Efficacy of laparoscopic sleeve gastrectomy on type 2 diabetes with BMI less than 35: a retrospective study
Padmakumar Ramakrishnapillai1*, Madhukara Pai1, Farish Shams1, Rajeev Jayadevan2, Praveen Kumar3, Shaji P.G4, Anithadevi T Sathyan5, Sulfia Jabbar3, Vani Krishna6, Premna Subin1
Affiliation
- 1Department of Laparoscopic and Metabolic Surgery, Sunrise Hospital, Kakkanad, Kochi 682030, India
- 2Department of Gastroenterology, Sunrise Hospital, Kakkanad, Kochi 682030, India
- 3Department of Diabetology, Sunrise Hospital, Kakkanad, Kochi 682030, India
- 4Department of Anesthesiology, Sunrise Hospital, Kakkanad, Kochi 682030, India
- 5Department of Bio-statistics, Sunrise Hospital, Kakkanad, Kochi 682030, India
- 6Department of Dietetics, Sunrise Hospital, Kakkanad, Kochi 682030, India, Data collection and compilation
Corresponding Author
Ramakrishnapillai Padmakumar, Consultant Surgeon, Department of Laparoscopic and Metabolic Surgery, Sunrise Hospital, Seaport-Airport Road, Kakkanad, Kochi 682030, India, Tel: +91-944-7230370; Fax: +91-484-2428917; E-mail: drrpadmakumar@gmail.com
Citation
Padmakumar R., et al. Efficacy of Laparoscopic Sleeve Gastrectomy in Type 2 Diabetes Even With BMI Less than 35: A Retrospective Study. (2015) J Diabetes Obes 2(1): 38- 42.
Copy rights
© 2015 Padmakumar R.P. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Abstract
Objective: To evaluate the effectiveness of Laparoscopic Sleeve Gastrectomy (LSG) for resolving type 2 diabetes in obese patients even with BMI < 35 kg/m².
Methods: A retrospective study was conducted on 90 type 2 diabetic patients with BMI > 30 kg/m² who underwent LSG at Sunrise Hospital, Kochi, India, from September 2009 to February 2014. In this study, we compared preoperative parameters such as BMI, HbA1c and diabetic medications with postoperative parameters during periodic reviews.
Results: Complete resolution of type 2 diabetes found in 86.6%, 91.1%, and 88.4% in patients with obese class I, II & III respectively. The complete resolution of diabetes (F = 0.421, P = 0.658) and drop in HbA1c (F = 0.172, P = 0.842) among the BMI groups were statistically not significant, i.e. class I obese patients were equally benefited compared to class II and class III obese patients. Co-morbidities also resolved to a good extent; sleep apnea 100%, fatty liver 89.47%, dyslipidemia 88.57%, polycystic ovarian disease 83.33% and hypertension 82.22%. Minor complications were reported in 3.84%, whereas no complications in 96.16% of the patients.
Conclusion: Laparoscopic sleeve gastrectomy was found to be an effective intervention for obese type 2 diabetic patients, even when BMI is 30-34.9 kg/m².
Introduction
Type 2 diabetes makes up about 90% of cases of diabetes while the other 10% are primarily due to diabetes mellitus type 1 and gestational diabetes[1]. Insulin resistance and beta cell failure are the prime causes of type 2 diabetes in people who are genetically predisposed to the disease. Obesity is a major independent risk factor for the development of type 2 diabetes and is associated with the rapid increase in the prevalence of type 2 diabetes[2]. It was found in a study that the majority (68%) of the type 2 diabetes subjects were obese[3]. In comparison with subjects having BMI < 25 kg/m², the relative prevalence of diabetes was about 1.25 times among subjects with BMI between 25 to 29.9 kg/m², and was elevated about 2.5 times among subjects with BMI>30 kg/m²[4]. Another study quotes that never-obese individuals were 60 times less likely to have diabetes than those with incident obesity[5].
Laparoscopic sleeve gastrectomy (LSG) is a well established bariatric procedure of treatment for people who are obese and having type 2 diabetes, not achieving desirable control with medical and dietary therapies, especially when there are other major co morbidities. It has shown to dramatically improve glycemic control, leading to complete resolution of type 2 diabetes in the majority of patients, as well as reduction of excess weight[6]. In India, 61.3 million people had been diagnosed with diabetes in 2011 as per International Diabetes Federation (IDF) and are expected to rise dangerously to 101.2 million by 2030. India holds second place, next to China in having the high prevalence of diabetes[7]. In this circumstance, this procedure is of great importance in offering a complete resolution for majority of type 2 diabetes patients.
