
| Frontal plane- the maximum horizontal range of motion of left side mandibular border movements (mm) | 12.16 | 3.01 | 13.07 | 1.84 | ns |
| Frontal plane- the maximum horizontal range of motion of right side mandibular border movements (mm) | 11.79 | 3.44 | 12.68 | 1.52 | ns |
| Sagittal plane- the maximum horizontal displacement between the anterior and posterior positions in the mandibular protrusion movements (mm) | 9.13 | 2.58 | 11.89 | 2.33 | * |
SD, standard deviation; ns, not significant; *P < 0.05
Discussion
Head Movement during Mandibular Movements
According to the study by Zafar et al.[12], a functional mandibular movement should include concomitant and coordinated head and mandibular movements. Mandibular movements are the result of jaw and neck muscle actions that pull TMJ, atlanto- occipital joint, and cervical spine joints. These muscle motor programs are innate, and the head posture affects the direction and stability of the mandibular opening movements[13]. Matsubara et al[14] also indicated that the head is naturally positioned backwards and downwards to prepare the action for starting an occlusal phase. This movement may occur before or simultaneously with the beginning of the occlusion. Head movements are evoked during mastication in order to achieve effective destruction of a food bolus. The average head movement velocities vary, depending on the hardness or softness of different foods. Comparing with soft food, hard food is associated with a faster head movement velocity.
Because the design and precision of available devices, fixed head designs were used in previous studies on mandibular movement's[15]; however, fixed head may restrict the natural movement of the mandible. Some scientists suggested that optical tracking systems could achieve satisfied precision, excellent reproducibility, a minimum of external interference to study subjects, and provide head movement elimination or compensation algorithms to ensure high accuracy[16]. In this study, therefore, to ensure a physiological and coordinated head motion during mandibular movements, we used an optical tracking system without fixing the head.
Differences in the References Points between Hard and Soft Tissues
Henrik son[17] noted that the reference points on soft skin tissue might appear self-movements in response to mandibular movements. Therefore, using soft tissue to record mandibular movements is more likely to result in experimental deviations, in addition to some measurement limitations[18]. The reliability of results only dependents upon the availability of compensation algorithms of the recording device. Furthermore, there are consistency and similarity between chin skin and mandibular movements, only the duration of masticatory cycle can be evaluated by the chin skin movements[19].
The reference points on teeth cause less concerns over the self-movement and can represent the movements of hard mandibular tissue. However, oral piercing devices may affect the feedback and reflection of oral peripheral receptors, such as the jaw bone, oral mucosa, periodontal ligaments, joints, muscles, and skin[20], and result in unnatural mandibular movements. In addition, oral piercing devices may cause compression on the lips and lead to slightly inaccurate mandibular movements[17]. Therefore, studies have suggested to replace oral piercing device with the reference frames[21]. For which, frontonosal reference points, with the most less movement among reference points on soft tissue, are the most favorable to be used for replacing the locations with oral piercing device to position markers and to observe mandibular movements in patients with TMJ disorders[22]. The advances in the resolution and precision techniques in conebeam computed tomography (CBCT) have gradually enhanced the use of CBCT in studies involving mandibular movements. Without the need of any reference mark, the performance of hard tissue movements can be directly observed through radiography. Chen et al.[23] observed 3D mandibular movements by using a CBCT and found that this approach enabled TMJ to perform complex functions and provide a complete description of the rigid-body mandibular motion. They suggested that more practical references would be required while using CBCT to evaluate 3D mandibular movements, and the use of radiation doses also need to be carefully considered.
Masticatory Movements
Mandibular movements during mastication are produced by a central pattern generator (CPG). In the review by Nakamura et al.[24], CPG is responsible for the coordination of peripheral sensory feedback during mastication and consequent regulation on masticatory movements. They also referred three components work interactively during mastication. First, chewing rhythm or cycle length; second, the movement patterns of jaw bone muscles, tongue and facial muscles in chewing process; and third, the coordination of these muscles. Thus, CPG not only produce actions by following the central nervous system, but also regulate masticatory movements according to the feedback of three components of mastication.
Consistent with previous studies[3], our findings revealed no significant difference in the parameters between deep bite and normal occlusion. However, we found significant differences in horizontal amplitude of the lateral positions in the frontal plane during right side chewing, as well as the most anterior position of mouth opening path in the sagittal plane. Some factors might be associated with the different results, such as sample numbers, the location of reference points, tracking devices, software, and statistical analysis methods, as shown in Table 4.
