Determinants of Male Uptake of Antenatal Care (ANC) services in Mutare City, 2015
Auxilia Chideme Munodawafa
Affiliation
- 1Africa University, Mutare, Zimbabwe
- 2Mutare Provincial Hospital Zimbabwe
Corresponding Author
Auxilia Chideme-Munodawafa, PhD. MSN. ANP. RN, Africa University, Mutare, Zimbabwe; E-mail: amunodawafa1@gmail.com
Citation
Chideme, A.M., et al. Determinants of Male Uptake of Antenatal Care (ANC) services in Mutare City, 2015 (2017) J Gynecol Neonatal Biol 3(2): 49- 62.
Copy rights
© 2017 Chideme, A.M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Male participation; Antenatal care; Mutare city
Abstract
Method: An unmatched 1:3 case-control study was conducted in Mutare Urban from May to July 2015 to establish the determinants of male uptake of antenatal care services. Data was collected on socio-demographic characteristics, health services factors and the knowledge, attitudes and perceptions of males about ANC services in Mutare city using an interviewer administered questionnaire and records review on 56 cases and 135 controls. Univariate, bivariate and multivariate data analysis was done to determine the significant that affect male involvement in ANC.
Introduction: Antenatal Care (ANC) is the care that a woman receives during pregnancy and helps ensure healthy outcomes for the woman and the new-borns. The tendency to associate family planning, pregnancy, child birth and child health as “women business”, has often led to the exclusion of men from services where they could also learn more about reproductive, maternal and child health. Male participation in the antenatal care of their spouses has been shown to increase the uptake of interventions prescribed during antenatal visits. This study seeks to establish the factors associated with male uptake of ANC services in Mutare City.
Results: The study enrolled 56 cases and 135 controls. The level of male participation in ANC services in Mutare city is low (16.7%). The perception that health-workers were overworked [AOR = 2.78, 95% C.I = (1.17, 6.62)] was associated with high male participation. Having attended ANC before [AOR= 0.20, 95% C.I = (0.09; 0.48)] and earning an income averaging between US $100 - $300 [AOR = 0.20, 95%C.I = (0.08, 0.48)] were independently associated with low male uptake of ANC services in Mutare.
Conclusion: The low participation of males in ANC services in Mutare was attributed to socio-economic factors. Different strategies such as extending clinic hours to 6 pm and extending invitations to the men are therefore called upon to make ANC more accommodative and attractive to men.
Introduction
Antenatal Care (ANC) is the care that a woman receives during pregnancy and helps ensure healthy outcomes for the woman and the new-borns[1]. Antenatal care is a key entry point for a woman to receive a broad range of preventive health services. These include the prevention, detection and treatment of diseases that adversely affect pregnant women such as malaria, tuberculosis and sexually transmitted infections (STIs) /HIV/ AIDS (so as to prevent mother to child transmission) and tetanus toxoid immunisation and other underlying medical conditions for example gestational diabetes, anaemia, pregnancy-induced hypertension and chronic kidney disease. It also provides an opportune time for counselling on the benefits of child spacing (family planning issues) (ZDHS, 2010-11). Importantly, it is a crucial link in the household-to-hospital care continuum since it is an intervention that can be provided both at the household and peripheral facility level and further assures the link to higher levels when need be.
According to the World Health Organisation (WHO, 2015), every day, approximately 800 women die from preventable causes related to pregnancy and childbirth. In 2013, 289 000 women died during and following pregnancy and child birth. Sadly, 99% of these deaths occur in developing countries. Maternal mortality remains high in rural areas and among poor communities. Young adolescents have not been spared as they face higher risk of complications and death due to pregnancy than older women. Women in developing countries have on average many more pregnancies than women in developed countries, and their lifetime risk of death due to pregnancy is higher. A woman’s lifetime risk of maternal death – the probability that a 15 year old woman will eventually die from a maternal cause – is 1 in 3700 in developed countries, versus 1 in 160 in developing countries. Between 1990 and 2013, the global maternal mortality ratio (the number of maternal deaths per 100 000 live births) declined by only 2.6% per year. This is way below the 5.5% that is required for the attainment of the Millennium Development Goal 5. More effort and focused strategies have to be identified such as male involvement in maternal health and wider reproductive health programming[2].
In many settings worldwide, ANC services seek to address the health needs of women by engaging and educating pregnant women in appropriate care seeking and care giving practices for themselves and their babies. This focus on women and a tendency to associate family planning, pregnancy, child birth and child health as “women business”, has often led to the exclusion of men from services where they could also learn more about reproductive, maternal and child health. Their exclusion has a bearing on the ANC services access as in many settings, men tend to be the decision makers in the families and often have a final say with regards to issues pertaining to family planning, allocation and use of family resources, and determining women’s access to critical health services including decisions that can result in a woman being successfully referred to a higher level when required[3]. This was reported also by Brunson, 2010[4], in a study that despite the fact men may not be knowledgeable about birth, in emergencies men still control the situation through their decision making so to prevent or reduce maternal and perinatal morbidity and mortality, they have to be involved during antenatal and postnatal care.
The involvement of men in ensuring and enhancing maternal health is actually a new idea, first hatched at a conference in Cairo in 1994, but not much has been done in practical terms in the developing world. The International Conference on Population and Development (ICPD) held in Cairo in 1994 where representatives from more than 180 countries formally acknowledged the value of men to women’s reproductive health[5] and also at the 4th World Conference on Women in Beijing drew attention to women’s health and the need to have men more involved in the promotion of sexual and reproductive health[6]. At both conferences, men’s shared responsibility and active partnership in sexual and reproductive health and promotion of gender equality was accentuated. It has been observed that the poor attitude of men towards women’s health especially in Africa had been greatly attributed to the practice of male dominance, often called “patriarchy”. Patriarchy is described as a family structure or society where the man is, as of right, the head of the family and regarded by the women as the lord and master whose decision (about any and all issues, including those of maternal health) is final[7].
Zimbabwe has a similar patriarchal system as men are the main decision makers and thus expected to provide emotional, social and financial support to their women. Therefore male participation is a crucial component in the optimisation of Maternal and Child Health services as including men in antenatal PMTCT services with HIV testing may improve infant health outcomes[8]. Mutare district is one of the 7 districts in manic land province. Mutare urban has a population of 187 621 with a sex ratio of 89.5 (Males/100 Females) (Census report, 2012). Mutare district has Government, Council and private institutions offering ANC activities. Council has 6 health facilities that offer ANC services in the city. Mutare provincial hospital is the referral centre where all complicated cases are referred to for management by specialist Obstetrician and Gynaecologists.
ANC in Zimbabwe
Zimbabwe adopted the WHO guidelines for ANC which recommend that a pregnant woman with no complications should have at least four ANC visits. These are between 12 - 16 weeks, at 28, 32 and at 36 weeks gestation. Baseline investigations like a full blood count (FBC), blood sugar level, urea and electrolytes, Rapid Plasmin Reagent (RPR), urinalysis, blood pressure measurement and an ultra-sound scan for foetal viability and well-being are done at the first booking. The woman then receives immunisations against tetanus (Tetanus Toxoid) and haematinics to protect her from the dangers of anaemia. She also gets IPT (Intermittent Presumptive Treatment) to protect her from malaria.
Problem Statement
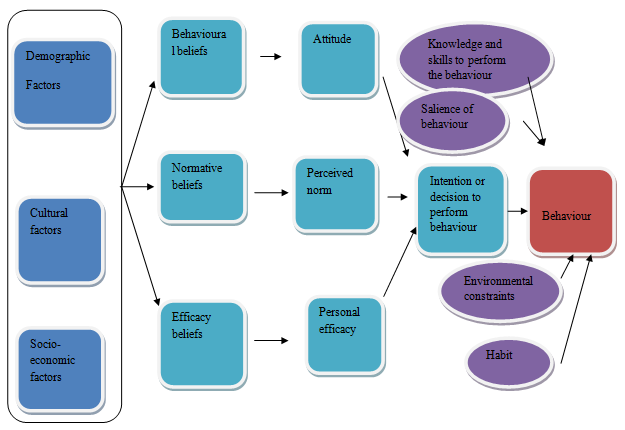
Male participation in the antenatal care of their spouses has been shown to increase the uptake of interventions prescribed during antenatal visits[9]. A review of records at Sakubva maternity clinic and Mutare provincial hospital showed that only 3.1% and 2.1% attended ANC as couples and were tested for HIV respectively. Despite couples being seen first (preferential care), male involvement remains low and this is a cause for concern. Male involvement in ANC activities may result in adherence to interventions prescribed during ANC and improvement of the outcomes of pregnancies thereby reduce maternal and prenatal morbidity and mortality. Findings from the following studies highlighted the impact of involving male participation on pregnancy outcome; Fathers’ engagement in pregnancy and childbirth: evidence from a national survey[10-11], Impact of husbands’ participation in antenatal health education services on maternal health knowledge, (2009) (Figure 1).