A systematic review assessing the resolution or improvement in type 2 diabetes mellitus after LSG showed that 66.2% had complete resolution and 26.9 % improved/resolved from diabetes[8]. As per the IDF guidelines, bariatric surgery is an option for T2DM patients with BMI > 35 kg/m² or more. In patients with BMI between 30-34.9 kg/m² when diabetes cannot be adequately controlled by optimal medical regimen, and in presence of comorbidities, surgery should be considered as an alternative treatment option. In Asians the BMI action point is still lower, i.e. BMI 27.5 kg/m² [9]. So our aim was to assess the effectiveness of LSG in patients with BMI 30-34.9 kg/m² and compare the same with that of patients with BMI > 35 kg/m².
Materials and Methods
This is a retrospective study conducted on 90 type 2 diabetic patients with BMI > 30kg/m² who underwent laparoscopic sleeve gastrectomy (LSG) and were available for follow-up at Sunrise Group of Hospitals, Kochi, India, from September 2009 to February 2014. In order to get 80% power at 5% significance level with 70% of complete diabetes resolution, we needed a minimum of 84 subjects to be studied. Preoperative parameters such as BMI, HbA1c & diabetic medications were compared with those during periodic postoperative reviews at 1 month, 3 months, 6 months and 12 months, to check the resolution rates of diabetes.
Inclusion criteria for the study were type 2 diabetic patients (HbA1c > 6.5%) with BMI > 30 kg/m² who underwent LSG. The study excludes, patients with lower BMI (i.e. BMI < 30 kg/m²), patients who were obese but non-diabetic and those who underwent other procedures like gastric bypass, Ileal interposition or revision of bariatric surgeries.
The patients who attained HbA1c level < 6.5% without any diabetic medications were considered as complete resolution. Diagnosis of sleep apnea and its resolution were based on patient statements. Diagnosis of fatty liver and its resolution were based on ultrasonographic findings. Diagnosis of hypertension and its resolution were based on clinical assessment and discontinuation of antihypertensive medications. The patients were asked to follow up at specified intervals and thus the study follow-up was conducted. Follow-up data from overseas patients who could not meet in person were obtained through emails.
Initial Assessment
All the patients underwent a thorough clinical evaluation by a team of doctors including bariatric surgeon, diabetologist, cardiologist, anaesthesiologist, pulmonologist, dietician and diabetes educator. An enquiry regarding duration of type 2 diabetes and other obesity related co morbidities like hypertension, sleep apnea, fatty liver, dyslipidemia, polycystic ovarian disease and infertility were done. The medications that the patients were taking were also recorded. A physical examination to look for acanthosis nigricans, abdominal wall herniation, abdominal and arm sagging was done.
Indications for LSG
• Obese class II and obese class III patients
• Obese class I patients with obesity related co-morbidities that could not be controlled with medicines.
• Patients failed to lose weight with conservative modalities
Contra indications for LSG
• Patients with age group < 15 and > 65 years
• Chronic liver diseases
• Major cardiovascular diseases that cause a high risk for anaesthesia
• Drug or alcohol abuse currently
• Uncontrolled psychiatric illness and lack of comprehension of the risks-benefits
Preoperative care
The medical conditions of the patients were stabilized to the maximum that is possible. They were counselled regarding the restriction of diet after procedure and probable complications including gastric leak and hair loss. They were admitted a day prior to the surgery and were kept on liquid diet for 24 hours. Preoperative antibiotics were given as per recommendations and proper consent for surgery obtained.
Operative technique
The procedure was done using a 5 port technique. The 1st port (12 mm) was placed towards left of midline well above umbilicus and the 2nd port (10 mm) was placed towards the left of it. Three 5-mm ports were placed at the right hypochondrium, right midclavicular line and left anterior axillary line respectively. Greater omentum was divided close to stomach along the greater curvature, preserving epiploic arcade towards the omentum. A 38F bougie was placed per-orally and under its guidance stomach was divided 3-5 cm proximal to pylorus. Thus using endostaples, a narrow stomach tube was created and entire fundus was resected. Methylene blue dye was instilled to check gastric leak.
Postoperative care
Oral clear fluids were initiated after 24 hours. Tight control of diabetes was maintained in the postoperative period with insulin as and when required. The patients were ambulated within 8 hours and chest physiotherapy was initiated along with leg exercise. Low molecular weight heparin for DVT prophylaxis, antibiotics and analgesics were administered. On the day of discharge the diet chart and diet counselling were given. For 2 weeks the patients were kept on clear-liquid diet like green tea or any herbal tea, black tea, clear vegetable soup, buttermilk, etc., and were asked to take small quantities of liquids frequently. Vitamin supplements and proton pump inhibiters were also provided to the patients. After two weeks vegetable based diet was initiated followed by normal diet in a month’s time. Vitamin supplement discontinued in two month’s time.
