Disulfiram Induced Psychosis
Hemendra Singh1*, Rahul Rao M2, Radhika A3, Murali Thyloth4
Affiliation
- 1Assistant Professor, Department of Psychiatry, Ramaiah Medical College, Bengaluru
- 2Junior resident, Department of Psychiatry, Ramaiah Medical College, Bengaluru
- 3Junior Resident Department of Pharmacology, Ramaiah Medical College, Bengaluru
- 4Professor Department of Psychiatry, Ramaiah Medical College, Bengaluru
Corresponding Author
Dr. Hemendra Singh, Assistant Professor, Department of Psychiatry, Ramaiah Medical College, Bengaluru, Tel: +8971220731, E-mail: hemendradoc2010@gmail.com
Citation
Singh, H., et al. Disulfiram Induced Psychosis. (2017) J Addict Depend 3(2): 1- 3.
Copy rights
© 2017 Singh, H. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Alcohol dependence syndrome; Disulfiram; Psychosis
Abstract
Background: Disulfiram was widely used as an aversive agent for treatment of alcohol dependence since its discovery. Various adverse drug reactions have been documented. Psychosis due to disulfiram is not a common side effect.
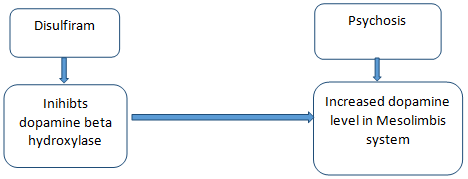
Methods & Discussion: We report two cases of disulfiram associated psychosis. We also highlight the biological mechanism of the psychosis associated with disulfiram use. The Dopamine (DA) hypothesis of schizophrenia states that an increase in DA activity in certain brain areas is associated with psychotic symptoms in schizophrenic patients. The possible explanation for the development of psychosis, might be inhibition of Dopamine-Betahydroxylase (DBH) enzyme due to metabolites of disulfiram. This enzyme catalyzes the metabolism of DA into norepinephrine. Inhibition of DBH increases dopamine level. Furthermore, alcoholics who developed psychosis due to disulfiram were found to have low levels of amine and monoamine oxidase, suggesting DBH blockage.
Conclusion: Disulfiram induced psychosis is not an uncommon side effect. Biological mechanism of Disulfiram induced psychosis, probably via its DBH inhibiting effects, which lead to an increase in DA activity. Hence, careful monitoring is required for emergent of psychotic symptoms in vulnerable patients while on disulfiram treatment.
Introduction
Disulfiram (tetraethylthiuram disulfide) is a quaternary ammonium compound, which is an aversive agent used for treating alcohol dependency[1]. In Copenhagen, researchers studying compounds to treat parasitic stomach infections take a small dose of disulfiram to check its side effects. Later they become ill after an alcoholic drink. They conclude that an interaction of disulfiram and alcohol is responsible and conduct a study to confirm their findings[2]. Early 1950’s, FDA approves disulfiram to treat alcohol dependence in the United States. The side effects associated with disulfiram are metallic taste, rashes & abdominal upset, hepatological, dermatological & psychiatric in nature. Organic causes of psychosis always need to be ruled out before arriving at diagnosis. We present two cases of disulfiram induced psychiatric disturbances that we encountered at our Hospital
Case Report
Case 1
A 50 year old married male, was brought to psychiatry department with 2 weeks history of talking to self, and suspiciousness towards the family members, as well as towards certain other people saying that they would harm him. On further clarification of history, it was found that he has been consuming alcohol for the last 35 years, with daily drinking of 90 ml to 180 ml alcohol since 20 years. His last drink was 2 months ago. He had no family and past history of psychiatric illnesses and other substance use disorders. In view of quitting the alcohol use, he was started on Tab. Disulfiram 500 mg OD. It was found that there was a temporal correlation between the initiation of disulfiram and the development of psychotic symptoms in a span of 1 week. His systemic examinations including central nervous system were normal. Relevant investigations like haemoglobin, serum vitamine B12, Thyroid function tests, serum electrolytes were done to rule out other possible causes of psychosis and to rule out delirium. All investigations were within normal limits. He was treated with Olanzapine 10 mg for 5 days, and it was stopped after a week. Further, serial Mental Status Examinations were performed it was found that his psychotic symptoms had resolved. He had no further episode of psychosis during regular follow up.
