Dysphagia as an Interdisciplinary Problem. Difficulties in the Diagnostic Process
Corresponding Author
Barbara Maciejewska
Citation
Maciejewska, B. Dysphagia as an Interdisciplinary Problem. Difficulties in the Diagnostic Process – Case Report. (2017) J Food Nutr Sci 4(2): 93- 97.
Copy rights
Keywords
Dysphagia, Malnutrition, Artheria lusoria, Cerebral palsy, Esophageal stenosis, Vascular anomalies
Abstract
Dysphagia is a relatively common diagnostic problem. This case shows the importance of a broad multidisciplinary diagnostic attitude. Many diseases including esophageal tumors, the Parkinson’s disease, cerebral palsy, myasthenia gravis, trismus, temporomandibular joint disorders, gastrointestinal reflux can cause swallowing problems. In this paper, a case of a young 20-year-old woman with dysphagia and malnutrition due to congenital vascular pathology malnutrition is presented. The article briefly presents the differential diagnosis of dysphagia.
Introduction
Introduction
Dysphagia is a more and more common problem because of the increasing prevalence of gastro esophageal reflux disease, a growing population aged over 65 and a longer life expectancy. The problematic propulsion of food bolus from the mouth to the stomach can classify as an oropharyngeal dysphagia - observed when discoordination of the aero digestive system (including breathing, swallowing and vocalizing) is present[1]. Also as an esophageal pathology when there is no or only slower propulsion of the bolus in the esophagus[1,2]. Difficulties of swallowing could be a complication of a stroke or degenerative illnesses as well as due to aging. It is a distinct additional risk factor of death in patients with motor neuron disease[2]. Approximately 60% of young adults with cerebral palsy have difficulty with management of oral secretions, and dysphagia[3]. The main causes are listed in [Table 1]. Dysphagia may lead to dehydration, malnutrition, or aspiration pneumonia and may have negative social and psychological consequences, e.g. feeding of the patients with cerebral palsy may take 45 minutes up to 1 hours, also may result in poor energy (caloric) intake and body weight loss[3]. Both good nutrition and quality of life are very important in the process of recovery. Due to the wide range of etiological factors of dysphagia the diagnosis may needs many different clinical specialists –a neurologist, gastroenterologist, laryngologist, phoniatrician or cardiologist, dietician. In the diagnostic process it is worth remembering that the causes and associations of dysphagia with different disease states are different among different age groups. An analysis of 189 articles shows that there are different causes of dysphagia depending on the age[1]. Congenital abnormalities/pathologies, acute infection, injury and neurodevelopmental delay are the most common in infancy, childhood and adolescence. Gastroesophageal and immunologic causes are predominant in the middle-aged population. In the elderly, it is associated with neurodegenerative diseases and oncologic causes[1]. The paper presents a case of arteria lusoria with a right-sided aortic arch manifested in a 20-year-old woman with mild residual cerebral palsy complaining of marked weight loss and dysphagia. An aberrant Left Subclavia Artery (LSCA) in patients with a right-sided aortic arch occurs in about 1/1000 of the general population. However, until 2004 only 32 cases had been published of symptomatic aberrant LSCA in the adult population[4]. The diagnosis remained elusive until a CT scan of the chest was performed; angiography further delineated the pathology. The differential diagnosis was discussed.
Table 1: The main causes of dysphagia.
| Diseases | causes |
| cranial nerves | Neuropathy (facial nerve paralysis, diabetic vagal neuropathy, GuillainBarre syndrome) |
| cerebral cortex and brain stem | Cerebrovascular disease Multiple sclerosis Motor neuron disease Parkinson’s disease Alzheimer’s disease Cerebral palsy |
| neuromuscular junction | Myasthenia gravis Eaton-Lambert syndrome botulism |
| muscle | Polyomyositis, dermatomyositis, myopathy dystrophy |
| inflammations | Herpes, candida, pharyngitis, radiation therapy, tonsillitis, gastritis (GERD) |
| Structural defects | Congenital-Cleft palate, schatzki ring, vascular rings Acquired – injury, resection |
| tumors | Cancers of the tongue, lips, palatum, mouth, Nasopharyngeal cancers, brain tumors, laryngeal tumors, tumor of the esophagus, mediastinum |
The table was created based on information from references[1,2,10,13].
