Extragonadal Germ Cell Tumor in an Older Patient. Not Every Mass is a Lung Cancer
Konstantinos Arnaoutakis2*
Affiliation
- 1Department of Hospital medicine, Cleveland Clinic Campus, Cleveland, Ohio, USA
- 2Division of Hematology and Oncology, University of Arkansas, Little Rock, Arkansas, USA
Corresponding Author
Konstantinos Arnaoutakis, MD, FACP, Assistant Professor of Medicine- Division of Hematology and Oncology/ Associate Program Director, Hematology/Oncology Fellowship, Winthrop P. Rockefeller Cancer Institute, University of Arkansas for medical sciences, 4301 West Markham Street, Slot # 508, Little Rock, Arkansas 72205, United States; Tel: 501-526-6990 x 8064/ Fax: 501-686-6342; E-mail: KArnaoutakis@uams.edu
Citation
Arnaoutakis, K., et al. Extragonadal Germ Cell Tumor in an Older Patient, Not Every Mass is a “Lung Cancer”. (2016) Intl J Cancer Oncol 3(1): 95-98.
Copy rights
© 2016 Arnaoutakis, K. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Lung cancer; beta-HCG; Extragonadal germ cell
Abstract
Background: Extragonadal germ cell tumors are rarely diagnosed beyond the fourth decade of life. Here, we present an unusual case of an older patient with a rapidly growing lung mass and a significantly elevated beta-HCG consistent with an extragonadal germ cell tumor.
Case presentation: A 69 year old male was found to have multiple brain lesions and a lung mass. He was initially diagnosed with stage IV poorly differentiated non–small cell lung cancer. A germ cell tumor was suspected due to its rapid growth and a highly elevated serum beta-HCG was found. Testicular ultrasound was negative for a gonadal mass. AFP was not elevated. There was no isochromosome 12p but there was hyperdiploidy of chromosome 12. He was treated with platinum based chemotherapy. He had an initial transient decline in the beta-HCG levels along with radiographic improvement but the disease progressedrapidly.
Conclusion: Extragonadal germ cell tumors should be suspected in older patients with a lung mass and a rapid tumor progression.
Introduction
Extragonadal germ cell tumors (EGCTs) account for 1–5% of germ cell tumors[1]. The most common site is in the anterior mediastinum and are typically diagnosed in the third and fourth decade of life[2]. It has been hypothesized that EGCTs are either a consequence of a mismigration of germ cells along the urogenital ridge during embryogenesis or they arise from germ cells that are physiologically distributed[3,4]. These are fast growing and clinically may present as chest pain, shortness of breath, cough, weight loss, fever, superior vena cava syndrome or as a mass causing compression of mediastinal structures.The characteristic genetic abnormality that is found is isochromosome 12p[5,6]. EGCTs are positive for tumor markers such as alpha-fetoprotein (AFP) and beta-Human Chorionic Gonadotropin (HCG)[7,8].
Beta-HCG elevation is also seen secondary to ectopic secretion by non- trophoblastic tumor cells[9]. Ithas been reported as a paraneoplastic phenomenon in about 10% of primary lung cancer case[10-14]. Lung cancers with elevated beta-HCG are more resistant to chemotherapy and have poor prognosis.
We present here a case of a lung mass with multiple brain lesions and visceral metastasis in a patient with a significantly elevated beta-HCG suggestive of an extragonadal germ cell tumor.
