Continuous Erector Spinae Plane (ESP) Analgesia In Different Open Abdominal Surgical Procedures: A Case Series
Zubair Tariq1, Niraj, G2*
Affiliation
1Speciality Doctor in Anaesthesia, University Hospitals of Leicester NHS Trust, Leicester General Hospital, Gwendolen Road, Leicester, UK
2Consultant in Anaesthesia & Pain Medicine, Clinical Research Unit of Pain Medicine, University Hospitals of Leicester NHS Trust, Leicester General Hospital, Gwendolen Road, Leicester, UK
Corresponding Author
Dr. G Niraj, Consultant in Anaesthesia & Pain Medicine, Clinical Research Unit in Pain Medicine, University Hospitals of Leicester NHS Trust, Leicester General Hospital, Gwendolen Road, Leicester LE5 4PW, Fax: 0116258 4661; E-mail: niraj.g@nihr.ac.uk
Citation
Niraj, G., et al. Continuous Erector Spinae Plane (ESP) Analgesia In Different Open Abdominal Surgical Procedures: A Case Series. (2018) J Anesth Surg 5(1): 57- 60.
Copy rights
© 2018 Niraj, G. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Continuous erector spinae plane analgesia; Open abdominal surgery; Somatic analgesia
Abstract
There has been a significant shift away from epidural analgesia following open abdominal surgery within an enhanced recovery programme. Various alternative techniques have been reported but suffer from limitations. Continuous erector spinae plane block have been described inlower abdominal surgery. Adult patients undergoingopen upper abdominal surgery, where thoracic epidural analgesia was refused or contraindicated, were offered continuous erector spinae analgesia. Surgical procedures included radical nephrectomy via a roof top incision, open nephrectomy via flank incision, liver resection, radical cystectomy and emergency laparotomy. Although erector spinae analgesia provides some visceral analgesia, it may be premature to rule that erector spinae analgesia can provide effective visceral analgesia and thereby avoid opioid supplementation following major open abdominal surgery. Continuous erector spinae plane analgesia may have the potential to be the analgesic technique of choice for providing somatic analgesia following any surgery on the abdomen.
Introduction
Optimal dynamic analgesia is recognised as the key to enhanced recovery following open abdominal surgery[1]. In the last decade, there has been a significant shift away from thoracic epidural analgesia (TEA) that has been long considered as the gold standard[2,3]. Various techniques have tried to replicate the analgesic efficacy of TEA. They include transversus abdominis plane analgesia (TAP), rectus sheath analgesia (RS), wound infusion analgesia (WI) and transmuscular quadratus lumborum (TQL) analgesia[3-8]. However each of these techniques hasspecific limitations that prevent them from being the analgesic technique of choice for all open abdominal surgeries.
Chin et al first described erector spinae plane (ESP) block for providing analgesia following ventral hernia repair[9]. Restrepo-Garces et al have described continuous ESP analgesia following lower abdominal surgery[10]. The authors present a report on continuous erector spinae plane analgesia for providing peri-operative pain relief following different major open abdominal surgeries where epidural analgesia was either refused or contraindicated.
Materials and Methods
Adult patients scheduled for major openabdominal surgery under one of the authors (NG) in whom thoracic epidural analgesia was contraindicated or refused were offered continuous erector spinae analgesia. Detailed explanation about the novel technique was provided to the patient and written consent obtained.
Open surgical procedures included radical nephrectomy with inferior vena cava exploration, liver resection, open nephrectomy utilising a flank incision, radical cystectomy with ileal conduit formation and emergency laparotomy. Patients undergoing a flank incision received continuous ESP analgesia through a single catheter.
Dermatomal testing was performed with ethyl chloride when the patient was in the post anaesthesia care unit.
Technique
The ESP catheters were inserted with the patient awake. The patient was positioned sitting and the skin of the upper back was prepared with 2% chlorhexidine solution. Counting down from the spine of seventh cervical vertebrae, the spine of the seventh thoracic vertebrae (T7) was identified. This corresponded to the tip of the scapular spine. A high frequency (5 - 10 MHz) ultrasound probe (S-NerveTM; SonoSite Inc., Bothell, WA, USA) was placed across the T7 spine and the probe was moved laterally to identify the T7 transverse process. Thereafter, the probe was moved to a vertical alignment and the erector spinae muscle was visualised lying underneath the trapezius muscle. A 16-G, 8-cm Tuohy needle (Portex; Smiths Medical International Ltd, Kent, UK) was then introduced medially in the plane of the ultrasound beam and directed towards the transverse process. Once the needle was underneath the anterior facial of the erector spinae muscle, 10 ml of saline 0.9% was injected. The injectate was observed spreading underneath the ES muscle lifting the muscle of the transverse process. A catheter (Portex; Smiths Medical International Ltd) was inserted into the newly formed space underneath the ES muscle and secured. The procedure was repeated on the contralateral side. Levo-bupivacaine (20 ml of 0.375%) solution was injected into each catheter over five minutes prior to induction of general anaesthesia. The catheters were secured in front of the upper chest (Figure 1).