Case Report
D.S., a 20 year-old girl with a three-year history of progressive dysphagia and malnutrition was referred to Neurology Ward for diagnosis. Her swallowing problems had progressed to the point that she could eat only small meals, so her BMI on admission was 17,9 (49.9 kg, 1.67 cm).
Her past medical history was positive and revealed a residual cerebral palsy (left facial paralysis). The first symptoms observed by the patient’s family were body weight loss and unwillingness to eat, permanent weakness. Before hospitalization the woman was suspected of emotional problems somatization/conversion and stress reaction (pharyngeal globus) - the first symptoms appeared just before her high school finals but the pharmacology (tranquilizers) was unsuccessful and psychological tests did not confirm it.
So she was further diagnosed by an endocrinologist to exclude struma, as well as by a gastroenterologist to exclude Gastroesophageal Reflux (GERD) and achalasia. Both consultations reveled no abnormalities. On admission she still complained of difficulty in swallowing. Her main complaints were difficulty in swallowing or sometimes odynophagia, and discomfort in the form of compression in the thorax during eating, no problems with breathing. The discomfort was localized just in the upper part of the neck close to incisura jugularis sterni. Moreover, the uncomfortable feeling was present even when swallowing saliva. She also complained of restricted movement of the jaw sometimes painful, a clicking sound in her jaw from time to time.
The patient was alert, self-reliant, without any weakness of the muscles. The neurological examination revealed scoliosis, a left facial paralysis II/III according to House and Brackmann’s scale – observed since childhood, which caused discrete asymmetry of her face; reflexes were very brisk but not pathological. When taking her medical history, an abnormal resonance in her voice was found (hyperrhinolalia or open nasality). Taking into account the symptoms and signs, differential diagnosis was planned. Because of the dysphagia and nasality, tests for the myasthenia gravis were done at first. No muscle weakness or fatigue was observed. EMG was within the normal limit; moreover the antiacetylcholine receptor antibodies in the blood test were not detected.
Residual cerebral palsy was also taken under consideration, because as a newborn she experienced problem with muscle tension. But now only a discrete left site facial paralysis remains. Magnetic Resonance Imaging (MRI) did not reveal anything specific – only a few unremarkable hyperintense, rounded lesions on MRI sequences described as vascular lesions; there were no lesions in the pons. Then anorexia nervosa was suspected. It was excluded after consultation by a psychiatrist. The laryngological and phoniatric examination did not revealed any pathology: no dyspnea was observed, no choking during the water and food swallow test such as mastication, tongue movements and tongue propulsion of the bolus to the oropharynx did not interfere with swallowing. There were no remains in the oral cavity after swallowing the bolus. However, the patient felt discomfort in the neck and the upper part of the thorax. The speech with discrete nasality, rather habitual because of the anatomical structure of the palatum; other organs in the oral cavity (the tongue, alveolars, teeth) were normal. Laryngoscopy revealed the smooth vocal folds in normal colour, mobile during breathing and phonation, with proper closure to protect against aspiration; no food in the valeacule and piriformis, discrete redness of mucosa in the inter arytenoid notch as in the previous evaluation [Figure 1a].