Case Presentation
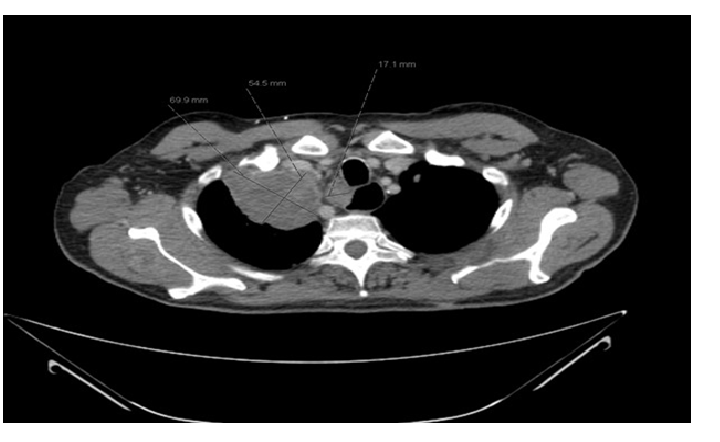
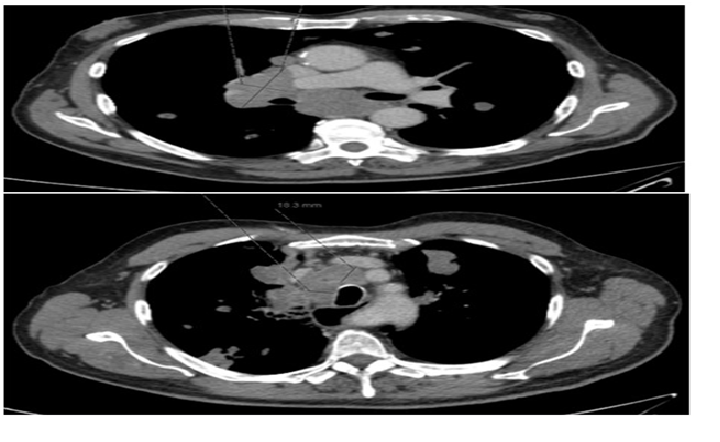
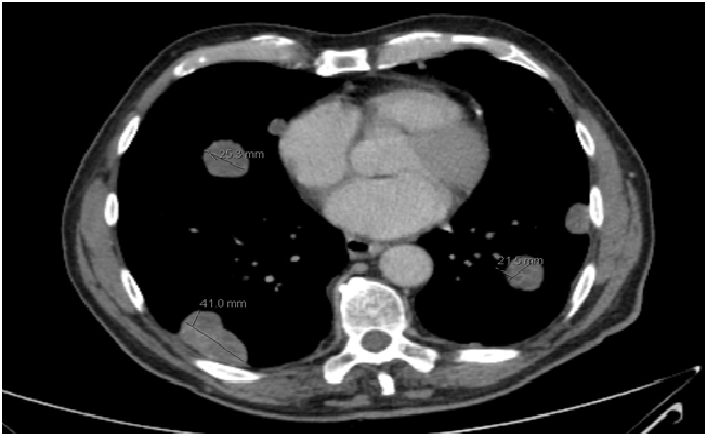
A 69 year old male smoker presented with headache, unsteadiness, disorientation and was found to have a lung mass with multiple brain lesions. His CT scan chest at presentation was significant for a right apical mass of 3.2 cm x 3.5 cm x 3.8 cm size adjacent to mediastinum, contiguous with mediastinal lymphadenopathy (Figure 1). He had enlarged pretracheal, right paratracheal and precarinal nodes and bulky right hilar and subcarinal adenopathy (Figure 2). He underwent resection of the largest brain tumor. Final pathology showed poorly differentiated carcinoma. CK 7 was strongly positive. CK 20 was weakly positive. Cytokeratin 5/6, TTF-1 and synaptophysin were negative. He was diagnosed as stage IV non-small cell lung cancer. Following whole-brain radiation he had a restaging scan that showed progression. CT chest showed increasing right apical soft tissue mass with extensive mediastinal lymphadenopathy and hepatic, renal, and skeletal metastases (Figure 3 - 4). He had a markedly elevated beta-HCG level at 21651.0 mIU/mL (0.0-9.9mIU/mL) and serum AFP was 7.2 ng/ml (0-8.0ng/ml). The testicular ultrasound was negative for gonadal mass. There was no isochromosome 12p but 76% of cells had additional copies of chromosome 12, without apparent gain of 12p.
Figure 1: CT scan Chest with oral and intravenous contrast. A large soft tissue mass is present in the right apex measuring 7 x 5.5 cm with moderate compression of the superior vena cava and multiple metastatic nodules
Figure 2: Extensive mediastinal lymphadenopathy is seen. Multiple paratracheal nodes, subcarinal and conglomerate of nodes in the right and left hilum is seen
Figure 3: Multiple peripherally enhancing hypodense mass lesions seen throughout the liver with heterogenous densities in the kidneys
Figure 4: Large satellite nodules present throughout the lungs measuring between 2 and 4 cm
He completed 4 cycles of platinum based chemotherapy. Follow up CT scan showed significant interval improvement in the mediastinal lymphadenopathy, with decrease in pulmonary and visceral lesions. His beta-HCG decreased to 35.4 mIU/ml after the fourth cycle. However, he continued to have significant burden of residual disease and his beta-HCG started rising. He failed second line treatment with gemcitabine and oxaliplatin and later with gemcitabine and paclitaxel. His beta-HCG level continued to rise despite ongoing chemotherapy with elevation to > 1,000,000 mIU/ml. Repeat CT scan showed innumerable bilateral pulmonary metastatic lesions with largest up to 3.8 cm with marked progression of metastasis. Due to progressive disease, worsening performance status and multiple co-morbidities, palliative care was recommended. The patient passed away 11 months after his initial presentation.