Table 4: Comparison with a previous study.
| Sample no. | Reference point | Tracking device | Software | Statistical method | Results with significant differences | |
|---|---|---|---|---|---|---|
| This study | Control-11 Deep bite-16 | Teeth | Digital camera | DigiGnatho V1.3 | Wilcoxon rank-sum test | Right-side chewing mastication -Horizontal amplitude in the frontal plane -Sagittal plane The most anterior position in mouth opening path |
| Buschang et al. | Control-24 Deep bite-23 | Chin Skin | Optoelectric jaw tracking system | multilevel statistical models | Vertical displacement Posterior displacement The maximum vertical velocity |
From the enclosed ranges of four border positions at each phase of masticatory cycle, including the position of centric occlusion, the most lateral position in mouth opening path, the position of maximum mouth opening, and the most lateral position in mouth closing path, we clearly observed a larger range of movement in control group compared with deep-bite group.
According to the Ogawa's study[25] that investigated masticatory movement in frontal plane in subjects with normal occlusion, the subjects could be categorized into vertical and lateral types based on the angles of mouth closing paths during mastication. They found increases in the angle of anterior guidance resulted in a more vertical mouth closing path, an increase in the average duration of masticatory cycle, and a slower velocity of the maximum mouth closing in the group with lateral type. However, no significant difference was observed between the two groups. Ogawa[25] suggested that the possible mechanism associated with mandibular movements after alterations in occlusal guidance, including a narrower mouth closing path, an increased duration of mouth closing, a lower velocity of mouth closing, and an overall increased duration of masticatory cycle. The results of our study also indicated that deep bite group was more likely to have a narrower chewing pattern in the frontal plane. The findings of a longer average duration of masticatory cycle and a slower of maximum mouth closing velocity in deep bite group were similar with the results of lateral chewing movements observed by Ogawa et al.[25]. Based on their results, we found that the subjects with deep bite might have exerted an effort to avoid steeper angles of incisors and a larger overbite, which resulted in a narrower range of mandibular movements during mastication, a slower mouth closing velocity, and a longer average duration of masticatory cycle.
Throckmorton[26] indicated that some chewing patterns existed since the deciduous dentition period and were difficult to be corrected even after orthodontic treatment, due to the consequent effects on the development of CPG and chewing patterns in permanent dentition. According to the hypothesis of Throckmorton et al., for the subjects with deep bite in the process of growth and development, the angle of mouth closing path during mastication would gradually adjust to the guidance of current (permanent) incisors, consequently affect the development of CPG and then become a natural rhythm of masticatory movement. The masticatory muscles also adapt to the current occlusal status; therefore, no difference can be detected between the two groups as shown in our results.
Foods with different physical properties can affect masticatory movements[27], including the average duration of a masticatory cycle, the number of masticatory cycles (chewing frequency), and muscle contraction patterns during mastication. According to the study by Gillings et al.[28] the duration of a chewing cycle was approximately 0.82 second, ranging from 0.59 to 1.13 seconds. Jemt[29] reported 0.76 - 1.12 seconds of a masticatory cycle. Buschang[3] indicated that the average duration of masticatory cycle was 0.85 second for deep-bite group and 0.87 second for control group. In our study, we found the average duration of a masticatory cycle ranged from 0.79 to 0.83 seconds, which was in line with the results of Jemt and Gillings, and also similar with Buschang's findings that reported an average duration of 0.79- 0.80 seconds for control group and 0.81- 0.83 seconds for deep bite group. While entering and leaving the occlusal contacts in dentition, the mandible in subjects with deep bite must adapt to maxillary dentition or avoid occlusal interference, which may account for the differences in the duration of masticatory cycle between two groups.
Our results indicated that the maximum velocities of mouth closing paths in two groups were greater than that of mouth opening paths. In a previous study investigating the effects of masticating chewing gum by Ogawa [25], the maximum velocities of mouth opening and closing were consistent with our results. However, opposite results were obtained from other studies exploring masticatory movements for different foods, such as the chewing paraffin blocks[30]. We speculated the differences were caused by different physical properties of foods (soft or hard). Because the duration of mouth closing is longer than opening while chewing hard food. In contrast with chewing soft food, the velocity of mouth closing was greater than that of mouth opening[31].
Masticatory Patterns
In the frontal view, the masticatory pattern during right-side mastication, the 8th subject in deep bite group and the 10th subject with normal occlusion had a reverse-sequencing pattern. Whereas, in the frontal view of the right-side masticatory pattern, the pattern of the 8th subject in deep bite group, as well as the 4th and 10th subjects in normal occlusion group were reversed, indicating that our findings were inconsistent with previous studies[32,33]. However, Piancino et al.[34] also showed a reverse-sequencing chewing pattern in control group (normal occlusion). In which, 3% of subjects presented right side mastication while chewing gum and 9% subjects were left side. We found that the subjects showing either right side or left site mastication accounted for 6% in the deep bite group, 9% of subjects with normal occlusion presented right side mastication, and 18% subjects were left side. The higher rates shown in our study were likely to be a result of a smaller sample size; however, a higher rate of left side than right side mastication was noticeable. Furthermore, Piancino[34] indicated that the reverse-sequencing pattern was often associated with posterior cross bites, they also concurred that orthodontic treatment could result in a reduction in reverse-sequencing chewing pattern. However, Throckmorton[26] did not reveal similar findings.