The gastroscopy was also performed to exclude gastro esophageal reflux disease because of redness of mucosa in the vestibulum of the larynx [Figure 1b]. The results were as followed: the esophagus without pathological morphological lesions, no hypertension of the Upper Esophageal Sphincter UES, bright liquid in the stomach, with a little amount of bile, the mucosa had normal structure, inversion: fundus and UES normal, the duodenum without pathological lesions, no stricture was revealed. The evaluation of the esophagus with contrast was within the normal limit. A biopsy of the mucosa from the stomach revealed tissues of normal morphology and structure; blood test to measure antibodies to Helicobacter pylori was negative. The eagle syndrome was excluded too – an x-ray of the scull showed short processus styloiseus (2.8 mm).
Figure 1: Endoscopic views of the patient’s larynx (a - laryngoscopy) and the esophagus (b- gastroscopy).
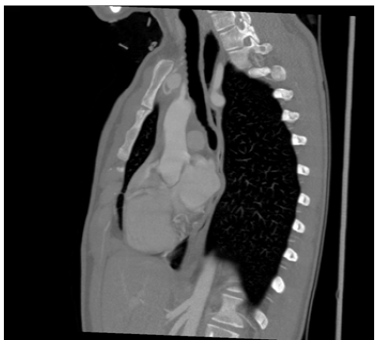
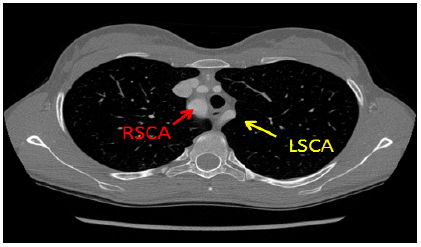
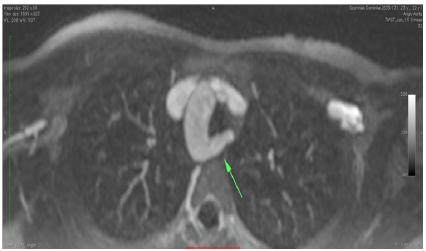
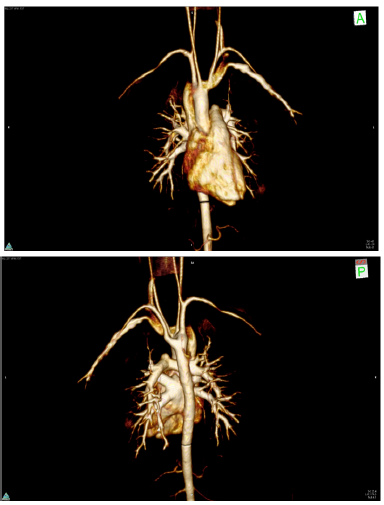
The dental evaluation showed restricted opening of the mouth and clicking sounds during chewing – symptoms of the temporomandibular disorder. The symptoms did not prevent to form bolus inside the mouth, however mouthfuls of food there smaller than normal. To sum up, the oropharyngeal phase was normal but the esophageal phase was affected. The Modified Barium Swallow (MBS) revealed effortless easy-going passage of the bolus with barium but there was a narrowing of the esophagus at the level of the aortic arch [Figure 2]. As a result, a computer tomography of the chest was performed [Figure 3]. The major finding in the patient was the right-sided aorta, with The Left Subclavian Artery (LSCA) originating as its last branch and following a retro esophageal course. Significant compression of esophagus was observed with dilatation of its lumen to 2 cm in the proximal part. Due to the persistence and worsening of the patient’s symptoms, a surgical correction was recommended. Approximately a month later, the patient was admitted to Cardio surgical Department where MRI was done with 3D reconstruction of the blood vessels [Figures 4,5]. She underwent endovascular embolization of the abnormally passed proximal part of the left arteria subclavia by Vascular Plug t.2 with diameter 16 mm. There were no complications, patient responded well to the therapy and her recovery was uneventful. She was followed up for several months and no symptoms and complains of dysphagia were observed no more. The patient had an uneventful postoperative course and remains symptom-free after a follow-up of twenty months.
Figure 2: Chest X-ray and modified barium swallow.
Figure 3: CT scan of the thorax showed the right aortic arch with the left subclavian artery with the constricted esophagus.