Figure 1: Adapted from: Health Behaviour and Health Education. Theory, Research and Practice, Fourth Edition (Karen Glanz, Barbara K. Rimer and K. Viswanath) 2005.
The above model was adopted to guide in the conduct of the study as the different factors were analysed as the independent variables
Justification
ANC provides a window of opportunity for problems associated with pregnancy to be detected thus allowing remedial action to be taken to save the lives of these mothers. The full benefits of ANC are accrued when couples attend ANC together[5]. Therefore a deeper understanding of the factors associated with low men in our setting will lead to the adoption of recommendations that will increase their involvement. Partner involvement has been shown to be complex and at times difficult to achieve in other settings due to cultural diversity[12]. This study will help identify these cultural barriers to male involvement in ANC activities in Mutare City Health Department. This study seeks to establish the factors associated with male uptake of ANC services in Mutare urban district and once these are known, to inform policy at district, provincial and national level.
Broad Objective
To determine the factors affecting male uptake of ANC services in Mutare City, 2015.
Specific Objectives
• To identify the socio-demographic factors associated with male participation in ANC activities in Mutare City, 2015.
• To determine the health services factors associated with male participation in ANC activities in Mutare City, 2015.
• To assess the knowledge, attitudes and perceptions affecting male involvement in ANC activities in Mutare City, 2015.
• To make appropriate recommendations to increase male involvement in ANC activities.
Methodology
Study Design
An unmatched 1:3 case-control study was carried out to determine the barriers to male participation in ANC activities.
Study Setting
The study was carried out in Mutare Urban District in Manic land province, Zimbabwe, from May to July 2015. Participants were enrolled into the study from the council clinics namely City, Chikanga, Hobhouse, Dangamvura, and Sakubva clinics.
Study population
The study population comprised of spouses of pregnant women attending ANC in Mutare city. A case was a spouse who accompanied his wife to and attends ANC and a control was a spouse who did not attend ANC activities with wife.
Sample size
The sample size was calculated using Epi Info version 7. Assuming a 54.7% exposure in controls, 87.1% exposure in cases, 95% confidence level, 80% power and an OR = 5.6 from a study done in Mwanza district, Malawi, where male partner involvement was found to be statistically significantly associated with condom use [AOR = 5.6, 95%CI = (2.3 – 13.5), p < 0.001)] (Kalembo, Zgambo, Mulaga, Yukai, & Ahmed, 2013), a minimum sample size of 99 participants(25 cases and 74 controls) was required (Fleiss wc 25:74). The sample size was doubled to power up the study (50 cases and 150 controls)
Sampling Methods
Selection of Mutare City Clinics
The city has a total of five clinics and participants were randomly selected to take part in the study from these clinics.
Selection of cases
All spouses that came and attended ANC with their wives were conveniently selected into the study. A total of 56 cases and 135 controls were identified and enrolled into the study.
Selection of controls
A sampling frame of pregnant women who attended ANC at these clinics without their spouses was compiled. A total of 347 women were identified and a sampling interval of 2 (347/150) was used. A die was used to select the first control. Thereafter every second control was selected until there were 150 controls. The identified controls were then followed up using their addresses or after phoning them. If a control refused to participate, the next on the line list was considered and then the interval applied.
Inclusion and exclusion criteria
Couples who were residents of Mutare City in 2015 were included and non–residents were excluded.
Pre-testing of the instrument
Pre-testing of the study instrument was done in city clinics which were not part of the study. This was done to observe the reactions of participants to the research questions and thus access the validity, reliability and acceptability of the questions. Also their willingness to answer the questions was assessed and all the questions were found to be acceptable to the participants. The time needed to administer the questionnaire was assessed.
Data Collection
An interviewer administered questionnaire was used to collect data on socio-demographic characteristics, health services factors and the knowledge, attitudes and perceptions of males about ANC services in Mutare city. All controls were traced to their homes and workplaces after contacting them using the telephone and interviewed. The majority 188(98.4%) opted to be interviewed in English and the remaining 3(1.6%) opted for Shona.
Data Analysis
Data was analyzed using Epi-info version 7 (CDC Atlanta, Georgia, USA). Univariate analysis was done on all variables and measures of central tendency were used to summarize them. Bivariate analysis was carried out and measure of association and their 95% CI and p-values were calculated. Stratified analysis using demographic variables was done to check for confounding and effect modification. The Chi-square for differing Odds Ratios by stratum was used to test if they were statistically different. All the variables whose p-value was less than 0.25 on bivariate analysis were included in a multivariate logistic regression analysis in order to determine their independent effects. Adjusted ORs and their respective 95% C.Is were obtained. The level of significance was set at p < 0.05. Logistic regression analysis was done to control for confounding and independent factors were determined. Qualitative data was sorted thematically and analyzed manually.
Ethical considerations
Permission to carry out the study was sought and granted by the Faculty of Health Sciences, Africa University, and the Provincial Medical Director Manic land Province and the Director of Health Services Mutare City. The protocol and consent forms were approved on the 23rd of April 2015 by the Africa University Research Ethics Committee (AUREC) (AUREC No AUREC 290/15).
Written informed consent was sought and granted from all the study participants before they are interviewed. Respect of their choice on whether to participate or not was maintained. Confidentiality was assured and maintained by holding interviews in secluded rooms at clinics or in their homes/workplaces and the data collected carried unique participant identification numbers and was stored in locked cabinets with limited access to the investigator to ensure its safety. The electronic data was kept in a password protected computer
All the participants that agreed to participate could read and write either English or the local language, Shona. Hence the data collection instruments were also translated into “Shona”, the local language by the linguistic department (See appendix in tables) . Also Zimbabwe as a country has 92% literacy level (United Nations Development Programme Statistical Digest, 2016) so most people are literate.
Results
Response Rate
The recruitment was below 100% as some study participants could not be located or they had moved outside the city during the data collection period. Further searches could not be done as time and resources were a limiting factor. Thus a response rate of 95.5% was achieved for this study (Table 1).
Table 1: Comparison of Sample Size at Design stage and Achievement on Recruitment.
| Sample size | Cases | Controls | Total |
|---|---|---|---|
| Calculated during design | 50 | 150 | 200 |
| Achieved (recruited) | 56 | 135 | 191 |
| % recruited (of initially calculated) | 112% | 90% | 95.5% |
Descriptive Epidemiology
A total of 56 spouses that attended ANC and 135 spouses that did not attend ANC with their wives were enrolled into the study. The median age for spouses that attended ANC was 32.5 years (Q1 = 27, Q3 = 35) and for the spouses that did not attend ANC, it was 31 years (Q1 = 25, Q3 = 35). The majority of spouses that attended and those that did not attend, 36(64.29%) and 80(59.26%) respectively, were over the age of 30 years. More than 60% of the wives of cases were aged more than 25 years and slightly more than half (53%) of the wives of controls were aged more than 25 years. Almost all of the spouses that attended ANC 55(98.21%) and those that did not attend 127(94.08%) were married, either legally or customarily. More than 75% of the spouses that attended ANC clinic and those that did not attend had attained secondary or tertiary level of education. Close to 86% of the spouses that attended ANC and 92% of the controls were employed (informally or formally) with 50% of the spouses that did not attend ANC with their wives earning between 100 - 300 US dollars (Table 2). Thirty eight of the cases and seventy-nine of the controls resided in the suburbs of Chikanga/ Hobhouse and Dangamvura. (Table 3). Men that attended ANC with their wives, 47(84%) and those that did not attend ANC, 112(84%), reported that the pregnancies were planned and there was no statistical difference between the two groups (p = 0.86). Nearly all the cases except 2 and 128(95%), were very happy about the pregnancies.
