Family members of Muslim patients with chronic illness and their attitudes towards life sustaining treatments
Farideh Razban, Sedigheh Iranmanesh
Affiliation
- Nursing Research Center, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
- Alborz University of Medical Sciences, Karaj, Iran
Corresponding Author
Mohammad Esmaeili Abdar M.Sc, Alborz University of Medical Sciences, Karaj, Iran, E-mail: mesmaeli87@gmail.com
Citation
Mohammad Esmaeili Abdar., et al. Family Members of Muslim Patients with Chronic Illness and their Attitudes towards Life Sustaining Treatments. (2016) J Palliat Care Pediatr 1(2): 28- 33.
Copy rights
© 2016 Iranmanesh, S. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Chronic illness, Family members, Attitude, Life sustaining treatments, South East Iran, Muslim
Abstract
Objective: Health care personnel need to be fully aware of public attitude towards Life Sustaining Treatments (LST), to know how to deal with individuals and family members from diverse cultural groups in this topic. This study was conducted to evaluate chronic patient’s family member’s attitude towards life sustaining treatment in South East Iran.
Method: Ethnicity and Attitudes toward Advance Care Directives Questionnaire was used to examine the attitude of 147 chronic patient’s family members toward LSTs in South East Iran.
Results: participants had a moderately positive attitude towards general use of LSTs (mean: 3.69 ± 0.54 out of 5). Findings indicated that married persons had a more personal desire for LSTs compared to single individuals. Persons with higher levels of education showed less positive attitude towards LSTs compared to those with lower levels of education.
Significance of Results: A globally and suitable strategy about how to withdraw and withhold LST may not be accepted by the general public and may not be appropriately established since these issues well understood by each person through public education.
Introduction
Death is inevitable for every human being. Humans naturally avoid death since it accompanies with pain, loss of control, loneliness and because of separation from loved ones and everything that is meaningful to him/her and the fact that we are no longer exists[1]. Hence, human has always been trying to postpone death for as long as possible, especially following the Second World War, advances in medical technology and pharmacy techniques make human unable to sustain human life[2]. Life sustaining treatments (LSTs) defined as “treatment which is intended to sustain or prolong life and that supplants or maintains the operation of vital bodily functions that are incapable of independent operation”[3]. These include “high tech” measures such as renal dialysis, ventilators and organ transplantation, as well as less technically advanced delivered through enteral tubes or intravenous means and chemotherapy[4]. Although, LSTs make human enable to push the limits of life further and further and extend life, but the same advances trapped patients in dying[5]. People in hospitals are sometime kept physically alive almost regardless their condition. It is as if they must be kept alive at all costs[6]. Consequently, patients were not acknowledged, they died at institutes not at their home and their sufferings were prolonged[7]. So, it is opposed to, on one hand never start treatment (withholding) and on the other, treatment that has been started should be stopped (withdrawing)[8]. Withholding and withdrawing treatment is “the waiving of life sustaining treatment that the patient or surrogate does not desire because of a perceived disproportionate burden on the patient or family member or for other reason”[9]. For those whose religion emphasizes the sanctity of life, a view limiting LSTs is inconsistent with that belief[10] and a debate to the tension between addressing “quality of life” and “sanctity of life” will provoke[11]. For appropriate end of life decision making health care providers need to know dying patients and their families understanding and attitudes towards LSTs to appreciate and address them.
