Complications in Pregnancy and Obstetrical Outcome in Some Patients with Endometriosis
Deenadayal, A, Alkatout, I
Affiliation
Department of Obstetrics and Gynecology, University Clinics of Schleswig-Holstein, Kiel, Germany.
Corresponding Author
Mettler, L. et al. Department of Obstetrics and Gynecology, University Medical Center Schleswig-Holstein, Campus Kiel, Arnold-Heller-Str. 3, House 24, 24105 Kiel, Germany; Fax: 49 431 5703407; E-mail: lmettler@email.uni-kiel.de
Citation
Mettler, L. et al. Complications in pregnancy and obstetrical outcome in some patients with endometriosis (2015) J Gynecol Neonatal Biol 1(1): 1-3
Copy rights
©2015 Mettler, L. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License.
Keywords
Caesarean sections; Endometriosis; Placental complications; NK cell behavior; Obstetrical emergencies
Abstract
In this paper we consider the relation of pregnancy and endometriosis with the following conclusions:
1. Increased risk for premature deliveries and pregnancy complications,
2. More frequent pre-eclampsia and antepartum hemorrhage,
3. Increased rate of Caesarean sections,
4. Severe pain in pregnancy continues in quite a few patients,
5. Obstetricians should be aware of obstetric emergencies, such as direct bleeding from lesions, bleeding from uterine arteries or veins, interruption of ureter and severe peritoneal decidualized endometriosis.
Introduction
As a disease affecting an estimated 176 million females of reproductive age worldwide endometriosis is considered the second most common benign female genital disease after uterine myomas[1]. It has been defined as the presence of endometrial glands and stroma outside the internal epithelial lining of the uterine cavity. Endometrial implants are typically situated in the pelvis (genital endometriosis) but can occur anywhere (extragenital endometriosis) (Figure 1). (Figure 2) reveals the histopathological picture of an endoscopic lesion.
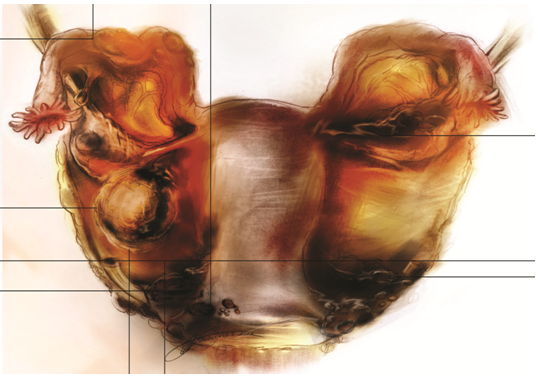
Figure 1: Overview of the typical locations of endometriosis genitalisexterna. Implants can be raised flame-like patches, whitish opacifications, yellow-brown discolorations, translucent blebs, or reddish irregularly shaped spots.
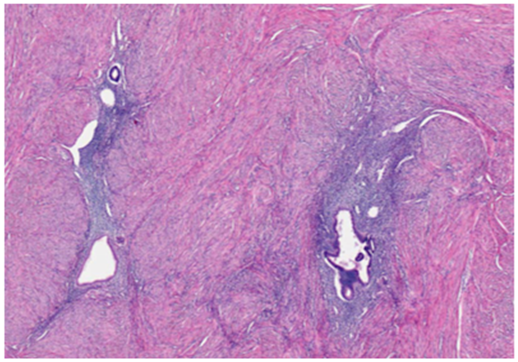
Figure 2: Haematoxilin Eosin (HE staining, EEC stage II) section of an endometriotic lesion on cycle day 10 showing endometriosis in the fibro-muscular stroma and an unspecific chronic fibrotic infectious reaction with some blood residuals. The subepithelial stroma tissue resembles endometrial glands and stroma.
The recently established international consensus statement on the current management of endometriosis[1] with the engagement of 56 representatives of 34 national and international medical and nonmedical organizations and persons led to the assumption of endometriosis being a chronic disease with multifaceted appearances and treatment options. Dr. Falconer said that endometriosis appears to be a risk factor for preterm birth, irrespective of ART. The findings of the study indicate that women with endometriosis may be considered a high risk group and need special care during pregnancy.
Endometriosis is a chronic inflammatory disease, affecting up to 15% of all women of reproductive age, in which the endometrial cells that line the uterus are deposited in other areas. Such displacement of endometrial cells can lead to anatomical distortion and also the release of anti-inflammatory cytokines, signaling molecules used in communication between cells. Known symptoms of endometriosis include severe pelvic pain, heavy menstrual periods, and nausea.