Table 2: Socio-Demographic characteristics of cases and controls of spouses of women who attended ANC in Mutare City, Zimbabwe 2015.
| Variable | Category | Cases N = 56 N (%) | Controls N = 135 N (%) |
|---|---|---|---|
| Age of Spouse | < 30 years | 20(35.71) | 55(40.74) |
| >30 years | 36(64.29) | 80(59.26) | |
| Median | 32.5 (Q1 = 27; Q3 = 35) | 31 (Q1 = 25; Q3 = 35) | |
| Age of wife | < 25 years | 21(37.50) | 63(46.67) |
| >25 years | 35(62.50) | 72(53.33) | |
| Median | 28 (Q1 = 20; Q3 = 31) | 26 (Q1 = 22; Q3 = 31) | |
| Education | Primary | 1(1.79) | 5(3.70) |
| Secondary | 39(69.64) | 93(68.89) | |
| Tertiary | 16(28.57) | 37(27.41) | |
| Marital status | Legally married | 9(16.07) | 39(28.89) |
| Customarily | 46(82.14) | 88(65.19) | |
| Co-Habiting | 1(1.79) | 6(4.44) | |
| Not living together | 0(0.00) | 2(1.48) | |
| Type of marriage | Monogamous | 55(98.21) | 127(94.07) |
| Polygamous | 1(1.79) | 8(5.93) | |
| Employment | Not employed | 7(12.50) | 11(8.15) |
| Informal | 23(41.07) | 52(38.52) | |
| Formal | 26(46.43) | 72(53.33) | |
| Religion | Catholic | 9(16.07) | 13(9.63) |
| Anglican | 0(0.00) | 10(7.41) | |
| Apostolic | 18(32.73) | 23(17.04) | |
| Pentecostal | 13(23.21) | 39(28.89) | |
| Methodist | 10(17.86) | 39(28.89) | |
| Traditional | 4(7.14) | 11(8.15) | |
| Average Monthly income | < 100 | 14(25.00) | 17(12.59) |
| 100-300 | 14(25.00) | 68(50.37) | |
| > 300 | 28(50.00) | 50(37.04) |
Table 3: Distribution of cases and controls by residence of spouses of women who attended ANC in Mutare City, Zimbabwe 2015.
| Variable (Place of residence) | Cases N (%) | Controls N (%) |
|---|---|---|
| City | 6(10.71) | 17(12.59) |
| Chikanga/Hobhouse | 18(32.14) | 31(22.96) |
| Dangamvura | 20(35.71) | 48(35.56) |
| Sakubva | 12(21.43) | 34(25.19) |
Bivariate Analysis, Individual factors
Couples who stayed together [OR = 10, 95% C.I = (1.34, 77.28) p = 0.005] had a 10 times increased odds of attending ANC compared to those not staying together and more so if they were customarily married [OR = 2.46, 95%C.I = (1.14,5.31), p = 0.03], the husbands had 2.46 times increased odds of attending ANC compared to those who were not. Spouses from the Apostolic faith sector [OR = 2.31, 95%CI = (1.12, 4.73)] were 2.31 times more likely to attend ANC with their wives compared to those of other religious sectors. Spouses who earned between US $100 - $300 dollars every month [OR = 0.31, 95%CI = (0.35, 0.62), p < 0.001] had 69% reduced odds of accompanying their wives to the ANC clinic compared to. These three findings were statistically significant (Table 4).
Table 4: Individual factors affecting male participation in ANC in Mutare City, Zimbabwe, 2015.
| Variable | Case | Control | OR 95%CI | p-value |
|---|---|---|---|---|
| AGE of spouses | ||||
| < 30 years | 20(35.71) | 55(40.74) | 0.8(0.42 - 1.54) | 0.63 |
| >30years | 36(64.29) | 80(59.26) | ||
| AGE of wives | ||||
| < 25 years | 21(37.50) | 63(46.67) | 0.69(0.36 - 1.30) | 0.32 |
| > 25 years | 35(62.50) | 72(53.33) | ||
| Education | ||||
| Primary/Secondary | 40(71.43) | 98(72.59) | 0.94(0.47 - 1.89) | 0.99 |
| Tertiary | 16(28.57) | 37(27.41) | ||
| Marital status | ||||
| Legally | 9(16.07) | 39(28.89) | 0.47(0.21 - 1.05) | 0.09 |
| married(Cha5:11) | 47(83.93) | 96(71.11) | ||
| Customarily married | 46(82.14) | 88(65.19) | 2.46(1.14 - 5.31) | 0.03 |
| 10(17.86) | 47(34.81) | |||
| Stay together | ||||
| Yes | 55(98.21) | 114(84.44) | 10(1.34 - 77.28) | 0.005(*F) |
| No | 1(1.79) | 21(15.56) | ||
| Employment | ||||
| Not employed | 7(12.50) | 11(8.15) | 0.51(0.59 - 4.39) | 0.51 |
| Employed | 49(87.50) | 124(91.85) | ||
| Average monthly income US 100-300 | ||||
| Yes | 14(25.00) | 70(51.85) | 0.31(0.15 - 0.62) | 0.00 |
| No | 42(75.00) | 65(48.15) | ||
| Religion | ||||
| Apostolic | 18(32.14) | 23(17.04) | 2.31(1.12 - 4.73) | 0.03 |
| Non-Apostolic | 38(67.86) | 112(82.96) | ||
| Do you consume alcohol | ||||
| Yes | 18(32.14) | 42(31.11) | 1.05(0.54 - 2.05) | 0.97 |
| No | 38(67.86) | 93(68.89) | ||
| Do you know your HIV status | ||||
| Yes | 43(76.79) | 95(70.37) | 1.39(0.682 - 2.87) | 0.47 |
| No | 13(23.21) | 40(26.63) | ||
| HIV Status | ||||
| Positive | 4(9.52) | 15(17.05) | 0.51(0.16 - 1.65) | 0.38 |
| Negative | 38(90.48) | 73(82.95) | ||
| Does wife know his status | ||||
| Yes | 42(75.00) | 95(70.37) | 1.26(0.62 - 2.57) | 0.64 |
| No | 14(25.00) | 40(29.63) | ||
| Was pregnancy planned | ||||
| Yes | 47(83.93) | 112(83.58) | 1.03(0.44 - 2.79) | 0.86 |
| No | 9(16.07) | 22(16.42) | ||
| Are you happy about pregnancy | ||||
| Yes | 54(96.43) | 128(94.81) | 1.48(0.30 - 7.34) | 0.92 |
| No | 2(3.57) | 7(5.19) | ||
| Type of marriage | ||||
| Monogamous | 55(98.21) | 127(94.07) | 3.36(0.42 - 28.37) | 0.39 |
| Polygamous | 1(1.79) | 7(5.19) | ||
*Fisher’s exact test
Health Services factors
The majority of spouses that attended ANC 50 (89.29%) and spouses that did not attend ANC with their wives 94 (69.63%) felt the attitude of health workers at the clinics was good [OR = 3.63, 95%CI = (1.44, 9, 15), p = 0.01]. They also felt that health workers were understaffed and hence overworked [OR = 3.76, 95%C = (1.88-7.54), p ≤ 0.001]. The majority of spouses that attended ANC 54 (96.43%) and those that did not attend ANC 109 (80.74%), felt that if invitations in the form of cards or a telephone call were extended to them, they would attend ANC services with their wives [OR = 6.44, 95% CI = (1.47, 28.14), p = 0.01]. These findings were statistically significant. The majority felt there was privacy at the clinics and the waiting times did not affect their attendance at ANC clinics though these findings were not statistically significant (Table 5).
Table 5: Health Services factors affecting male participation in ANC in Mutare City, Zimbabwe, 2015.
| Variable | Case | Control | OR 95%CI | p-value |
|---|---|---|---|---|
| Perception of H/worker attitude | ||||
| Good | 50(89.29) | 94(69.63) | 3.63(1.44-9.15) | 0.01 |
| Don’t know | 6(10.71) | 41(30.37) | ||
| Health workers overworked | ||||
| Yes | 42(75.00) | 59(44.36) | 3.76(1.88-7.54) | < 0.001 |
| No | 14(25.00) | 74(55.64) | ||
| Is there privacy at clinics | ||||
| Yes | 42(75.00) | 92(68.15) | 1.40(0.69-2.84) | 0.44< |
| No | 14(25.00) | 43(31.85) | ||
| Do waiting times at the clinic result in you not attending | ||||
| Yes | 22(39.29) | 52(38.52) | 1.03(0.55-1.96) | 0.95 |
| No | 34(60.71) | 83(61.48) | ||
| Attend ANC if invited | ||||
| Yes | 54(96.43) | 109(80.74) | 6.44(1.47-28.14) | 0.01 |
| No | 2(3.57) | 26(19.26) | ||
Knowledge, Attitudes and Perceptions
Spouses that had attended ANC before were 55% less likely to attend ANC with their wives again [OR = 0.450; 95% CI = (0.24, 0.87) p]. Also the majority of the spouses that attended ANC 53(94.6%) and spouses that did not attend ANC 103(76.3%) felt it was necessary for men to attend ANC with their wives and those spouses that accompanied their wives were 5.49 times more likely to attend ANC sessions so as to learn about the health of pregnant women during the health education sessions. (Table 6)
Table 6: Knowledge, Attitudes and Perceptions of spouses of women who attended ANC in Mutare City, 2015.