Statistical Analysis
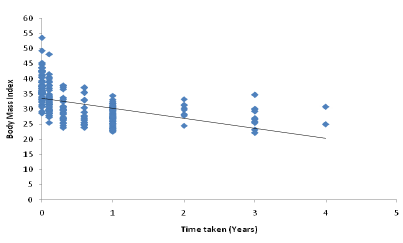
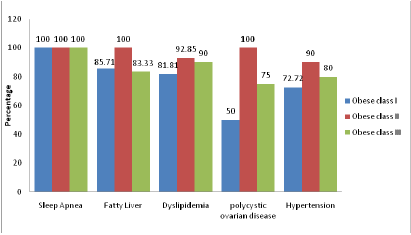
There were 90 patients having BMI>30 kg/m², who underwent LSG. The subjects were classified in three groups based on the guidelines provided by World Health Organization (WHO) i.e. obese class I- BMI 30-34.9 kg/m², obese class II - BMI 35-39.9 kg/m², and obese class III - BMI > 40 kg/m², for studying the characteristics of the data. Descriptive statistics were computed on continuous variable, age. The sex ratio was also calculated. Scatter plot was used to study the variation in BMI with time for the whole population. The proportion of patients having complete resolution of diabetes, improved but not fully resolved and sustained medical conditions were calculated. Of the 90 patients, 61 patients who completed 1 year were included in comparing the preoperative HbA1c and 1 year postoperative HbA1c values. Difference in the mean preoperative HbA1c and the mean postoperative HbA1c were computed using paired t-test, p-value < 0.05. The differences among the BMI groups were analyzed using one way ANOVA. The percentages of comorbidities resolved were presented graphically using multiple bar diagram. All the statistical analysis was carried out using Statistical Package for Social Sciences (SPSS) version 19.1 and Microsoft office Excel 2007.
Results
The study population consisted of 90 diabetic patients. The mean age of the patients was 43 yrs, ranging from 20 to 63 yrs. The weight of the overall population ranged from a minimum of 63 kg to a maximum of 168 kg. Height varied from 149 cm to 187 cm and BMI ranged a minimum of 30.12 kg/m² to a maximum of 53.62 kg/m², giving a mean of 37.58 kg/m², which decreased to 27.6 kg/m² within a year. Duration of diabetes was found to be an average of 5 years with range 1 month to 19 years. The blood parameters were, fasting insulin: 25.21 Uu/Ml (mean), fasting c-peptide: 4.04 ng/ml, serum cortisol: 11.27 ug/dL and FBS: 159.57 mg/dl. Eighty four percent of patients were on diabetic medications (Table 1). The reducing trend of BMI during follow-up is shown in the scatter plot. The mean BMI was noted to be 37.16 kg/m² in the preoperative period and 32.91 kg/m², 29.53 kg/m², 28.52 kg/m², 27.74 kg/m², 27.65 kg/m², 27.42 kg/m² and 26.87 kg/m² at postoperative periods of 1st month, 3rd month, 6th month, 1 year, 2 year, 3 year and 4 year respectively (Figure 1).
Figure 1: Variation in BMI with times
Table 1: Baseline and demographic characteristics of the population
| Variables | Levels of BMI | |||
|---|---|---|---|---|
| Obese class I(n = 30) | Obese class II(n = 34) | Obese class III(n = 26) | ||
| Age (Mean ± S.D) | 45.69 ± 9.44 | 43.74 ± 9.32 | 38.14 ± 12.88 | |
| Gender | Male | 10 | 10 | 12 |
| Female | 20 | 24 | 14 | |
| BMI (kg/m²) (Mean ± S.D) | 32.21 ± 1.75 | 37.03 ± 1.43 | 43.52 ± 3.16 | |
| Mean duration of diabetes (years) | 4 | 7 | 5 | |
| *On diabetic medication n(%) | 26 (86.6%) | 29 (85.29%) | 21 (80.76%) | |
BMI: Body Mass Index; SD: Standard Deviation
* Diabetic medications includes oral hypoglycemic agents (OHA), insulin or both.