The paper only intends to describe possible complications in patients with endometriosis concerning their obstetrical outcome. It is a good description of these possible complications and of course, cannot be generalized to be a problem for all patients with endometriosis. Of course, every patient does require an individual treatment according to her fertility status, the extend of pain and her age.
Methods
In the following we focus on current treatment possibilities, pain, fertility and the obstetrical outcome in endometriosis patients.
The largest study to date of endometriosis in pregnant women has found that the condition is a major risk factor for premature birth[2]. This study was presented at the 25th Annual Conference of the European Society of Human Reproduction and Embryology (ESHRE) in 2009 by Henrik Falconer of the Department of Woman and Child Health, Karolinska Institute, Stockholm, Sweden. His team found that women with endometriosis had a higher risk of pregnancy complications and premature deliveries and were more likely to deliver by Caesarean section.
The researchers investigated the association between adverse pregnancy outcome, assisted reproduction technology (ART), and a previous diagnosis of endometriosis in 1,442,675 single births to Swedish women. They were 13,090 single ton births among 8922 women diagnosed with endometriosis. Compared with women without endometriosis, they had a 33% greater risk of preterm birth.
Results
Women with endometriosis were also more likely to have difficulty in conceiving and the use of ART was more prevalent, which in itself may be considered a risk factor for adverse pregnancy outcome, although we strongly disagree with this concept. Once conception takes place the embryo has to prove itself and fight for survival. That certainly promotes a healthy embryo but, of course, we agree that it is tiring to start the fight for life against possible cytokines or antibodies at that early stage.
Among women with endometriosis, 11.9% conceived after ART compared with the 1.4% of women without endometriosis who used the technique. This means that patients with endometriosis have a better chance of becoming pregnant with ART than without it.
The risk of preterm birth associated with endometriosis among women with ART was 1.24 and among women without ART 1.37.
One explanation for the interaction of endometriosis with preterm birth has been given by the group of Ivo Brosens with the enigmatic uterine junctional zone[3].
In addition to an increased risk of preterm birth, the researchers also found other differences in the pregnancies of women with endometriosis. Dr. Falconer reported that nearly twice as many women in this group were delivered by Cesarean section. The study group observed that among these women the risk of induced preterm birth was higher than for spontaneous preterm birth. They believe that women with endometriosis are more frequently scheduled for preterm Cesarean section, possibly due to placental complications.
Women with endometriosis were also more likely to suffer from pre-eclampsia, a condition that develops in the second or third trimester of pregnancy and involves the development of high blood pressure and the presence of protein in the urine. However, this is strongly contradicted by others[4]. Antepartal bleeding was also found to be more common among women with endometriosis. As endometriosis is so strongly associated with infertility, we know that women suffering from endometriosis are of higher maternal age and have fewer children. Even after adjusting for maternal age and other confounding factors, the strong association between endometriosis and risky pregnancies still remains.
Given that endometriosis is relatively common in women of childbearing age, we advise pregnant patients with a history of previous endometriosis to observe extra care, to enable them to have a normal pregnancy and give birth to a healthy baby.
Concerning pain in pregnancy in patients with endometriosis, there are several reports on intensified pain in pregnancy, although others report that pain totally disappears during pregnancy and breast feeding. Pregnancy appears to be a cure for these patients. However, it is a misconception to believe that pregnancy cures endometriosis. The symptoms usually recur after each pregnancy[5].
Discussion
Concerning the question of the obstetrical outcome in endometriosis patients let us pose two critical questions:
1. Endometriosis is known to interfere with conception and implantation. Is there any effect on the obstetrical outcome?
2. Do women with endometriosis need special care during pregnancy to avoid premature deliveries?
The effect on the obstetrical outcome seems to be premature delivery. The question whether endometriosis triggers recurrent spontaneous abortions was investigated following the observation that "Natural Killer (NK) cell activity" is low in endometriosis patients and high in unexplained recurrent abortions. There is good evidence that endometriosis is associated with an opposite regulation of NK cell behavior[6]. From 1991 to 1995 at least nine independent groups reported a functional defect of peripheral NK cells in patients with endometriosis. However, Somigliana et al. in 1999 concluded that the relationship between NK cell activity, endometriosis, and infertility seems to be "more puzzling" than considered so far[6]. These fine implied mechanisms may still reveal interesting biological and clinical possibilities for treatment.