| Variable | Case | Control | OR 95%CI | p-value |
|---|---|---|---|---|
| Have you attended ANC before | ||||
| Yes | 18(32.14) | 69(51.11) | 0.45(0.24-0.87) | 0.03 |
| No | 38(67.86) | 66(48.89) | ||
| Know any pregnancy related complications | ||||
| Yes | 45(80.36) | 111(82.22) | 0.88(0.40-1.96) | 0.92 |
| No | 11(19.64) | 24(17.78) | ||
| Are pregnant women given medicines | ||||
| Yes | 35(62.50) | 97(71.85) | 0.65(0.34-1.26) | 0.27 |
| Don’t know | 21(37.50) | 38(28.15) | ||
| Is it necessary for men to attend ANC | ||||
| Yes | 53(94.64) | 103(76.30) | 5.49(1.61-18.76) | < 0.001 |
| No | 3(5.36) | 32(23.70) | ||
| Are you comfortable attending ANC | ||||
| Yes | 52(92.86) | 112(82.96) | 2.67(0.88-8.11) | 0.12 |
| No | 4(7.14) | 23(17.04) | ||
| Have you read/heard any programmes on ANC | ||||
| Yes | 45(80.36) | 90(66.67) | 2.05(0.97-4.33) | 0.09 |
| No | 11(19.64) | 45(33.33) | ||
Stratified Analysis
This was done to control for confounders and assess for effect modification (Table 7). The Crude OR for the spouses of women who attended ANC and were of the Apostolic sect was 2.37 with 95% CI = (1.15, 4.87). The relationship between attending ANC by spouses with their wives and religion is modified by income earned by these spouses. The Crude OR, 2.37 lies between the two stratum specific ORs of 1.83 and 4.02. The Chisquare for differing Odds Ratios by stratum indicates that the odds ratios differ significantly by stratum (Chi-square statistic c = 4.56, p-value = 0.03).
Table 7: Relationship between Religions of spouses of women who attended ANC in Mutare City, 2015, stratified by income earned.
| Variable | Category | Attended ANC | Stratum specific | OR 95%C.I. | p-value | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Stratum 1: > US100 | ||||||
| Apostolic | Yes | 6 | 11 | 4.02 | 1.17 - 13.89 | 0.02 |
| No | 8 | 59 | ||||
| Stratum 2: < US100 | ||||||
| Apostolic | Yes | 12 | 12 | 1.83 | 0.73 - 4.58 | 0.20 |
| No | 29 | 53 | ||||
Multiple Logistic Regressions
Multiple logistic regressions were done to control for confounding and effect modification. All the factors whose p-value were less than 0.25 on bivariate analysis were included and a step-wise approach was applied (Table 8). The perception that health-workers were overworked [AOR = 2.78; 95%C I = (1.17, 6.62), p = 0.02] was independently associated with male attendance of ANC services. Having attended ANC before [AOR = 0.20; 95%CI = (0.09, 0.48, p < 0.001) and earning income averaging between US$100-$300 dollars [AOR = 0.20; 95%CI = (0.08 - 0.48), p < 0.001) were independently associated with reduced male uptake of ANC services in Mutare. Being customarily married [AOR = 2.09, 95%CI = (0.83, 5.22) p = 0.12], having invitations extended to men [AOR = 1.90, 95% CI = (0.22, 16.32), p = 0.56], whether it was necessary for men to attend ANC with their wives [AOR = 2.72, 95%CI = (0.27, 28.0), p = 0.4], whether men were comfortable attending ANC with their wives [AOR = 0.23; 95% CI = (0.03-2.09), p = 0.19], having read or heard any male involvement information through the media [AOR =2.35, 95% CI = (0.80, 6.94), p = 0.12] and if the couple stayed together [AOR = 5.95, 95% C I = (0.65, 54.72), p = 0.12] were attenuated and did not retain significant associations with male involvement after multiple logistic regression.
Table 8: Independent Factors Associated with Male uptake of ANC services in Mutare City, 2015.
| Variable | Crude OR (95% C.I.) | Adjusted OR (95% C.I.) | p-value |
|---|---|---|---|
| Health-worker overworked | 3.63(1.44-9.15) | 2.78(1.17-6.62) | 0.02 |
| Having attended ANC before | 0.45(0.24-0.87) | 0.20(0.09-0.48) | 0.00 |
| Income between US 100-300 dollars | 0.31(0.15-0.62) | 0.20(0.08-0.48) | 0.00 |
| Customarily married | 2.46(0.83-5.22) | 2.09(0.83-5.22) | 0.12 |
| Invitation to attend ANC | 2.46(1.14-5.31) | 1.90(0.22-16.32) | 0.56 |
| Is it necessary for men to attend ANC | 5.49(1.61-18.76) | 2.72(0.27-28.0) | 0.40 |
| Are you comfortable attending ANC | 2.67(0.88-8.11) | 0.23(0.03-2.09) | 0.19 |
| Have you read/heard any male attendance information through media | 2.05(0.97-4.33) | 2.35(0.80-6.94) | 0.12 |
| Do you stay together as a couple | 10(1.34-77.28) | 5.95(0.65-54.72) | 0.12 |
Discussion
In Mutare City, over the study period, only 1in 6 (16.7%) male partners attended ANC with their wives. This level of involvement is low and is reported in other studies from West Africa and Asia. For example, one study done in the Atelewo community in Osogbo, Osun State, Nigeria, only 24% of the men attended ANC with their wives[13]. In Cameroon it was observed that male participation did not exceed 18%[14]. In Mekelle, Northern Ethiopia it was reported that male participation was also low at 20%[15]. In our study, we identified a number of factors that were associated with male participation in ANC services in Mutare city. These included socio-economic, health service delivery and cultural factors. In our study, the age of the pregnant woman was not associated with male partner involvement. This was also reported in a study done in Ethiopia by Abubay, Abebe and Fentahun, 2014[16], who found that age of the wife was not statistically associated with male participation in ANC services even though it was reported to have an association in a study done in the DRCby Ditekemena et al, 2011, who found that older age was associated with male involvement. In Sweden, where Ekeus and Christensson, 2003[17], supported this finding and reported that fathers of babies born to older primiparous women (> 25 years) were more likely to participate in ANC activities that fathers of younger primiparous mothers (< 25 years).
The majority of couples (> 95%) in our study were in a monogamous relationship and this was not associated with male participation (OR 3.36, C.I. 0.42 - 28.37, p = 0.39) as was found in the DRC or in Cameroon where men in polygamous relation ships showed higher involvement[14]. Also in Nairobi, Kenya, Farquhar et al, 2004, reported that being married (p < 0.001), in a polygamous marriage (p = 0.013) and living together (p < 0.001) were associated with male participation in ANC/VCT activities. In our study, for couples that were customarily married, the men were 2.46 times more likely to participate in ANC activities on bivariate analysis (OR,2.46, 95% C.I. 0.83 - 5.22). This could be attributed to the continued family support and stability that is associated with traditional marriages, though this was not statistically significant on logistic regression (AOR 2.09, 95% C.I. 0.83 - 5.22 p = 0.12). This is in line with the findings of Katz et al, 2009[18], in Nairobi, Kenya, who found that being in a monogamous marriage and living together was associated with male attendance at the ANC clinic (AOR 4.34, 95% C.I. 1.05 to 18.0).
Byamugisha et al (2010)[12], reported that men in Uganda who had completed 8 or more years of education were two times more likely to be involved in ANC activities compared with those with less than 8 years of education (OR = 1.9; 95% CI: 1.1 - 3.3; p ≤ 0.05). This was not the case in our study in Mutare city where the level of education of spouses did not influence male participation (OR = 0.94; 95% CI 0.47 - 1.89; p > 0.05). This could be because the majority (> 70%) of spouses (both men who attended ANC and those that did not attended) had attained secondary education (high literacy rate). Our finding is in line with that found by Tweheyo, Konde-Lule, Tumwesigye, and Sekandi, 2010[19], in Northern Uganda who found that the male partner’s level of education was not associated with male participation in ANC activities. Our findings also concur with those of Ampt et al, 2015[20] who reported that in Myanmar, the level education of the spouses that attended ANC sessions was not associated with levels of involvement in ANC activities on multivariate analysis. It was interesting to note that in other settings, researchers had found that no education or having attained primary education was associated with high male involvement, Bhatta, 2013[10], in Nepal and Awungafac et al, 2015[21], in Cameroon.