From the perspective of average masticatory patterns presented by superimposing all cycles of mastication, the frontal plane showed the path near to central occlusion was narrower in deep bite group compared to control group; whereas, the sagittal plane revealed the mouth opening path near to central occlusion was at more anterior position in control group. A previous study indicated that masticatory movements could be affected by the anterior or posterior parameters, and were particularly more significant in the frontal plane[35]. Our results indicated the dentition in deep bite was affected not only in the frontal plane but also the sagittal plane. In other words, the masticatory path near to CO was more vertical, and with lesser lateral movements in deep bite group, indicating that the range of masticatory movements during final stage of occlusion was affected by incisors. The most significant factor influencing the masticatory performance was the occurrence of grinding motion in the masticatory path while entering and leaving the CO position[36]. According to the observation on subjects with normal dentition by Ehrlich et al. [37], the masticatory movements were guided by the incisors into intercostal position in some subjects during mastication. The occlusal surfaces of the first molar also showed less wear on these subjects, suggesting that masticatory pattern guided by the incisors had a less ability to breakdown foods. In Kobayashi's study[38] investigate two masticatory patterns in normal occlusion, the first type was the mouth closing path entered into the occlusal surface from a more horizontal direction, and by a more vertical direction was the second type. The also indicated that the first type presented significantly more active masticatory muscles and a higher masticatory efficiency. More studies may be necessary to explore whether the effects of vertical overbite and the angle of the incisors during mastication in the deep bite subjects resulted in lesser lateral movements while entering or leaving the OC position, and consequently led to a lower efficiency in breaking down foods or chewing performance than the normal occlusion group.
For the subjects with normal occlusion, the masticatory pattern in the sagittal plane showed that the mouth closing path was posterior to the opening path, and was in more regular pattern[39]. However, in contrast to the findings by Gibbs et al.[40], the masticatory patterns of some subjects were partial or entire mouth closing path posterior to the opening path. Our results were more consistent with the findings of Gibbs et al., showing that the mouth closing paths were more or less posterior to the opening path in both deep bite and normal occlusion groups, and some subjects even involved continuous alternating masticatory patterns.
Therefore, according to the report of a literature review[36], each individual has a unique masticatory pattern that was controlled by the central nervous system. The pattern can also be affected by the teeth, occlusion, and the anatomical patterns of TMJ. Most importantly, only the grinding motion produced during leaving and entering the maximum occulsal contact position in masticatory cycle present a greater ability to facilitate the breakdown of foods.
Border Movements
Mandibular order movement is a less common functional movement in daily life; however, it has been often used to examine the range of TMJ motion or treatment outcomes in clinical practice. We found a smaller range of TMJ motion in the frontal plane in deep bite group compared with control group, despite the difference was significant. However, in the sagittal plane, the deep bite group had a significantly decreased horizontal motion between anterior and posterior positions in mandibular protrusion, the effects of incisors guided movements on mandibular protrusion were also significantly noticeable, as shown in Figure 7. The results of previous studies also suggested that the degree of coverage of the incisors significantly affected mandibular protrusion and lateral movements[41]. In comparing to the condylar guide, the incisors guide possessed a more significant impact on the movements of mandibular protrusion[42].
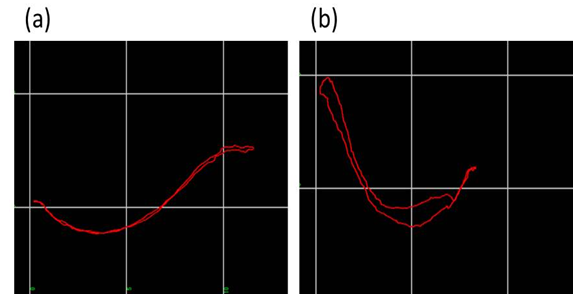
Figure 7: Sagittal view of movements of mandibular protrusion (a) Control group; (b) Deep bite group
Two movements, rotation and displacement of the condylar head, should be included in the process of mandibular movements in normal occlusion. According to Thompson et al.[43], in the case of a very steep angle of front teeth guide, when the mandible come into contact with the front teeth guide for movements, such as mandibular protrusive movements, a more vertical degree of front teeth guide will limit the displacement of condylar head. And, in contrast, more rotary hub openings can be produced by the condylar head, which is an abnormal movements of condylar head, or prone to causing TMJ disorders.