The mean preoperative HbA1c for the whole population was 8.26%, while the mean postoperative HbA1c one year after surgery was 6.11%. The difference between the mean preoperative and 1 year postoperative HbA1c values was significant with (t = 10.242, P < 0.001). Mean HbA1c reduced to 6.06, 6.21 and 6.08 in the three BMI groups, (t = 2.73, P = 0.014 in obese class I, t = 5.41, P < 0.001 in obese class II and t = 5.05, P < 0.001 in obese class III) respectively. It was observed that 88.7% of patients who were having diabetes and were on diabetic medications before surgery achieved complete resolution of diabetes after surgery. Complete resolution of diabetes was found to be 86.6 %, 91.1%, and 88.4% in patients with obese class I, obese class II and obese class III respectively (Table 2). The difference among the values of complete resolution of diabetes in the BMI groups was found to be statistically not significant, (F = 0.421, P = 0.658). Similarly, the drop in HbA1c among the BMI groups was also found to be statistically not significant (F = 0.172, P = 0.842), i.e. class I obese patients were equally benefited when compared to class II and class III obese. The patients in whom diabetes did not resolve had significant reduction in medicine dosage.
Table 2: Preoperative versus postoperative diabetic resolution
| BMI | Number of patients (n) | Mean HbA1c (pre-op) | Mean HbA1c (post-op) | P-value | *Complete resolution n (%) | **Significant improvement n (%) |
|---|---|---|---|---|---|---|
| Obese class I | 30 | 8.26 | 6.06 | 0.014 | 26 (86.6) | 4 (13.4) |
| Obese class II | 34 | 8.34 | 6.21 | < 0.001 | 31 (91.1) | 3 (8.9) |
| Obese class III | 26 | 8.20 | 6.08 | < 0.001 | 23 (88.46) | 3 (11.53) |
BMI: Body Mass Index; HbA1c (Pre-op): Preoperative glycated haemoglobin;
HbA1c (Post-op): Post-operative glycated haemoglobin
*HbA1c < 6.5% without any diabetic medication
**HbA1c coming to normal with significantly reduced dosage of diabetic medication than preoperative period.
Other co morbidities also resolved to a good extent such as sleep apnea 100%, fatty liver 89.47%, dyslipidemia 88.57%, polycystic ovarian disease 83.33% and hypertension 82.22%. The resolution of co morbidities in the obese class I, obese class II and obese class III groups were represented using a multiple bar diagram (Figure 2). Major complications that can lead to death or require a second surgery were not seen in any of the patients in the study. Minor complications like hair loss and gastroesophageal reflux disease were seen in 3.84 % of the patients, no complications were reported in 96.16% of the patients in this study. We have found that the percentage of patients having complete resolution of diabetes in the second year was almost the same as that in the first year of follow-up (Table 3). This shows that the chance of relapse of diabetes is very low.
Figure 2: Co-morbidities resolved (Other than diabetes mellitus)
Table 3: Diabetic resolution during the follow-up
| Follow-up | Number of patients (n) | *Complete resolution of diabetes n (%) | **Significantly improved but not completely resolved n (%) |
|---|---|---|---|
| Up to 12 months | 90 | 80 (80.99) | 10 (11.11) |
| 1 year | 61 | 52 (85.24) | 9 (14.76) |
| 2 year | 21 | 17 (80.95) | 4 (19.05) |
| > 2 year | 5 | 4 (80.00) | 1 (20.00) |
*HbA1c < 6.5% without any diabetic medication
**Significantly improved but not completely resolved: HbA1c coming to normal with significantly reduced dosage of diabetic medication.
Discussion
Laparoscopic sleeve gastrectomy (LSG) is an apparently effective procedure that can achieve resolution of diabetes. It also improves other obesity-associated co morbidities, thereby potentially reducing mortality. In morbidly obese patients, it allows substantial and sustained weight loss[10]. In this study LSG has shown to have successful weight reduction with 65% of desired weight loss in six months period (obese class I: 63%; obese class II: 68%; obese class III: 65%) and it found to be sustained as shown in the other studies. Our focus is on the effectiveness of LSG in resolving type 2 diabetes in obese patients.
This study shows that LSG leads to complete resolution of diabetes mellitus in 88.7% patients and improved/resolved in 100% of patients. It substantiates the previous studies on the effectiveness of LSG in apparently curing type 2 diabetes (HbA1c > 6.5%). J. Ellsmere reported a diabetic resolution rate of 78% after LSG[11].
LSG is generally recommended in patients with BMI > 35 kg/m²[12]. In our observation, complete resolution of diabetes was achieved in 31 out of 34 (i.e., 91.1%) patients with BMI > 35 kg/m² through this method. Hence, our data supports the former study results, in recommending it as an effective tool for resolution of diabetes mellitus in patients with BMI > 35. Interestingly, our study echoed an almost similar success rate (86.6%) in fully resolving diabetes among patients with BMI between 30 and 35 kg/m² also.