Previous studies done in Kenya[22], Cameroon[14] and Tanzania[23], have found financial constraints as a barrier to attending ANC services. This was also confirmed in our study where husbands who earned less than US300 dollars were 80% less likely to attend ANC clinics with their wives (AOR = 0.20; 95% CI;0.08 - 0.48; p < 0.05). This could be due to the fact that the husbands were informally employed and spent most of their time at their workplaces. Most were drivers, carpenters, vendors or other skilled workers running their own workplaces such that they lacked time to participate in ANC activities especially during the day. Possibly men could be encouraged to attend by opening clinics on weekends when some men are not in paid work, however, since many of the men that did not attend ANC were informally employed, this may hinder attendance. This is similar to findings of Byamugisha et al, 2010[12], where being informally employed and earning less meant these men would spare less time to attend ANC with their wives. Given the prevailing situation in Zimbabwe where many men will find themselves in the informal sector urgent strategies have to be put in place if the level of male involvement is to improve.
It is conventional in many African countries that men do not go together with their wives to the ANC clinics. Studies done by Benkele (2007)[24], Mullick, Kunene and Wanjiru (2005)[25], Mbizvo and Basset (1996)[26] and Falnes et al, (2011) [27] showed that culturally men do not accompany their wives to ANC consultations as they deemed these activities as women’s business. In our study it was interesting to find that men of the Apostolic sect were four times more likely to attend ANC with their wives especially those that were earning more than US 100 dollars (OR = 4.02; 95% CI; 1.17 - 13.87; p < 0.05). This could indicate a change in behaviour in this group warranting further research. Also after multivariate analysis, we found in our study that men that did not attend ANC with their wives were 77% less likely to feel comfortable accompanying their wives to the ANC clinics (AOR 0.23 95% C.I.0.03 - 2.09, p = 0.19). In our study, men considered accompanying their wives to the ANC clinics as important (AOR 2.72, 95% C.I. 0.27 - 28.0, p = 0.40) but they were no doing it. This was in line with what was also reported by Nkuoh, Meyer, Tih, and Nkfusai, (2010)[14], in Cameroon who also found men acknowledging the importance of accompanying their wives to ANC clinics but not actually doing it.
Studies done in Uganda[12] and Kenya (Reynolds and Kimani, 2006), observed that health workers in ANC clinics were perceived by men not to be client friendly, in our study men perceived them to be good and helpful (OR = 3.63; 95% CI;1.44 - 9.15; p < 0.05). This was because when they attended ANC with their wives, they were attended to first and were also given one to one service. As a result there was no delay at the clinic. This is also reported by Kululanga, Sundby, Malata and Chirwa, 2011[28], in Malawi where the fast and first strategy was used when couples come together for ANC, they were attended to first. Health workers were critical of this strategy as it was not sustainable in the long run. It only worked as long as few men attended ANC but when the numbers increased, it would not be applicable. They also felt strongly that health workers were overworked (AOR = 2.78; 95% CI; 1.17 - 6.62; p < 0.05). This they thought could explain why in some instances health-workers are perceived to be rude, harsh and at times lack of respect for patients. The male peer initiative is also used in Malawi such that those men who would have attended ANC with their wives are encouraged to inform their peers about their experiences. Influential men in these societies can act as role models and made to impart the benefits of male participation.
In our study waiting times at the clinic was not an issue with regards to male participation (OR 1.03, 95% C.I. 0.55 - 1.96, p = 0.95) as was found in the DRC[29], Nigeria[30] and Uganda[31]. This could have been due to the fact that for 71(37.17%) of the men recruited into the study, this was the first pregnancy their wife was carrying and so had no experience of the on-goings at the ANC clinics. In Malawi incentives were offered to reduce the waiting time by using the fast and first strategy. Health care workers also criticised this strategy as it pronounced the traditional gender role that men are the breadwinners so they need not wait for long at the clinics. This again is not sustainable in the future if men start attending ANC with their wives but until then, it indeed however motivated male involvement in antenatal care.
In Uganda, it was suggested that one of the ways to increase male participation was to invite the men through their wife’s cards[12]. This is supported by researchers in South Africa[32], who also found that the men who had received written invitations were 1.36 times more likely to attend ANC clinics with their wives than those who had received verbal invitations [relative risk (RR) 1.36, 95% confidence interval (CI) 1.12 – 1.64, P = 0.002]. In our study, we found that spouses were two times more likely to attend ANC activities if invited, though not statistically significant on logistic regression (AOR = 1.90; 95% CI, 0.22; 16.32; p > 0.05), it could be clinically significant and a strategy that can be used to increase male participation. This is further supported by systematic review done by Morfaw, F., et al., 2013[33] that showed that inviting men to the health institution for voluntary testing and counselling was a key health system facilitator.
Interestingly[34] in a randomised facility-based intervention trial, found that the percentage of trial participants who attended the antenatal clinic with their spouses increased to 16.2% (86/530) and 14.2% (75/530) in the intervention and non-intervention groups, respectively (OR = 1.2; 95% CI: 0.8, 1.6). The intervention was an invitation letter and the control group received an information letter, a leaflet, concerning antenatal care. This showed that even receiving information could change one’s perception and behaviour. This is supported by findings of Singh, D., 2014[35], that it may just be an issue of providing more information to men so that they understand the proven benefits of attending antenatal care and supporting their wives.
Several studies mention men being concerned about HIV-associated stigma as why they end up not going to ANC clinics. Sprague, Chersich and Black[36] in South Africa; Reece, Hollub, Nangami[22] and Lane in Western Kenya and Ndiaye et al (2009)[37] in West Africa found that men were afraid of HIV disclosure at health facilities. This could be the reason why in our study men who had attended ANC clinics before were less likely to participate in these activities (AOR = 0.20; 95%C.I; 0.09; 0.48; p < 0.05). Despite not being statistically significant, men who were HIV positive were 49% less likely to attend ANC services with their wives (OR 0.51, 95%C.I. 0.16 - 1.65, p = 0.38). In our setting, all pregnant mothers are required to have an HIV test and to protect them from being infected during pregnancy, it is thus imperative to also test their spouses since some couples can be discordant. We found that men who participated in ANC activities were 1.39 times more likely to know their HIV status than those that did not participate (OR = 1.39; 95%C.I. 0.68- 2.87, p = 0.47) and in most instances they would be indeed negative. Seventy-three (82.95%) of the men that did not accompany their wives to the ANC clinic claimed to be HIV negative and their status was not verified to ascertain the true status. This calls for the strengthening of strategies to upscale couple counselling and testing so that definitive sero-status of couples is known so as to reduce the possibility of HIV transmission.
At the same time health workers have to be mindful of the dangers of couple counselling and testing. In Zambia, Musheke[38] concluded that despite the biomedical and social benefits associated with couple counselling and testing, it had to be non-coercive as it could lead to abandonment, cessation of sexual relations between couples and intimate partner violence. According to the Zimbabwe Demographic and Health Survey (2010 - 11), in urban settings, 5.9% of HIV positive men were married to an HIV negative woman, 3.9% of HIV positive women was married to HIV negative men and 12.8%, both were HIV positive. This reinforces the need to test couples but because men know that they will be tested, this could be a hindrance and hence less likely to attend ANC sessions with their wives as some feared abandonment if they were found HIV positive and their wives negative.
Accessing male involvement information through the media has been shown to increase male participation in ANC activities. In Malawi, health workers reported that couples who used the couple initiative strategy attended all ANC visits together[28]. In our study men who attended ANC with their wives were 2.35 times more likely to have heard male involvement information through the media than those who did not (AOR = 2.35, 95%C.I. 0.80 - 6.94, p = 0.12). Though not statistically significant in logistic regression, the media could be used to enhance male involvement in ANC services. In Lilongwe Malawi, Mphonda, found that engaging peer educators using drama in ANC facilities resulted in increased male involvement in ANC activities. It was after the dramas had been done in the appropriate language, and the messages were relevant that they began to see an increase in men participation. In Uganda, similar interventions such as music, dance and drama were used to spread the information on the benefits of male involvement in ANC activities[39]. The number of male partners that attended ANC rose from 16.7% to 89.6% over a two year period. Therefore combing community and health facility interventions can result in male participation in ANC activities.
Since many of the studies that have been done to date were qualitative in nature, a cluster randomised controlled trial is under way in South Africa to try and assess the nature and impact of male involvement as it remains unclear and untested[40-45]. The ‘Protect Your Family’ trial will test the effectiveness of a behavioural intervention to significantly increase adherence to male participation, determine whether the intervention conducted both with or without the participation of male partners will have an additive or synergistic (or negative) impact on ANC services such as PMTCT. The study ends in 2018 after which the effectiveness and impact of male participation in ANC services will be assessed. It will be interesting what the results of this study will show.