Figure 1: The two erector spinae catheters connected to a Y connector in a patient following an extensive laparotomy with the incision extending from T6-L1 dermatome.
General anaesthesia was induced following insertion of the ESP catheters. Intraoperative analgesia included intravenous morphine (0.1 - 0.15 mg/kg body weight). The ESP catheters were topped up with 15 ml of 0.25% levo-bupivacaine at the end of the surgery. Post-operative analgesia included an infusion of 0.25% bupivacaine (10 ml/h) into the ESP catheters through a Y connector, regular acetaminophen 1g every 6 h and patient controlled analgesia with morphine (PA with morphine). Patients also received a bolus of 10 ml of 0.25% bupivacaine into each ESP catheter 12 h for 72 hours.
Outcomes recorded included age, gender, American Society of Anesthesiologists (ASA), body mass index, pain scores on coughing at 12, 24, 36 and 48 hours, 48 h morphine consumption, type of surgical incision and any complication with the technique.
Results
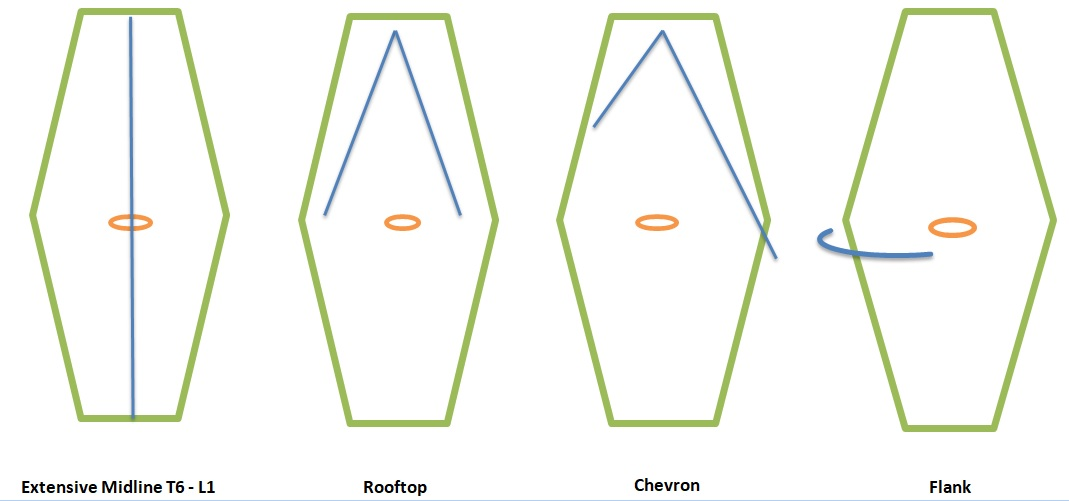
Over a six-month period, nine adult patients in whom thoracic epidural analgesia was contraindicated or refused received continuous ESP analgesia. Surgical procedures included radical nephrectomy (Figure 2), open nephrectomy, radical cystectomy, liver resection, and emergency laparotomy. Surgical incisions included extensive midline incision (thoracic dermatome T6 – lumbar dermatome L1), chevron incision, flank incision, lower midline incision (T10-L1) and rooftop incision (Figure 3).
Figure 2: Erector spinae plane catheters in a patient following radical nephrectomy and inferior vena cava exploration utilising a roof top incision.
Figure 3: The various types of surgical incisions for open abdominal surgery covered by erector spinae analgesia in this series.
The patient demographics, American Society of Anesthesiologists ASA scores, pain scores and 48 h morphine consumption are shown in Table 1. Dermatomal testing revealed loss of cold sensation from Thoracic dermatome T6 to Lumbar L1 dermatome in the anterolateral abdominal wall in all patients.
All patients had successful placement of ESP catheters. There were no complications with the technique.