The mechanism behind such resolution of diabetes is not fully elucidated. It is likely that some endocrine changes, independent of weight loss, can give rise to remission of type 2 diabetes. All co morbidities resolved considerably after the procedure. This substantiates LSG as a choice for obese type 2 diabetic patients with other co morbidities. There was no death reported after the surgery in this study. Zero percent mortality rates were reported in 16 other studies[13]. There were no major complications reported and incidence of minor complication was 3.84%, mainly gastroesophageal reflux disease, whereas other studies reported 10.3 % chances of complications[13]. There were no complications in the post-operative follow-up in 96.16 % of the patients at Sunrise Hospital.
Limitations of the study include lack of long-term follow-up for obvious reasons. Long-term follow-up data, when eventually available, will be of interest to see the 5, 10 and 20 year remission rates of diabetes in this group of patients. Randomized controlled trials that are long term would give a better picture when eventually available. The results of this study, along with other previously published studies, show that LSG is safe and helps in resolution of diabetes as well as weight reduction
Conclusion
Laparoscopic sleeve gastrectomy is a new procedure for treatment of obesity. It is safe and effective in weight reduction as well as resolution of associated co morbidities especially diabetes mellitus in obese 2 and obese 3 categories. Our study indicates that LSG is effective in obese class 1 group as well.
Acknowledgement
We are extremely thankful to Dr. Hafeez Rahman, Chairman and Ms. Parveen Hafeez, Managing Director Sunrise Group of Hospitals, Kakkanad, Cochin, India, for permitting us to conduct this study. We are thankful to Bincy A Sam, Head of the Department of Medical records for providing the details of the patients. There were no conflicts of interest. We also thank all the patients who participated in the study.
References
- 1. Norris, S.L., Holmer, H.K., Ogden, L.A., et al. Conflicts of Interest among Authors of Clinical Practice Guidelines for Glycemic Control in Type 2 Diabetes Mellitus. (2013) PLoS One 8(10): e75284.
- 2. Yoon, K.H., Lee, J.H., Kim, J.W., et al. Epidemic obesity and type 2 diabetes in Asia. (2006) Lancet 368 (9548): 1681– 1686.
- 3. Patel, M., Patel, I.M., Patel, Y.M., et al. A Hospital-based Observational Study of Type 2 Diabetic Subjects from Gujarat, India. (2011) J Health Popul Nutr 29(3): 265- 272.
- 4. Murray M.F. The Prevalence of Diabetes among Overweight and Obese Individuals is Higher in Poorer than in Richer Neighbourhoods. (2008) Canadian J Diabetes 32(3): 190- 197.
- 5. Natalie S.T., Andrea S.R., Gordon-Larsen, P. Timing and Duration of Obesity in Relation to Diabetes: Findings from an ethnically diverse, nationally representative sample. (2013) Diabetes Care April 36(4): 865-872.
- 6. Pok, E.H., Lee, W.J. Gastrointestinal metabolic surgery for the treatment of type 2 diabetes mellitus. (2014) World J Gastroenterol 20(39): 14315– 14328.
- 7. Chandini, R. Prevalence of diabetes increases among youngsters in India. (2012).
- 8. Gill, R.S., Birch, D.W., Shi, X., et al. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. (2010) Surg Obes Relat Dis 6(6): 707– 713.
- 9. Dixon, J.B., Zimmet, P., Alberti, K.G., et al. Bariatric surgery: an IDF statement for obese Type 2 diabetes. (2011) Diabet Med 28(6): 628– 642.
- 10. Wang, Y., Zhang, C. Bariatric Surgery to Correct Morbid Obesity Also Ameliorates Atherosclerosis in Patients with Type 2 Diabetes Mellitus. (2009 ) Am J Biomed Sci 1(1): 56– 69.
- 11. Hoogerboord, M., Wiebe, S., Klassen, D., et al. Laparoscopic sleeve gastrectomy: perioperative outcomes, weight loss and impact on type 2 diabetes mellitus over 2 years. (2014) Can J Surgv 57(2): 101- 105.
- 12. Gluck, B., Movitz, B., Jansma, S., et al. Laparoscopic sleeve gastrectomy is a safe and effective bariatric procedure for the lower BMI (35.0-43.0 kg/m2) population. (2011) Obese Surg 21(8): 1168- 1171.
- 13. Anvari, M. Use of Metabolic Surgery for the Treatment of Type 2 Diabetes. (2011) Canadian J Diabetes 35(2): 99- 108.