RSCA – right subclavian artery
LSCA – left subclavian artery
Figure 4: MRI scans of the thorax showed the right aortic arch with the left subclavian artery with the constricted esophagus.
Figure 5: 3D reconstructions of the vessels.
a) anterior view, b) posterior view
The case was presented because of the following causes:
• Dysphagia in young adults is rare discussed – Roden`s analysis of 2511 articles revealed that about two thirds of the published literature on dysphagia represents adults older than 50 years[13]
• The vascular abnormality is not typical / characteristic cause of dysphagia in young adults – in adolescence it is associated usually with acute and chronic upper respiratory diseases in the late years with reflux, Somatic left subclavian artery is a really rare cause of dysphagia.
• Dysphagia is a multidisciplinary problem and wide differential diagnosis is needed and cooperation of different specialists is helpful to make a proper diagnosis.
Discussion
A retro esophageal course of the right/left subclavian artery is referred to as “arteria lusoria”. It may be related to severe compression of the trachea and esophagus, typically resulting in impaired swallowing and dyspnea[4,5]. However, it is not a common cause of dysphagia. An aberrant LSCA in patients with a right-sided aortic arch occurs in about 1/1000 of the general population[6]. While about 10 % of adults with the most common embryological abnormality of the arch - an aberrant right subclavian artery (0.5 - 2% of the population) is symptomatic (dysphagia, dyspnea), there are only a few papers about symptomatic aberrant left subclavian artery with right-sided aortic arch in adult patients[4]. In such cases, the so-called dysphagia lusoria is observed - dysphagia secondary to an aberrant right/left subclavian artery that has a retro esophageal course[7]. Two-thirds of individuals with a retro esophageal (Aberrant) Right Subclavian Artery (ARSA) are believed (on the basis of autopsy studies and retrospective studies) to remain completely asymptomatic despite the anomaly[7]. Our patient was a young woman with vascular anomaly diagnosed because of dysphagia and odynofagia; symptoms had appeared two years before hospitalization. Dysphagia can occur at any age. However it is usually treated as a problem that affects the elderly population. The mean age of patients with dysphagia in Hoy’s paper was 62 years, while in Roden systematic review of the literature on dysphagia almost two-thirds of the published literature described adults over 50 years of age[1]. According to Barci, oropharyngeal dysphagia is present an as many as 35% of the population older than 75 years[8]. Although most cases of these anomalies are asymptomatic, severe congenital aortic arch failures are already symptomatic in childhood[5]. Difficulty breathing and/or swallowing or/ and pain in the chest and/or odynophagia are the most common complaints forcing patients to visit the doctor’s office[4,5,7]. Other common problems related to difficulty of swallowing include tongue-thrust, prolonged and strongly exaggerated bite reflex, hypersensitive gag reflex, sialorrhoea (drooling), tactile hypersensitivity in the oral area (almost oral defensiveness), coughing during swallowing, frequent choking and pneumonia[9,10]. There are some possible mechanisms as to why certain individuals become symptomatic: increased esophageal rigidity with ageing, aortic elongation with ageing, aneurysm formation, and the presence of a bicarotid trunk[7].
In the presented case no more additional pathologies were observed, so the first two reasons are the most probable cause. Because of the woman’s medical history, residual Cerebral Palsy (CP) was also suspected as the cause of her problem with swallowing. Dysphagia is connected with three major pathologies associated with cerebral palsy namely poor lingual function, delayed swallow reflex initiation and poor primary peristaltic wave[11]. Cerebral palsy is a heterogeneous condition, but in most cases significant feeding and swallowing problems are observed already in childhood - especially during the first 12 months of life[11]. Although the condition is not progressive its effect are permanent and observed also in adults. People with CP are prone to aspirate oral and gastric contents, which cause respiratory complications such as Gastro Esophageal Reflux Disease (GERD), and more than 90% have an oral-motor dysfunction. The incidence of dysphagia in children with CP is estimated to be about 40%, gastro-oesophageal reflux problems are estimated to affect 75%[11,12]. Abnormal responses such as the bite reflex, suckle-swallow reflex, lack of tongue lateralization, instability of the lower jaw can severely limit the ability to chew and swallow food bolus[13]. Cerebral palsy cannot be cured, but the dysphagia symptoms can be eliminated utilizing intensive therapy, food consistency management and positioning techniques. So the proper diagnosis is important for the trapeutic process.