Table 1: Demographic details, opioid consumption over 48 hours (mg), type of surgery and incision and pain score on coughing following surgery.
| S No | Age (y), Gender | ASA | Surgery | Incision | 48 h morphine (mg) | NRS score on coughing @ 12, 24, 36 and 48 h |
|---|---|---|---|---|---|---|
| 1 | 74, M | 3 | Radical Nephrectomy | Rooftop | 54 | 4, 3, 3, 2 / 10 |
| 2 | 66, M | 3 | Emg Laparotomy | Midline (T6-L1) | 36 | 3, 3, 2, 1 / 10 |
| 3 | 36, F | 2 | Liver Resection | Chevron | 24 | 3, 2, 1, 1 /10 |
| 4 | 72, M | 3 | Open Nephrectomy | Flank | 12 | 2, 2, 1, 1 / 10 |
| 5 | 57, F | 3 | Open Nephrectomy | Flank | 47 | 3, 2, 2, 2 / 10 |
| 6 | 79, M | 3 | Radical Cystectomy | Midline (T10-L1) | 14 | 5, 3, 3, 2 / 10 |
| 7 | 59, F | 2 | Radical Cystectomy | Midline (T10-L1) | 34 | 4, 3, 2, 2 / 10 |
| 8 | 64, M | 3 | Radical Cystectomy | Midline (T10-L1) | 50 | 4, 4, 3, 2 / 10 |
| 9 | 78, F | 3 | Emg Laparotomy | Midline (T8-L1) | 30 | 3, 2, 2, 1 / 10 |
ASA American Society of Anaesthesiologists, T Thoracic, L Lumber, NRS Numerical Rating Scale, Emg Emergency
Discussion
The authors present the first report on continuous ESP analgesia following different major open upper and lower abdominal surgical procedures. Pain following abdominal surgery has two components: somatic pain and visceral pain. Somatic pain arising from the anterior abdominal wall constitutes 70 - 75% of the pain and usually lasts for 72 hours following open surgery. Visceral pain is intense but short-lived and lasts for 24 - 36 hours. Opioids are poorly effective against somatic pain but remain the mainstay in the treatment of visceral pain. Although thoracic epidural infusion provides optimal analgesia, attenuates stress response from surgery and improves gastrointestinal motility, there are other effects that hinder enhanced recovery. These include difficulty in ambulation, intensive nursing care, analgesic failure (25 - 30%), hypotension, excessive intravenous fluid administration and the potential risks with a neuraxial technique[11]. The role of TEA within an enhanced recovery programme has been questioned 3, 11. The result is an initiative to find alternative techniques to provide analgesia after major abdominal surgery. Transversus abdomen is plane analgesia was the first abdominal wall technique touted as an alternative to TEA[4]. There are two types of TAP analgesia: Subcostal TAP analgesia for upper abdominal surgery and Posterior TAP analgesia for lower abdominal surgery[4,12,13]. Although TAP analgesia is effective in providing adequate somatic cover, it has a dermatomal limitation at T10 level[4,12-14]. Surgical incisions that cross T10 dermatome are not reliably covered by TAP analgesia[4,12]. Rectus sheath analgesia, first described over 100 years ago, has regained popularity[5]. However, RS analgesia is effective only for midline incisions. Transmuscular quadratus lumborum analgesia is a novel technique where the catheters are inserted between the quadratus lumborum and psoas major muscles with the patient in a lateral position[6]. Although initial reports confirm a paravertebral site of action, the authors experience in a limited cohort suggests possible sparing of the upper thoracic dermatomes 7.Wound infusion analgesia lacks a pre-emptive effect and is dependent on surgical expertise.
Chin et al first described ESP analgesia for abdominal surgery[15]. The site of action is reported to be the paravertebral space. We have observed intraoperative hypotension suggesting sympathetic blockade. Potential benefits of continuous ESP analgesia include pre-emptive benefit, catheters placed away from the surgical site, and analgesic efficacy in any type of surgical incision on the anterior abdominal wall.
The lower 6 intercostal nerves innervate anterior abdominal wall. The ESP plane is a high volume space with a vertical orientation. We have observed that the patients require extra bolus of local anaesthetic agents in the first 48 hours after surgery.
Visceral pain following surgery on the viscera can be intense especially in the first 24 - 36 hours. Chin et al have reported that ESP block could provide visceral analgesia in patients undergoing ventral hernia repair[15]. Ventral hernia repair involves somatic structures (anterior abdominal wall) producing intense somatic pain and minimal visceral pain. Since then reports in laparoscopic abdominal surgery have also reported on effective visceral analgesia following single shot erector spinae analgesia[16]. It may be premature to conclude that single shot ESP block can produce significant visceral analgesia. Our experience with continuous erector spinae analgesia reveals that this technique does provide some visceral analgesia and has a definite opioid sparing effect. However, continuous ESP analgesia does not provide effective visceral analgesia whereby one can completely avoid opioid analgesia during the first 48 hours following major open abdominal surgery. Our findings are supported by Restrepo-Garces and Chin et al.[10]. They reported on continuous erector spinae plane analgesia in one patient undergoing open lower abdominal surgery. The patient required supplemental analgesia with patient controlled analgesia with morphine. Despite receiving two supplemental analgesic agents with known opioid sparing effect, pregabalin and intravenous metamizole, the 48-hour opioid consumption in their patient was 18 mg[17,18]. Thus, patients require supplemental visceral analgesia with opioids in patients receiving continuous ESP analgesia.