Case 2
A 32 year old male, with history of alcohol dependence since past 15 years, was brought to the psychiatry department. It was found from the family members that since last 6 to 7 weeks, he was showing suspiciousness and constantly believed that people are talking about him, and also showed hallucinatory behavior in the form of talking to self in isolation. He would say that people around him are getting to know about his thoughts with clear consciousness. His last drink of alcohol was 4 months back. Patient had several admissions for alcohol dependence in the past and had tried to abstain but was unsuccessful. Patient was started on Disulfiram 250 mg/day and escitalopram 10 mg/day 2 months prior to coming to our hospital. He had no past and family history of any other psychiatric illnesses. His systemic examinations including central nervous system were normal. Relevant investigations were done to rule out other possible causes of psychosis and were within normal range. Disulfiram was stopped and his psychotic symptoms were improved within a week period. During follow up, patient was maintaining well with escitalopram 10 mg and without any psychotic symptoms for about 6 months, and had no symptoms during the follow up period. After one year, patient started consuming alcohol and he was restarted with Tab. Disulfiram 250 mg/day, and after 2 weeks in the next follow up, he was found to have delusions of reference, persecution and anger outbursts. Tab. Disulfiram was again stopped and Tab. Amisulpride 200 mg BD was started. Patient’s psychotic symptoms improved within a week period. Patient was treated with topiramate 25 mg/day built upto 50 mg/day, for alcohol dependence.
Discussion
Disulfiram is used in alcohol addiction. When there is co-occurrence of alcohol consumption, it produces sensitivity to alcohol, leading to an unpleasant reaction, ethanol-disulfiram reaction, caused by the accumulation of acetaldehyde through the inhibition of the enzyme acetaldehyde-dehydrogenase with histamine release[3]. The most common symptoms of this harmful reaction are hypotension, tachycardia, diaphoresis, flushed face, headache, nausea, vomiting, and confusion; however, only 28% of patients experience these symptoms that are under disulfiram treatment, after having alcoholic consumption[4,5]. Disulfiram can also cause adverse symptoms, when used unique, such as drowsiness, fatigue, impotence, headaches, skin eruptions, neurological toxicity, and psychosis[5]. Disulfiram major metabolites, carbon disulfide and Diethyldithiocarbamate (DDC) are associated with side effects. Disulfiram major metabolite diethyldithiocarbamate is an inhibitor of dopamine beta hydroxylase, an enzyme involved in conversion of dopamine to norepinephirne. Thus leading to increase concentration of dopamine in the mesolimbic system & inducing psychosis as stated by the “dopamine hypothesis” described in schizophrenia[6]. Krishna et al in two studies, reported 5 cases of psychosis out of 53 and 6 cases in a total of 52 patients under disulfiram treatment[7]. Adverse reactions can last for 2 weeks after administering disulfiram, but usually they last no longer than 3 days after suspending this drug[8]. Psychosis develops in patients who are vulnerable that is, family history of psychosis[9]. In our first case psychotic symptoms emerged during a week of initiation of the disulfiram and remitted well with antipsychotic drugs within a period of one week. In our second case psychotic symptoms were lasted for more than 2 months as patient was on disulfiram for 2 months, however psychotic symptoms remitted within a week period after stopping of the disulfiram. However, re-challenge with disulfiram after 12 months period also resulted in the psychotic episode in the second case. The causality assessments of the adverse drug reactions were performed by using the WHO and Naranjo’s causality scales. As per the WHO[10] scale, the adverse drug reactions was found to be ‘certain’ in its causality. Naranjo’s causality scale[11] score for this reaction was found to be 9, which implies that the adverse drug reaction was ‘certain’ due to the drug.
The dopamine (DA) hypothesis of schizophrenia states that an increase in DA activity in certain brain areas is associated with psychotic symptoms in schizophrenic patients[12]. The possible reason for the development of psychosis in a patient on disulfiram is that, it is an inhibitor of Dopamine-Betahydroxylase (DBH), an enzyme that catalyzes the metabolism of DA to Norepinephrine (NE)[13]. Alcoholics who developed psychotic symptoms during disulfiram treatment are found to have low levels of amine and monoamine oxidase, suggesting DBH blockage[9]. Hence, blockade of norepinephrine synthesis and production may relate to psychosis and mania among patients on disulfiram therapy[14]. Genetic vulnerability such as family history of psychiatric illnesses had been debated as a predisposing factor for psychosis in the literature[15]. Supporting the genetic diasthesis as a contributing factor, patients with family history of psychosis or mania also reported with disulfiram induced psychosis[9]. Relatively more prevalence of disulfiram associated psychosis in eastern countries also suggests possible role of genetic factors[16]. Use of disulfiram during alcohol intake or higher dosages of disulfiram also might be a contributing factor for the psychosis[17]. Hence, proper evaluation is required to rule out the various contributing factors of psychosis before starting patients on disulfiram therapy.