Study Limitations
Access of participants through their wives could have caused selection bias as well as recall bias of participants. Time limit as well as exclusion criteria of only including urban participants was another limitation.
Conclusion
The level of male participation in ANC services in Mutare city is low. This was attributed to socio-economic factors such as earning less than US300 dollars and perceptions and attitudes after having attended ANC clinics before by spouses of pregnant women contributed to this low participation. Maternal health initiatives that solely focus their thrust on women may therefore be flawed considering the patriarchal society that we live in. Different strategies such as couple counselling, extending operating times of clinics to cater for the working men and the use of invitation cards are therefore called upon to make ANC more accommodative and attractive to men. Findings from this study were presented to both provincial and central authorities for action.
APPENDICES
Annex I: English/Shona Questionnaire
Questionnaire number …...
Socio-Demographic Characteristics
1. Case [ ] Control [ ]
2. Age (Makaberekwa rini? ) DOB_________________
3. AGE of wife (Mudzimai wenyu akaberekwa rini?) DOB____
4. Marital status (Munemuchato here?) Legally married [ ] Customarily married [ ] Just staying together (Cohabiting) [ ] Not together [ ]
5. How many wives do you have (Mune madzimai mangani?) One [ ] Two [ ] Three [ ] Four [ ] Other [ ]
6. This is you’re.......Marriage. (Muchato wechingani) First[ ] Second [ ] Third [ ] Fourth [ ] Other [ ]
7. Do you live together as a couple (Munogara pamwe nemudzimai wenyu here?) Yes [ ] No [ ]
8. Number of children the couple has (Mune vana vangani?) ___________
9. Education (Makadzidza mukagumira papi?) None [ ] Primary [ ] Secondary [ ] Tertiary [ ]
10. Place of Residence (Munogara kupi?) Sakubva [ ] Dangamvura [ ] Chikanga [ ] City [ ]
11. Employment (Munoshanda here?) Unemployed [ ] Informal employment [ ] Formal employment [ ]
12. What is your Profession? (Makadzidzira basa ripi?)__________________________________
13. Average monthly income (Munotambira marii?) 0-$100[ ] $100-$300 [ ] Above $300 [ ]
14. Religion (Munopinda svondo ipi?) Catholic [ ] Anglican [ ] Methodist [ ] Pentacostal [ ] Apostolic [ ] Atheist [ ] Traditional [ ]
Individual factors
15. Do you consume alcohol?(Munonwa doro/mhamba here?) Yes [ ] No [ ]
16. How often? (Kangani pasvondo?) Once a week [ ] Twice [ ] More than twice but not every day [ ] Every day [ ]
17. Do you know your HIV status (Makamboongororwa here nezveutachiona weHIV?) Yes [ ] No [ ]
18. If No, why have you not been tested (Kana musati, chikonzero ndechei?)____________________________
19. What is it? (Makanzi zvakamira sei?) Positive [ ] Negative [ ] Not comfortable disclosing [ ]
20. Does your wife know your status? (Mudzimai wenyu anoziva mamiriro enyu here?) Yes [ ] No [ ]
21. Was this pregnancy planned? (Pamuviri pane mudzimai wenyu pangapakatarisirwa here?) Yes [ ] No [ ]
22. Are you happy about this pregnancy? (Zvakakufadzai here pamakaziva kuti mai vabata pamuviri?) Yes [ ] No [ ]
23. If Yes/ No (Delete inapplicable), Why? (Sei makafara/ musina kufara?)_____________________________ Health service factors
24. What is your perception of health worker attitudes to patients at the clinic? (Munoona sei mabatirwo avarwere nanamukoti pakiriniki? Good [ ] Harsh [ ] Fearsome [ ] Do not know [ ]
25. Do you think the health workers are overworked? (Munofunga here kuti vanamukoti basa ravo rakawandisa?) Yes[ ] No [ ]
26. Is there privacy at the clinics? (Pakiriniki pane kuwanzika here apo varwere pavanenge vachirapwa?) Yes[ ] No [ ] Don’t know [ ]
27. Does the waiting time at clinics affect your attendance? (Munoona kumira kwenguva refu pakiriniki kuchikutadzisai kuuya here?) Yes [ ] No [ ] Don’t know [ ]
28. If invited to attend ANC with your wife, would you attend? (Mukakokwa kuti muuye nemudzimai wenyu, munouya here?) Yes [ ] No [ ]
Knowledge, Attitudes and Perceptions
29. Have you attended ANC before? (Makamboendawo kuskero namai here?) Yes [ ] No [ ]
30. What services are offered at ANC? (Chii chinoitwa kuskero?)_____________________________________
31. Do you know of any complications of pregnancy? (Pane zvinogona kukanganisika here kana mai vakazvitakura?) Yes [ ] No [ ]
32. If yes, which ones? (Zvii zvinogona kukanganisi____________________________________
33. Are pregnant women given any medicines during pregnancy? (Vanamai kana vakazvitakura, vanopihwa mishonga kana mapiritsi here?) Yes [ ] No [ ] Don’t know [ ]
34. Which ones do you know? (Munozivaipi?)__________________________________
35. Do you think it’s necessary for women to attend ANC? (Munoona zvakakosha here kuti vakadzi vaende kuskero?) Yes[ ] No [ ]
36. If yes/no, why? (Seimadaro? ____________________________________
37. Do you think it’s necessary for men to attend ANC with their wives? (Munofunga kuti zvakakosha here kuti varume vaende nemadzimai avo kuskero?) Yes [ ] No [ ] Don’t know [ ]
38. If Yes/No (Delete in applicable), why? (Sei muchidaro?)________________________________
39. Are you comfortable attending ANC with your wife? (Makasununguka here kuenda kuskero nemudzimai wenyu?) Yes [ ] No [ ]
40. If Yes/No (Delete inapplicable), Why? (Nemhaka yei?) ______________________________________
41. Have you read/ heard any programme on ANC services? (Makambonzwawo here kana kuverenga nezveskero?) Yes[ ] No [ ]
42. Which form of media did you hear about ANC services? (Makazvinzwara kana kuverenga pai? Radio [ ] TV [ ] Print media [ ] Electronic media [ ]
Thank you very much (Ndatenda)
Appendix 2 English Consent Form
ENGLISH CONSENT FORM (Adapted from the MRCZ Consent Form)
Introduction
Topic: Determinants of Male Uptake of Antenatal Care (ANC) services in Mutare City, 2015
Principal investigator: Stephen Murahwa [MBChB (UZ)]
Phone number: 0712877019/ 0773264418
Academic Supervisor: Prof. A Chideme-Munodawafa Phone No. 0772136880
Africa University Research Ethics Committee: P. O. BOX 1320 Mutare Zimbabwe, TEL (+263-20) 60075/60026/61611 E-MAIL: aurec@africau.edu
Approval Number: AUREC290/15
What you should know about this research study:
• We give you this consent so that you may read about the purpose, risks, and benefits of this research study.
• The main goal of this research is to gain knowledge that will help you understand and appreciate the importance of attending ANC with your expecting wives.
• We cannot promise that this research will benefit you directly.
• You have the right to refuse to take part, or agree to take part now and change your mind later.
• Whatever you decide, it will not affect your wife’s health care and assistance she will get at health facilities.
• Please review this consent form carefully. Ask any questions before you make a decision.
• Your participation is voluntary.
Purpose
You are being asked to participate in a study on ‘Determinants of Male Uptake of Antenatal Care (ANC) services in Mutare City, 2015’ .The purpose of the study is to determine the factors affecting male uptake of ANC services in Mutare City, 2015 You were selected as a possible participant in this study because your name corresponded to a number that was picked from the ANC attendance register at random. You are one of 220 participants to be interviewed for this study.
Procedures and Duration
If you decide to participate, you will be interviewed using an interviewer administered questionnaire. It will take about 15-20 minutes.
Risks and Discomforts
Your participation in this research will increase the time you are going to be at the health facility or at your house.
Benefits and/or Compensation
We do not promise that you will receive monetary or material benefits from this study. If you have suffered stress and discrimination and are in need of assistance, we will offer you appropriate treatment.
Confidentiality
If you indicate your willingness to participate in this study by signing this document, we will not include your name on the questionnaire. We plan to disclose any information obtained from this study to Manicaland Provincial Medical Director, the Director Health Services of Mutare City Council and the Faculty of Health Sciences, Africa University, for the purpose of evidence based planning of programs and improving service delivery to our clients. Any information obtained in connection with this study that can be identified with you will remain confidential and will be disclosed only with your permission.