Continuous ESP analgesia does provide effective somatic analgesia as well as some visceral analgesia thereby producing a major reduction in postoperative opioid consumption. However, the unique nature of continuous ESP analgesia is that it could be used to provide effective somatic analgesia following any type of abdominal surgery. This series highlights the unique aspect of continuous ESP analgesia that has not been reported before.
The authors accept the significant limitation of their small series of patients and the observational interpretation. The data has enabled us to design a pilot study on continuous ESP analgesia. We recommend randomised clinical trials to confirm our early findings.
Acknowledgement: The authors would like to sincerely thank Consultants in General Surgery at Leicester General Hospital for their whole hearted support.
Financial Disclosure: None
Conflict of Interest: None declared
Author’s contribution: ZT: Data Collection, Report writing, NG: Design, ESP catheter insertion, Report writing
References
- 1. Scott, M.J., Baldini, G., Fearon, K.C., et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. (2015) Acta Anaesthesiol Scand 59(10): 1212-1231.
- 2. Kehlet, H., Joshi, G.P. Systematic reviews and meta-analyses of randomized controlled trials on perioperative outcomes: an urgent need for critical reappraisal. (2015) Anesth Analg 121(4): 1104-1107.
- 3. Rawal, N. Epidural technique for postoperative pain: gold standard no more? (2012) Reg Anesth Pain Med 37(3): 310-317.
- 4. Niraj, G., Kelkar, A., Jeyapalan, I., et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. (2011) Anaesthesia 66(6): 465-471.
- 5. Wilkinson, K.M., Krige, A., Brearley, S.G., et al. Thoracic Epidural analgesia versus Rectus Sheath Catheters for open midline incisions in major abdominal surgery within an enhanced recovery programme (TERSC): study protocol for a randomised controlled trial. (2014) Trials 15(1): 400.
- 6. Borglum, J., Moriggi, B., Jensen, K., et al. Ultrasound guided transmuscular quadratus lumborum blockade. (2013) Br J Anaesth 111(22):
- 7. Warusawitharana, C., Basar, H.M.S., Jackson, L.B., et al. Ultrasound guided continuous transmuscular quadratus lumborum analgesia for open renal surgery: a case series. (2017) J Clin Anesth 42: 100-101.
- 8. Liu, S.S., Richman, J.M., Thirlby, R.C., et al. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. (2006) J Am Coll Surg 203(6): 914-932.
- 9. Forero, M., Adhikary, S.D., Lopez, H., et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. (2016) Reg Anesth Pain Med 41(5): 621-627.
- 10. Restrepo-Garces, C.E., Chin, K.J., Suarez, P., et al. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery: a case report. (2017) A A Case Rep 9(11): 319-321.
- 11. Hughes, M.J., Ventham, N.T., McNally, S., et al. Analgesia after Open Abdominal Surgery in the Setting of Enhanced Recovery Surgery. A Systematic Review and Meta-analysis. (2014) JAMA Surg 149(12): 1224-1230.
- 12. Niraj, G., Kelkar, A., Hart, E., et al. Comparison of analgesic efficacy of four-quadrant transversus abdominis plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: an open-label, randomised, non-inferiority trial. (2014) Anaesthesia 69(4): 348-355.
- 13. Hebbard, P. Subcostal transversus abdominis plane block under ultrasound guidance. (2008) Anesth Analg 106(2): 674-675.
- , , ., Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. (2008) Clin Anat 21(4): 325-333.
- 15. Chin, K.J., Malhas, L., Perlas, A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. (2017) Reg Anesth Pain Med 42(3): 372-376.
- 16. Tulgar, S., Selvi, O., Kapakli, M.S. Erector spinae plane block for different laparoscopic abdominal surgeries. (2018) Case Reports Anaesthesiol 39(4): 72-81.
- 17. Pesonen, A., Suojaranta-Yilnen, R., Hammaren, E., et al. Pregabalin has an opioid-sparing effect in elderly patients after cardiac surgery: a randomized placebo-controlled trial. (2011) Br J Anaesth 106(6): 873-881.
- 18. Tempel, G., von, Hundelshausen, B., Reeker, W. The opiate-sparing effect of dipyrone in postoperative pain therapy with morphine using a patient-controlled analgesic system. (1996) Intensive Care Med 22(10): 1043-1047.