Discussion
The encountered clinical scenario shared many similarities with a primary mediastinal non-seminomatous germ cell tumor (PMNSGCT) except for the patient’s age. The reported median age for PMNSGCT is 30 years[6,13]. The rapid clinical progression in this patient raised the suspicion of a non-conventional case of non-small cell lung cancer which further prompted beta-HCG evaluation. Beta-HCG can be elevated with both trophoblastic and non-trophoblastic tumors. Ectopic secretion of beta-HCG is reported in 20-40% of non-trophoblastic tumors such as gastric, liver, ovarian and lung cancers. It acts as an autocrine or paracrine growth factor by inhibiting apoptosis and probably contributes to tumor progression, chemo-resistance and therefore poor prognosis[11]. Elevation of beta-HCG in lung cancer is rare. It has a reported incidence of 14% in small cell lung cancer and 28% in non-small cell lung cancer[12-19]. The reported elevation of beta HCG in lung cancer is about 20-3000 mIU/ml only. The persistent and very highly elevated beta-HCG in this patient raised a strong possibility of a germ cell tumor even without a traditional isochromosome12p[20]. The hyperdiploidy for chromosome 12 in germ cell tumors is rare but has been described before[21].
In patients with extragonadal tumors, the presence of liver, lung and brain metastasis, a primary mediastinal location, a non-seminomatous histology, and elevated beta-HCG have been recognized as the negative predictors for both progression free survival and overall survival. In the International Germ Cell Cancer Collaborative Group (IGCCCG) database, mediastinal NSGCTs have lower complete remission rate, higher relapse rate and failure of salvage chemotherapy[8]. The studies identified the characteristics such as age older than 30 years, beta-HCG elevation at presentation, metastasis to liver, brain and lung, to independently contribute to the poor overall survival in these patients. Most of these characteristics were identified in this case and have probably contributed to rapid deterioration in our patient.
Treatment for PMNSGCTs usually entails cisplatin-based combination chemotherapy regimens followed by post-chemotherapy surgical resection in cases with radiographic evidence of residual disease. Standard treatment involves four cycles of BEP (Bleomycin, Etoposide, Cisplatin), or alternatively VIP (Vinblastine, Ifosfamide, Cisplatin). Chemotherapy regimens using cisplatin have improved themedian survival to 29 months[7]. The median survival in patients untreated with cisplatin is reported as 4.0 - 6.5 months[22,23]. In a study by Hartmann et al[24], it was observed that the long-term disease-free survival after second-line chemotherapy was only 11% and a mediastinal origin of the NSGCT independently predicted failure of second-line chemotherapy.Patients with rising post-chemotherapy serum tumor markers values have median survival of 9.7 - 11.5 months and overall 1- and 5-year survival rates of 41% and 36%, respectively[25,26]. In the advanced cancers, salvage chemotherapy has achieved only 7% long-term disease-free survival and 39-42% 2-year overall survival from the initial clinical presentation[27,28]. Considering persistent and highly elevated post chemotherapy beta HCG, rapid tumor progression with pulmonary lesions with bulky mediastinal involvement and extra pulmonary metastasis, elderly age and the poor survival despite chemotherapy, the given clinical scenario is less likely to be a case of lung tumor with paraneoplastic syndrome. This case probably represents an unusual manifestation of an extragonadal germ cell tumor in a patient in the 7th decade of life.
Conclusion
The germ cell tumors should be suspected while encountering any predominantly mediastinal mass with a rapid progression, and elevated serum beta-HCG or AFP, to be able to initiate early appropriate therapy and discuss prognosis.
Financial disclosure: None
Conflict of interest: None
References
- 1. Moran, C.A., Suster, S. Primary germ cell tumors of the mediastinum: I. Analysis of 322 cases with special emphasis on teratomatous lesions and a proposal for histopathologic classification and clinical staging. (1997) Cancer 80(4): 681-690.
- 2. Collins, D.H., Pugh, R.C. Classification and frequency of testicular tumours. (1964) Br J Urol 36(Suppl): 1-11.
- 3. Willis, R.A. The borderland of embryology and pathology. (1950) Bull N Y Acad Med 26(7): 440-460.
- 4. Friedman, N.B. The function of the primordial germ cell in extragonadal tissues. (1987) Int J Androl 10(1): 43-49.
- 5. Chaganti, R.S., Houldsworth, J. Genetics and biology of adult human male germ cell tumors. (2000) Cancer Res 60(6): 1475-1482.
- 6. Bokemeyer, C., Nichols, C.R., Droz, J.P., et al. Extragonadal germ cell tumors of the mediastinum and retroperitoneum: Results from an international analysis. (2002) J Clin Oncol 20(7): 1864-1873.
- 7. Takeda, S., Miyoshi, S., Ohta, M., et al. Primary germ cell tumors in the mediastinum: A 50-year experience at a single japanese institution. (2003) Cancer 97(2): 367-376.