Additional Costs
There will be no additional costs to you.
Voluntary Participation
Participation in this study is voluntary. If you decide not to participate in this study, your decision will not affect your wife’s future relations with any health facilities and its personnel. If you decide to participate, you are free to withdraw your consent and to discontinue participation at any time without penalty.
Offer to Answer Questions
Before you sign this form, please ask any questions on any aspect of this study that is unclear to you. You may take as much time as necessary to think over it.
Authorization
You are making a decision whether or not to participate in this study. Your signature indicates that you have read and understood the information provided above, have had all your questions answered, and have decided to participate.
------------------------------------ -----------
Name of Research Participant (please print) Date
--------------------------------------------------- -------------------
Signature of Participant or legally authorized representative Time
Appendix 3: Shona version
TSAMBA YECHITENDERANO (Adapted from the MRCZ Consent Form)
Kutanga
Tsvagurudzo yekuda kuziva ‘Maoonero nemafungiro avana baba maererano nekuenda kuskero nemadzimai avo apo vanenge vakazvatakura muguta reMutare, mugore ra 2015’.
Muongorori: Stephen Murahwa [MBChB (UZ)]
Nhamba dzenhare: 0712877019/0773264418
Murairidzi wangu: Prof. A Chideme-Munodawafa Phone No. 0772136880
Africa University Research Ethics Committee P. O. BOX 1320 Mutare Zimbabwe, TEL (+263-20) 60075/60026/61611 E-MAIL: aurec@africau.edu
Approval Number: AUREC290/15
Zvamunofanira kuziva maererano neongororo ino:
• Tirikukupai tsamba yechitenderano chino kuti mugonzwisisa zvinangwa zveongororo ino, zvakaipa uye zvakanakira ongororo ino.
• Chinangwa cheongororo ino ndechekutsvaga ruzivo maererano nemaonero kana mafungiro avana baba panyaya yekuenda kuskero nemadzimai avo apo vanenge vakazvitakura.
• Hatikuvimbisei kuti pane zvamuchawana kuburikidza nekupinda muongororo ino.
• Makasununguka kuramba kupinda muongororo ino kana kubvuma kupinda iyezvino uye makasununguka kuzoramba panguva inotevera.
• Kubvuma kana kuramba kupinda mongororo ino, hazvikanganise kubatsirwa kwemudzimai wenyu panguva inotevera.
• Nyatsoverengai nekunzwisisa gwaro rino zvakakwana. Kana paine mibvunzo, sunungukai kubvunza musati masarudza kupinda kana kusapinda muongororo ino.
• Kupinda kwenyu muongororo ino hakumanikidzwe.
Chinangwa
Muri kukumbirwa kuti mupinde mutsvagurudzo yekuda kuziva maererano nemaonero kana mafungiro avana baba panyaya yekuenda kuskero nemadzimai avo apo vanenge vakazvitakura muguta reMutare mugore ra 2015. Masarudzwa nekuda kwekuti zita renyu raenderana nenhamba yangodomwa mugwaro remadzimai akaonekwa kuskero pakirini kwete kuti pane zvamaita kanazvamunazvo. Tinotarisira kukurukura nevanhu mazana maviri ane makumi maviri (220) mutsvagiridzo ino.
Maitirwo nenguva yeongororo
Kana matenda kupinda muongororo iyi muchatarisirwa kupindura mibvunzo yamuchabvunzwa. Zvichatora nguva inosvika maminetsi gumi nemashanhu kana makumi maviri chete.
Njodzi nekushungurudzi
Kupinda kwenyu muongororo kuchawedzera nguva yamuchange muri pano pakiriniki kana pamba penyu.
Zvakanakira kuva muongororo
Hapana muripo wemari kana zvinhu zvamuchawana kuburikidza nekuva muongororo ino
Kuvimbika kweongororo
Kana mukasarudza kupinda muongororo ino kuburikidza nokuisa runyoro rwenyu, zita renyu harisi kuzoiswa pagwaro rinenge rine mhinduro dzenyu. Zvatinenge tawana mutsvagurudzo ino tinotarisira kuzivisa mukuru wezveutano weManicaland (PMD), mukuru wezveutano wekanzuru yeMutare uye nevadzidzisi vedu vepa AfricaYunivhesiti nechinangwa chekuda kuwedzera mabatsiro atingaita vana baba maererano nekukosha kuenda kwavo kuskero nemadzimai avo apo vanenge vakazvitakura. Zvichawanikwa muongoro ino zvinogona kunangana nemi zvinochengetedzwa muchiwande uye zvinogona kuzoburitswa chete kana imi muchinge mazvitendera.
Mumwe muripo
Hamuna chamunobhandara muongororo ino.
Kusununguka kupinda muongororo
Isarudzo yenyu kupinda muongororo ino. Kusarudza kusapinda muongororo ino hakukanganisi mabatirwo kana marapirwo achaitwa mudzimai wenyu pakiriniki. Mukasarudza kupinda muongororo ino parizvino, makasununguka kusarudza kubuda muongororo panguva inotevera pasina muripo.
Kupindurwa kwemibvunzo
Musati maisa runyoro rwenyu pabepa rino, makasun ungoka kubvunza mibvunzo pamunenge musina kunzwisisa. Makasununguka kutora nguva yamunoda kana muchida kumbonotanga mafunga nezvazvo.
Mvumo
Muri kuita sarudzo yekupinda kana kusapinda muongororo ino. Runyoro rwenyu runoratidza kuti maverenga uye manzwisisa umbowo hwamapihwa, majekeserwa pamaive musina kunzwisisa uye masarudza kupinda muongororo ino.
______________________________ _____________
Zita remupinduri (nyorai zvinooneka) Zuva
________________________ _________
Runyoro rwechibvumirano rwemupinduri Nguva
References
- 1. World Health Organisation (WHO)/United Nations Child’s Emergency Fund (UNICEF). Antenatal Care in Developing Countries. Promises, Achievements and Missed Opportunities- An Analysis of the trends, Levels and Differentials. (2003) WHO, Geneva.
Pubmed || Crossref || Others - 2. United Nations (2008). Committing to action: Achieving the MDGs, Background note by the Secretary-General for the High-level Event on the Millennium Development Goals, United Nations, New York, The Millennium Development Goals Report 2008, United Nations; UNFPA Webpage No Woman Should Die Giving Life: Facts and Figures
Pubmed || Crossref || Others - 3. Davies, J., Stanley, L., Wendy, H., et al. Men and Maternal and newborn health: benefits, harms and challenges and potential strategies for engaging men, Compass. (2012) Women’s Child Health Kno Hub.
Pubmed || Crossref || Others - 4. Brunson, J. Confronting maternal mortality, controlling birth in Nepal: the gendered politics of receiving biomedical care at birth. (2010) Soc Sci Med 71(10): 1719-1727.
Pubmed || Crossref || Others - 5. UNFPA: Report of the international conference on population and development. (1994) Cairo. UNFPA, New York 5–13.
Pubmed || Crossref || Others - 6. United Nations: Report of the fourth world conference on women: (1995) Beijing. United Nations, New York 4–15.
Pubmed || Crossref || Others - 7. Nwokocha, E.E. Maternal crises and the role of African men: The case of a Nigerian community. (2007) African Popul Stud 22(1).
Pubmed || Crossref || Others - 8. Aluisio, A., Richardson, B. A., Bosire, R., et al. Male Antenatal Attendance and HIV Testing Are Associated with Decreased Infant HIV Infection and Increased HIV Free Survival. (2011) J Acq Immune Def Syndro (1999) 56(1): 76–82.
Pubmed || Crossref || Others - 9. Cohen, S.I. Partnering: A new approach to sexual and reproductive health. (2000) 3: 196.
Pubmed || Crossref || Others - 10. Bhatta, D. N. Involvement of males in antenatal care, birth preparedness, exclusive breast feeding and immunizations for children in Kathmandu, Nepal. (2013) BMC Pregnancy and Childbirth 13: 14.
Pubmed || Crossref || Others - 11. Lakhey, B., Shrestha, D., Hindin, M.J., et al. Impact of husbands' participation in antenatal health education services on maternal health knowledge. (2009) JNMA J Nepal Med Assoc 48(173): 28-34.
Pubmed || Crossref || Others - 12. Byamugisha, R., Tumwine, J.K., Semiyaga, N., et al. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. (2010) Reprod Health 7: 12.