Other than the factors mentioned above, another factor may be associated with mandibular muscles. Because deep bite subjects usually have a steeper angle of front teeth, so that the mandible must continue to move forward under the condition of steeper angle, which will probably fatigue the muscles that control protrusive movements. Moreover, for the deep bite subjects in the process of mandibular protrusion, the protrusive muscles are under greater tension while passing through a front teeth guide with steep angle. Forward movement from horizontal extension may cause a less horizontal motion. In addition to muscle fatigue and tension, another possible factor is the fixed elongation of muscle controlling protrusive movements. After a greater vertical movement, only a limited horizontal motion is available to be used in the following movements. Overall, a preliminary interpretations for the results of the current study are summarized as above.
Limitations
Head movements of study subjects were relatively uncontrollable. There were always some differences in the angles in head and body among individuals despite. The subjects were asked to sit in the same position as much as possible, and with their eyes levelled with the camera positioned in front of them. Although a literature 44 documented the use of the external auditory canal rod could reduce head movements and result in more accurate and higher repeatable mandibular movements; however, natural mandibular movements are affected by restricted movement of the head. Therefore, this study allowed the subject head to freely move in order to reduce the number of factors affecting masticatory movements.
For the feasibility in clinical practice and to faithfully present mandibular movements, we used an intraoral device to adhere teeth. However, as described in previous literatures, although a dental adhesive device could more faithfully present the mandibular movements, it also produced a more or less compression on the lips during mastication, affected the feedback reflection of peripheral receptors around the oral activity, and consequently, interfered the control of central nervous system on masticatory movements. Moreover, this study applied a single reference point for describing mandibular movements was for the ease of understanding and clinical significance; however, a single reference point might be insufficient for a detailed description of mandibular rigid-body motion.
An image frequency of 30 fps was used in this study; however, the fastest mastication in subjects was about 1.7 seconds per masticatory cycle, errors might have been produced, despite the speed was still within the capacity of camera used.
A small sample size of this study was one of the major limitations. More samples will be included in the future study following this one, so that the trend can be more evident. More categories of study subjects can be made, such as skeletal or dental deep bite. Other factors should also be taken into consideration, such as the angle of the incisors, canine guided and molars guided occlusions, the angle of mouth closing path during mastication, the angle of occlusal plane, and occlusal contact guided by the incisors during mastication, the depth of curve of Spee, are all the important parameters warrant further investigation.
Conclusion
1. Comparing with the group with normal occlusion, no significant difference in masticatory movements was detected in the deep bite; however, a slightly lower performance was observed.
2. In the chewing pattern during masticatory cycle, the deep bite group appeared a more centralized masticatory path and less lateral movements in the horizontal direction.
3. The protrusive border movements in deep bite group were significantly affected by the incisor guide and result in a smaller moving motion in horizontal direction than normal occlusion group.
4. Mandibular movements in the final stage of occlusion were affected by dentition patterns and the degree of vertical coverage of the incisors.
Acknowledgement: This work was supported by grant DMR- 98-112 to JH Yu.
References
- 1. Jankelson, B., Swain, C., Crane, P., et al. Kinesiometric instrumentation: a new technology. (1975) JADA 90(4): 834- 840.
- 2. Neto, G. P., Puppin-Rontani, R. M., Garcia, R. Changes in the masticatory cycle after treatment of posterior crossbite in children aged 4 to 5 years. (2007) AJO-DO 131(4): 464- 472.
- 3. Buschang, P. H., Throckmorton, G. S., Austin D, et al. Chewing cycle kinematics of subjects with deepbite malocclusion. ( 2007) AJO-DO 131(5): 627- 634.
- 4. Proffit, W. R., Fields Jr, H. W., Sarver, D. M. Contemporary orthodontics: 4th edn. (2006) J Den Edu 751.
- 5. Nanda, R. The differential diagnosis and treatment of excessive overbite. (1981) Dent Clin North Am 25(1): 69- 84.
- 6. Thompson, J. R. Abnormal Function of the Temporomandibular Joints and Related Musculature: Orthodontic Implications. Part II (1986) Angle Orthod 56(3): 181- 92.
- 7. Gianelly, A. A., Petras, J. C., Boffa, J. Condylar position and Class and Class II deep-bite, no-overjet malocclusions. (1989) Am J Orthod Dentofacial Orthop 96(5): 428- 432.
- 8. Seligman, D. A., Pullinger, A. G. The role of functional occlusal relationships in temporomandibular disorders: a review. (1991) J craniomandib Disord 5(4): 265- 279.
- 9. Granger, E. R. The establishment of occlusion. (1960) Dent Clin North Am 527- 39.
- 10. Sheppard, I. M. The effect of extreme vertical overlap on masticatory strokes. (1965) J prosthc dent 15(6): 1035- 1042.
- 11. <a href="http://www.ajodo.org/article/0002-9416%2884%2990119-2/abstract" t