Several case reports deal with obstetrical emergencies arising during delivery through endometriosis. Let us discuss a few of them:
1) A 22-year-old woman with unoperated deep endometriosis of the uterosacral ligament suddenly experienced severe abdominal pain, hematuria, and intrauterine death at 31 gestational weeks. Surgical intervention revealed an active hemorrhage from the right uterine artery and urine leakage from interruption of the right ureter in the area of a laparoscopic documented, but not treated, endometriotic nodul[7].
2) An emergency exploratory laparotomy was performed on a patient 3 days postpartum. This patient had a history of previous laparoscopic treatment for deep infiltrating endometriosis before her pregnancy. Active bleeding was found at the right uterine vein, near the site of previous surgery for deep infiltrating endometriosis[8].
3) A 30-year-old woman, at 24 weeks of gestation, was admitted with acute intra abdominal bleeding. Endometriosis lesions infiltrating the lateral wall of the uterus, the right ovarian fossa, and the right cardinal ligament were found[9].
4) A case of spontaneous postpartum hemorrhage due to massive preperitoneal implants suggestive of decidualized endometriosis was reported and verified[10,11].
Conclusion
As endometriosis remains an enigmatic disease, there is a growing realization that the origin of major obstetrical complications and problems during pregnancy may lie in very early pregnancy events. Recent studies have focused on the implantation window, particularly in endometriosis patients. The implantation window may not only be responsible for delayed implantation but also for defective deep placentation leading to preterm labor, fetal growth restriction, and pre-eclampsia.
It is a myth that pregnancy can heal endometriosis as severe pain attacks due to endometriosis can also occur during pregnancy. A relation between endometriosis and abortions remains questionable.
Obstetrical emergencies based on endometriosis, such as bleeding endometriotic lesions, uterine arteries, or veins; interruption of ureter, and postpartum haemorrhage due to decidualized endometriosis, have occurred and have to be considered.
References
- 1. Johnson, N.P., Hummelshoj, L. Consensus on current management of endometriosis. (2013) Hum Reprod 28(6): 1552- 1568.
- 2. Stephansson, O., Kieler, H., Granath, F., et al. Endometriosis, assisted reproduction technology, and risk of adverse pregnancy outcome. (2009) Hum Reprod 24(9): 2341- 2347.
- 3. Brosens, I., Derwig, I., Brosens. J., et al. The enigmatic uterine junctional zone: the missing link between reproductive disorders and major obstetrical disorders? (2010) Hum Reprod 25(3): 569- 574.
- 4. Hadfield, R.M., Lain, S.J., Raynes-Greenow, C.H., et al. Is there an association between endometriosis and the risk of pre-eclampsia? A population based study. (2009) Hum Reprod 24(9): 2348- 2352.
- 5. Wood, R., Guidone, H., Hummelshoj, L. Myths and misconceptions in endometriosis.
- 6. Somigliana, E., Vigano, P., Vignali, M. Endometriosis and unexplained recurrent spontaneous abortion: pathological states resulting from aberrant modulation of natural killer cell function? (1999) Hum Reprod Update 5(1): 40- 51.
- 7. Chiodo, I., Somigliana, E., Dousset, B., et al. Urohemoperitoneum during pregnancy with consequent fetal death in a patient with deep endometriosis. (2008) J Minim Invasive Gynecol 15(2): 202- 204.
- 8. Wada, S., Yoshiyuki, F., Fujino, T., et al. Uterine vein rupture at delivery as a delayed consequence of laparoscopic surgery for endometriosis: a case report. (2009) J Minim Invasive Gynecol 16(4): 510- 512.
- 9. Falcao, J.J., WE, S.J. Endometriosis in obstetric emergency. (2011) Free Communications and Posters, 11th World Congress of Endometriosis. Montpellier, France 1- 108.
- 10. Mabrouk, M., et al. Spontaneous postpartum hemoperitoneum in primipara with decidualized pelvic endometriosis. (2011) Free Communication and Posters, 11th World Congress on Endometriosis. Montpellier, France. 1- 112.
- 11. Marcellin, L., Santulli, P., Gogusev, J., et al. Endometriosis also affects the decidua in contact with the fetal membranes during pregnancy. (2015) Hum Reprod 30(2): 392- 405.