Myasthenia gravis was also suspected as a neurologic disease often affecting swallowing. Moreover most patients usually present with voice problems such as: dysarthria or open nasality. Muscles of facial expression, mastication and swallowing are the most frequently involved (just after ocular muscles). Swallowing is affected when the muscles of mastication and pharyngeal muscles fatigue as a result of repetitive muscle contraction. Thus, approximately 20% - 30% of patients with myasthenia have dysphagia[13]. It is oropharyngeal rather than esophageal dysphagia. The disease was excluded thanks to several tests and investigations conducted on the patient; moreover, her complaints and symptoms indicated the lower, retropharyngeal dysphagia. Differential diagnosis should be performed with some neurologic diseases in each case of dysphagia. Many neurological disorders have been shown to cause dysphagia [table 1]. Literature even mentions the term “neurological dysphagia”, which refers to difficulty swallowing/eating as a result of a neurological disease[13]. Certain neurogenic dysfunctions can impair both the esophageal and oropharyngeal functions, but in most cases problems related to oropharyngeal dysphagia tend to be predominant. Results of recent studies strongly suggest that GERD is a major cause of globus pharynges as well as the main cause of dysphagia in young adults. Moreover, as mentioned earlier, GERD often occurs with cerebral palsy[1,14]. Because of the patient’s age, medical history of CP, and the redness of the larynx in laryngoscopy there was a strong suspicion of GERD in the young woman, but gastroscopy was performed twice to exclude this condition in the end.
A fast screening test in dysphagia is the water swallow test, which provides a good initial drinking as well as any associated symptoms such as coughing and changing voice (moist) are recorded. The test was negative in our patient, there were no problems with initiating swallowing, but she complained of feeling a lump in the throat. Apart from descreet redness the structure and function of the oral cavity and the larynx together the vocal cords was normal in the phoniatric assessment, slight left facial paralysis had no impact on the swallowing and chewing movements or articulation. That is why the patient was suspected of a psychogenic disease at first. The most important evaluation (the gold standard) in dysphagia is still video fluoroscopy. Despite that, radiological examinations of the esophagus with barium are often useful in the diagnostic process, especially that of retropharyngeal / esophageal dysphagia. To visualize the arch anatomy digital Subtraction Angiogram, CT with contrast, or MRI make the diagnosis possible. The majority of symptomatic patients with arteria lusoria have benefited from surgical intervention such as resection and reconstructive bypass surgery. Janssen et al. concluded that in the absence of another cause of the symptoms and after a trial of medical management, surgery should be considered[15]. In 1994, Kieffer et al. reported on 19 patients who underwent surgery, of whom 16 had a complete resolution of their symptom[16].
In the presented case, embolization of the left subclavian artery was the alternative treatment. Improvement was observed after the intervention – the follow-up is now 14 months. The differential diagnosis of dysphagia depends on the location of symptoms and the patient’s age. Because of affected phase, oral/pharyngeal or esophageal dysphagia is diagnosed. It is worth knowing that oropharyngeal dysphagia has neurological in 80% and structural background in 20% of the cases, while the reasons of the esophageal dysphagia are observed in the reverse proportions. The most common etiologies of dysphagia in different age groups are as followed: infancy is associated with neurodevelopmental delay, childhood and adolescence is associated with pharyngitis, young adult to middle age is associated with predominantly GERD, older adults are at significantly higher risk because of medical comorbidities and neurodegenerative disease as Altman claimed[1].