- 8. International germ cell consensus classification: A prognostic factor-based staging system for metastatic germ cell cancers. International germ cell cancer collaborative group. (1997) J Clin Oncol 15(2): 594-603.
- 9. Pelosof, L.C., Gerber, D.E. Paraneoplastic syndromes: An approach to diagnosis and treatment. (2010) Mayo Clin Proc 85(9): 838-854.
- 10. Hauber, H.P. Paraneoplastic syndromes in lung cancer. (2011) Pneumologie 65(6): 347-358.
- 11. Iles, R.K. Ectopic hCGbeta expression by epithelial cancer: Malignant behaviour, metastasis and inhibition of tumor cell apoptosis. (2007) Mol Cell Endocrinol 260-262: 264-270.
- 12. Szturmowicz, M., Slodkowska, J., Zych, J., et al. Frequency and clinical significance of beta-subunit human chorionic gonadotropin expression in non-small cell lung cancer patients. (1999) Tumour Biol 20(2): 99-104.
- 13. Vicier, C., Tabouret, E., Tallet, A., et al. Beta HCG secretion by a pulmonary adenocarcinoma. (2013) World J Surg Oncol 11: 228.
- 14. Szturmowicz, M., Wiatr, E., Sakowicz, A., et al. The role of human chorionic gonadotropin beta subunit elevation in small-cell lung cancer patients. (1995) J Cancer Res Clin Oncol 121(5): 309-312.
- 15. Yoshida, J., Nagai, K., Nishimura, M., et al. Secretion of hCG/beta-hCG by squamous cell carcinoma of the lung in a 31-year-old female smoker. (2000) Jpn J Clin Oncol 30(3): 163-166.
- 16. Mehta, H., Bahuva, R., Sadikot, R.T. Lung cancer mimicking as pregnancy with pneumonia. (2008) Lung Cancer 61(3): 416-419.
- 17. Taverne, J., Delourme, J., Dhalluin, X., et al. Should elevated beta-HCG levels be an exclusion criteria in clinical trials? A case report of paraneoplastic secretion associated with lung adenocarcinoma. (2013) Rev Pneumol Clin 69(1): 36-40.
- 18. Khobta, N., Tomasini, P., Garcia, M.E., et al. Beta-human chorionic gonadotropin (HCG) dosage and lung cancer: A pitfall when screening patients for clinical trials. (2012) Bull Cancer 99(11):1065-1068.
- 19. Khattri, S., Vivekanandarajah, A., Varma, S., et al. Secretion of beta-human chorionic gonadotropin by non-small cell lung cancer: A case report. (2011) J Med Case Rep 5:19.
- 20. Carter, B.W., Marom, E.M., Detterbeck, F.C. Approaching the patient with an anterior mediastinal mass: A guide for clinicians. (2014) J Thorac Oncol 9(9 Suppl 2): S102-S109.
- 21. Castedo, S.M., de Jong, B., Oosterhuis, J.W., et al. Cytogenetic analysis of ten human seminomas. (1989) Cancer Res 49(2): 439-443.
- 22. Economou, J.S., Trump, D.L., Holmes, E.C., et al. Management of primary germ cell tumors of the mediastinum. (1982) J Thorac Cardiovasc Surg 83(5): 643-649.
- 23. Dulmet, E.M., Macchiarini, P., Suc, B., et al. Germ cell tumors of the mediastinum- A 30-year experience. (1993) Cancer 72(6): 1894-1901.
- 24. Hartmann, J.T., Einhorn, L., Nichols, C.R., et al. Second-line chemotherapy in patients with relapsed extragonadalnonseminomatous germ cell tumors: Results of an international multicenter analysis. (2001) J Clin Oncol 19(6):1641-1648.
- 25. Radaideh, S.M., Cook, V.C., Kesler, K.A., et al. Outcome following resection for patients with primary mediastinal nonseminomatous germ-cell tumors and rising serum tumor markers post-chemotherapy. (2010) Ann Oncol 21(4): 804-807.
- 26. De Latour, B., Fadel, E., Mercier, O., et al. Surgical outcomes in patients with primary mediastinal non-seminomatous germ cell tumours and elevated post-chemotherapy serum tumour markers. (2012) Eur J Cardiothorac Surg 42(1): 66-71.
- 27. Saxman, S.B., Nichols, C.R., Einhorn, L.H. Salvage chemotherapy in patients with extragonadal nonseminomatous germ cell tumors: The Indiana University experience. (1994) J Clin Oncol 12(7): 1390-1393.
- 28. Walsh, G.L., Taylor, G.D., Nesbitt, J.C., et al. Intensive chemotherapy and radical resections for primary nonseminomatous mediastinal germ cell tumors. (2000) Ann Thorac Surg 69(2): 337-343.