Pubmed || Crossref || Others - 13. Adenike, A.O., Oluwaseyi, O.I. Attitudes and Practices of Males towards Antenatal Care in Saki West Local Government Area of Oyo State, Nigeria. (2013) Adv Life Sci Techn 22.
Pubmed || Crossref || Others - 14. Nkuoh, G.N., Meyer, D.J., Tih, P.M., et al. Barriers to men’s participation in antenatal and prevention of mother-to-child HIV transmission care in Cameroon, Africa. (2010) J Midwifery Womens Health 55(4):363–369.
Pubmed || Crossref || Others - 15. Haile, F., Brhan, Y. Male partner involvements in PMTCT: a cross sectional study, Mekelle, Northern Ethiopia, (2014) BMC Pregnancy Childbirth 14: 65.
Pubmed || Crossref || Others - 16. Abubay, Y., Abebe, L., Fentahun, N. Male involvement in the Prevention of Mother to Child Transmission of HIV and Associated Factors among Males in Addis Ababa, Ethiopia. (2014) Ameri J Health Res 2(6): 338-343.
Pubmed || Crossref || Others - 17. Ekeus, C., Christensson, K. Reproductive history and involvement in pregnancy and childbirth of fathers of babies born to teenage mothers in Stockholm, Sweden. (2003) Midwifery 19(2): 87-95.
Pubmed || Crossref || Others - 18. Katz, D.A., Kiarie, J.N., John-Stewart, G.C., et al. Male Perspectives on Incorporating Men into Antenatal HIV Counselling and Testing. (2009). PLoS One 4(11) 7602.
Pubmed || Crossref || Others - 19. Tweheyo, R., Konde-Lule, J., Tumwesigye, N. M., et al. Male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda. (2010) BMC Pregnancy Childbirth 10: 53.
Pubmed || Crossref || Others - 20. Ampt, F., Mon, M. M., Than, K. K., et al. Correlates of male involvement in maternal and newborn health: a cross-sectional study of men in a peri-urban region of Myanmar. (2015) BMC Pregnancy Childbirth 15: 122.
Pubmed || Crossref || Others - 21. Awungafac, G., Njukeng, P. A., Ndasi, J. A., et al. Prevention of mother-to-child transmission of the Human Immunodeficiency Virus: investigating the uptake and utilization of maternal and child health services in Tiko health district, Cameroon. (2015) Pan Afr Med J 20: 20.
Pubmed || Crossref || Others - 22. Reece, M., Hollub, A., Nangami, M., et al. Assessing male spousal engagement with prevention of mother-to-child transmission (PMTCT) programs in western Kenya. (2010) AIDS Care 22(6): 743–750.
Pubmed || Crossref || Others - 23. Msuya, S.E., Mbizvo, E.M., Hussain, A., et al. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: implications for preventive programs. (2008) AIDS Care 20(6): 700–709.
Pubmed || Crossref || Others - 24. Benkele, R.G. Male involvement and participation in prevention of mother to child transmision (PMTCT) of HIV/AIDS: the case of Chipata district. (2007) Bachelors University Zambia, Department of Nursing.
Pubmed || Crossref || Others - 25. Mullick, S., Kunene, B., Wanjiru, M. Involving men in maternity care: health service delivery issues. (2005) Agenda Special Focus.
Pubmed || Crossref || Others - 26. Mbizvo, M.T., Bassett, M.T. Reproductive health and AIDS prevention in sub-Saharan Africa: the case for increased male participation. (1996) Health Policy Plan 11(1): 84–92.
Pubmed || Crossref || Others - 27. Falnes, E.F., Moland, K.M., Tylleskär, T., et al. “It is her responsibility”: partner involvement in prevention of mother to child transmission of HIV programmes, northern Tanzania. (2011) J Inter AIDS Society 14: 21.
Pubmed || Crossref || Others - 28. Kululanga, L.I., Sundby, J., Malata., A., et al. Striving to promote male involvement in maternal health care in rural and urban settings in Malawi – a qualitative study. (2011) Reprod Health 8: 36.
Pubmed || Crossref || Others - 29. Ditekemena, J., Matendo, R., Koole, O., et al. Male partner voluntary counselling and testing associated with the antenatal services in Kinshasa, Democratic Republic of Congo: a randomized controlled trial. (2011) Int J STD AIDS 22(3): 165–170.
Pubmed || Crossref || Others - 30. Adelekan, A. L., Edoni, E. R., Olaleye, O. S. Married Men Perceptions and Barriers to Participation in the Prevention of Mother-to-Child HIV Transmission Care in Osogbo, Nigeria. (2014) J Sex Transm Dis 680962.
Pubmed || Crossref || Others - 31. Larsson, E.C., Thorson, A., Nsabagasani, X., et al. Mistrust in marriage-Reasons why men do not accept couple HIV testing during antenatal care- a qualitative study in eastern Uganda. (2010) BMC Public Health 10: 769.
Pubmed || Crossref || Others - 32. Mohlala, B.K., Gregson, S., Boily, M.C. Barriers to involvement of men in ANC and VCT in Khayelitsha, South Africa (2012) AIDS Care 24(8): 972–977.
Pubmed || Crossref || Others - 33. Morfaw, F., Mbuagbaw, L., Kunda, J., et al. Male involvement in prevention programs of mother to child transmission of HIV: a systematic review to identify barriers and facilitators. (2013) Syst Rev 2: 5.
Pubmed || Crossref || Others - 34. Byamugisha, R., Åstrøm, A. N., Ndeezi, G., et al. Male partner antenatal attendance and HIV testing in eastern Uganda: a randomized facility-based intervention trial. (2011) J Int AIDS Soc 14: 43.
Pubmed || Crossref || Others - 35. Singh, D., Lample, M., Earnest, J. The involvement of men in maternal health care: cross-sectional, pilot case studies from Maligita and Kibibi, Uganda. (2014) Reprod Health 11: 68.
Pubmed || Crossref || Others - 36. Sprague, C., Chersich, M. F., Black, V. Health system weaknesses constrain access to PMTCT and maternal HIV services in South Africa: a qualitative enquiry. (2011) AIDS Res Ther 8: 10.
Pubmed || Crossref || Others - 37. Ndiaye, C., Boileau, C., Zunzunegui, M.V., et al. Gender-Related Factors Influencing HIV Serostatus Disclosure in Patients Receiving HAART in West Africa. (2008) World Health Popul 10(3): 43-54.
Pubmed || Crossref || Others - 38. Musheke, M., Bond, V., Merten, S. Couple experiences of provider-initiated couple HIV testing in an antenatal clinic in Lusaka, Zambia: lessons for policy and practice. (2013) BMC Health Serv Res 13: 97.
Pubmed || Crossref || Others - 39. Ediau, M., Wanyenze, R. K., Machingaidze, S., et al. Trends in antenatal care attendance and health facility delivery following community and health facility systems strengthening interventions in Northern Uganda. (2013) BMC Pregnancy Childbirth 13: 189.
Pubmed || Crossref || Others - 40. Farquhar, C., Kiarie, J.N., Grace, C., et al. Antenatal Couple Counselling Increases Uptake of Interventions to Prevent HIV-1 Transmission. (2004) J Acquir Immune Def Syndr 37(5): 1620-1626.
Pubmed || Crossref || Others - 41. Kalembo, F. W., Zgambo, M., Mulaga, A. N., et al. Association between Male Partner Involvement and the Uptake of Prevention of Mother-to-Child Transmission of HIV (PMTCT) Interventions in Mwanza District, Malawi: A Retrospective Cohort Study. (2013) PLoS ONE 8(6): e66517.
Pubmed || Crossref || Others - 42. Larson, A Social context of human immunodeficiency virus transmission in Africa: historical and cultural bases of east and central African sexual relations. (1989) Rev Infect Dis 11(5): 716-731.
Pubmed || Crossref || Others - 43. Choko, A.T., Chimwaza, A.F., Muula, A.S. Invitation Cards during Pregnancy Enhance Male Partner Involvement in Prevention of Mother to Child Transmission (PMTCT) of Human Immunodeficiency Virus (HIV) in Blantyre, Malawi: A Randomized Controlled Open Label Trial. (2015) PLoS One 10(3): 0119273.
Pubmed || Crossref || Others - 44. Maggie, R., Henderson, Jane. Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. (2013) 13: 70.
Pubmed || Crossref || Others - 45. Sheffield, J.S., Wendel, G.D. Jr., McIntire, D.D., et al. The effect of progesterone levels and pregnancy on HIV-1 coreceptor expression. (2009) Reprod Sci 16(1): 20-31.
Pubmed || Crossref || Others