References
- 1. Altman, K.W. Dysphagia: Diagnosis and Managenent. (2013) Otolaryngologic Clinics of North America 46(6): 924.
Pubmed || Crossref || Others - 2. Szacka, K., Sznajder, J., Jó?wiak, E., et al. Zaburzenia po?ykania w stwardnieniu bocznym zanikowym: patogeneza, diagnostyka i leczenie. (2014) Neurologia praktyczna 3(78): 7-16.
Pubmed || Crossref || Others - 3. Rapp, C.E., Torres, M.M. The Adult with Cerebral Palsy. (2000) Arch Fam Med 9(5): 466-472.
Pubmed || Crossref || Others - 4. Czekajska-Chehab, E., Uhlig, S., Sta?kiewicz, G., et al. Arteria lusoria in patients with a normal and a right-sided aortic arch diagnosed with multi-slice computed tomography: a report of two cases. (2007) Folia Morphol 66(1): 74-77.
Pubmed || Crossref || Others - 5. Carrizo, G.J., Marjani. M.A. Dysphagia Lusoria Caused by an Aberrant Right Subclavian Artery. (2004) Tex Heart Inst J. 31(2): 168–171.
Pubmed || Crossref || Others - 6. McNally, P.R., Rak, K.M. Dysphagia lusoria caused by persistent right aortic arch with abberant left subclavian artery and diverticulum of Kommerell. (1992) Dig Dis Sci 37(1): 144-149.
Pubmed || Crossref || Others - 7. Rogers, A.D., Nel, M., Eloff, E.P., et al. Dysphagia Lusoria: A Case of an Aberrant Right Subclavian Artery and a Bicarotid Trunk. (2011) ISRN Surgery (2011): 6.
Pubmed || Crossref || Others - 8. Barci, S.R., Sullivan, P.A., Robbins, J. How should dysphagia care of older adults differ? Establishing optimal practice patterns. (2000) Semin Speech Lang 21(4): 347-361.
Pubmed || Crossref || Others - 9. Field, D., Garland, M., Williams, K. Correlates of specific childhood feeding problems. (2003) J Paediatr Child Health 39(4): 299-304.
Pubmed || Crossref || Others - 10. Czernuszenko, A., Litwin, M., Zaborski, J. Patofizjologia i konsekwencje kliniczne dysfagii neurogennej. (2014) Neurologia praktyczna 4(79): 23-28.
Pubmed || Crossref || Others - 11. Gerek, M., Çiyiltepe, M. Dysphagia management of pediatric patients with cerebral palsy. (2005) British Journal of Developmental Disabilities 51(100): 57-72.
Pubmed || Crossref || Others - 12. Erasmus, C.E., Hulst, K., Rotteveel, J.J. et al. Clinical practice: Swallowing problems in cerebral palsy. (2012) Eur J Pediatr 171(3): 409-414.
Pubmed || Crossref || Others - 13. Perlman, A.L., Schulze-Delrieu, K. Deglutition and Its Disorders. (1997) Singular Publishing Group 42(2): 522.
Pubmed || Crossref || Others - 14. Lee, B.E., Kim, G.H. Globus pharyngeus: A review of its etiology, diagnosis and treatment. (2012) World J Gastroenterol 18(20): 2462–2471.
Pubmed || Crossref || Others - 15. Janssen, M., Baggen, M.G.A., Veen, H.F., et al. Dysphagia lusoria: clinical aspects, manometric findings, diagnosis, and therapy. (2000) Am J Gastroenterol 95(6): 1411–1416.
Pubmed || Crossref || Others - 16. Kieffer, E., Bahnini, A., Koskas, F. Aberrant subclavian artery: Surgical treatment in thirty-three adult patients. (1994) J Vasc Surg 19(1): 100–111.
Pubmed || Crossref || Others