Figure 1: Flow Chart of Possible Mechanism of Disulfiram Induced Psychosis.
Conclusion
Our observation supports the hypothesis that Disulfiram induced psychosis may have a pathophysiological substrate i.e increased dopamine level, which shows remarkable response to a typical antipsychotic agents. Hence, careful monitoring is required for emergent of psychotic symptoms in vulnerable patients while on disulfiram treatment
References
- 1. Oshea, B. “Dissulfiram revisited”. (2000) Hosp Med 61(12): 849-851.
Pubmed || Crossref || Others - 2. Hald, J., Jacobson, E., Larsen, V. “The sensitizing effect of tetraethyl thiuramdisulphide (Antabuse) to ethyl alcohol”. (1948) Acta Pharmacol 4: 285-296.
Pubmed || Crossref || Others - 3. Reisberg, B. “Catatonia associated with dissulfiram therapy”. (1978) J Ner Ment Dis 166(8): 607-609.
Pubmed || Crossref || Others - 4. Rainey, J.M.Jr. “Disulfiram toxicity and carbon disulfide poisoning”. (1977) Am J Psychiatry 134(4): 371–378.
Pubmed || Crossref || Others - 5. Choi, D.W. “Glutamate neurotoxicity and diseases of the nervous system”. (1988) Neuron 1(8): 623-634.
Pubmed || Crossref || Others - 6. Rossiter, S.K. “Psychosis with disulfiram prescribed under probation order”. (1992) BMJ 305(6856): 763.
Pubmed || Crossref || Others - 7. Sherif, P.A., Krishna, M. “Psychosis and enuresis during dissulfiram therapy”. (2006) Indian J Psychiatry 4(1): 62–63.
Pubmed || Crossref || Others - 8. Bagadia, V.N., Dhawale, K.M., Shah, L.P. et al. “Evaluation of disulfiram in the treatment of alcoholism”. (1982) Indian J Psychiatry 24(3): 242-247.
Pubmed || Crossref || Others - 9. Nasrallah, H.A. Vulnerability to disulfiram psychosis. (1979) West J Med 130(6): 575-577.
Pubmed || Crossref || Others - 10. The use of the WHO–UMC system for standardised case causality assessment.
Pubmed || Crossref || Others - 11. Naranjo, C.A., Busto, U., Sandor, P. et al. A method for estimating the probability of adverse drug reactions. (1981) Clin Pharmacol Ther 30(2): 239–245.
Pubmed || Crossref || Others - 12. Meltzer, H.Y., Stahl, S.M. The dopamine hypothesis of schizophrenia: A review. (1976) Schizophr Bull 2(1): 19-76.
Pubmed || Crossref || Others - 13. Goldstein, M., Lauber, E., Anagnoste, B., et al. Inhibition of dopamine-B-hydroxylase by disulfiram. (1964) Life Sci 3: 763-767.
Pubmed || Crossref || Others - 14. Melo, de.R.C., Lopes, R., Alves, J.C. A case of psychosis in disulfiram treatment for alcoholism. (2014) Case Rep Psychiatry 561092
Pubmed || Crossref || Others - 15. Kety., S.S., Rosenthal., D., Wender., P.H. “Mental illness in the biological and adoptive families of adopted individuals who have become schizophrenic”. (1976) Behav Genet 6(3): 219-225.
Pubmed || Crossref || Others - 16. Murthy, K.K. Psychosis during disulfiram therapy for alcoholism. (1997) J Indian Med Assoc. 95(3): 80-81.
Pubmed || Crossref || Others - 17. Brewer, C. “How effective is the standard dose of disulfiram? A review of the alcohol-disulfiram reaction in practice”. (1984) Br J Psychiatry 144(2): 200-202.
Pubmed || Crossref || Others