The withholding and withdrawing life sustaining treatments is based on principles that are global in nature and different countries should implement them as a guide; although there are some cultural and religious differences[12]. So it seems necessary to consider socio-cultural and religious issues related to death, dying and withholding and withdrawing life sustaining treatments in Iran. Iran, as one of the most ancient world civilizations, is part of Middle East culture. According to World Health Organization in 2013, the total population of Iran is approximately 77.4 million people and life expectancy has risen to 72 years in men and 76 years among women[12]. The overwhelming majority of Iranians (98%) are Muslims and 89% of them adhere to Shia Islam. According to Zahedi et al.,[14] Muslims religious believe that death does not happen except by God’s permission, as dictated in the Quran: “it is not given to any soul to die, but with the permission of Allah at an appointed time”[14]. In Islam, life is sacred. The saving of life is a duty and the unwarranted taking of life is a grave sin[15]. For Muslims everything possible must be done to prevent premature death, but when medical experts believe death is inevitable and it is determined that treatment will not improve the patient condition or quality of life, withdrawal of withholding treatment is acceptable[16]. Withholding life-sustaining treatment is accepted by most of Muslims based on the “Do no harm” principle, and they believe that they are obligated to do whatever is in their power to treat a life-threatening illness[17].
Reviewing literature revealed that some previous study examined attitudes of Korean American and Mexican American older adults[10], Chinese older persons[18], UK general public[19], ambulatory African American or Caucasian patients[20], Chinese teacher’s[21] and different ethnic groups who was living in America[22] towards LSTs. They reported a general positive attitude towards the limited use of life-sustaining treatment for a good death[10,18-21]. Bayer et al., and Ko et al., mentioned that there was a significant difference in participant’s attitude regarding LSTs based on their ethnicity and race. Reviewing literature indicated that Razban et al.,[23] evaluated the attitude of critical care nurses towards LSTs in South East Iran. They reported that although a majority of critical care nurses (77%) did not have the personal desire for use of LSTs including CPR and mechanical ventilation, they had moderately negative to neutral attitude towards general use of LSTs. Also in Iran, some studies evaluated nurse’s[24], nursing student’s[25] and medical student’s[26] attitude towards do not resuscitate (DNR) orders. They reported that in many key items participants showed negative attitude towards DNR orders[24-26]. This study was conducted to evaluate chronic patient’s family member’s attitude towards life sustaining treatment in South East Iran.
Methods
Design
A Cross-sectional descriptive survey was used in this study to examine attitudes towards LST among family members of chronic patients that referred to Ali-ebnAbitaleb hospital in South-East of Iran. Prior to the collection of data approval was obtained from Rafsanjan University of Medical Sciences and head of Ali-ebnAbitaleb hospital.
Sample and Setting
A convenience sample of chronic patients’ family members referred to Ali-ebnAbitaleb hospital enrolled in the study between January and March 2013. Ali-ebnAbitaleb is a general hospital with 300 beds, supervised by Rafsanjan University of Medical Sciences in Rafsanjan, South East Iran[27]. Participants consist of family members of hospitalized people aged 60 years or above, with chronic illness requiring continuing medical care. The chronic diseases that contained within the ten leading causes of death worldwide, as reported by WHO (2014), were considered in this study. Family member of patients with the following chronic conditions were included in this study: COPD, stroke, ischemic heart disease, hypertensive heart disease, lung cancer and diabetes mellitus. Individuals who were older than 18 years included in this study. The exclusion criteria were non-Iranian tourists or individuals unable to complete the questionnaire due to perceptual difficulties. Family members of patients with cognitive impairment, suffering from mental illness or in unstable condition (e.g. vital signs or haemodynamically unstable) were excluded. A target sample size of 123 was calculated to evaluate chronic patient’s family member’s attitude towards life sustaining treatment in South East Iran, at an α = 0.05.
Background Information
First, a questionnaire was designed to obtain background information which was assumed to influence attitudes towards life sustaining treatments. It was developed based on two categories including: (1) personal characteristics like gender, age, marital status, and education (2) religiosity index consist of intrinsic (belief in God) and extrinsic (attendance at religious services and activities) religiosity.
Instrument
To fulfill the aim of the study, a translated version of the “Ethnicity and Attitudes toward Advance Care Directives Questionnaire” was used. This questionnaire designed by Blackhall et al in 1999. It consist of two sections: (1) attitude toward use of life sustaining/prolonging technology (general attitude), and (2) personal desire for use of life support (personal desire). The `general attitude’ was assessed through 13 items each measured by a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Six items worded `positively’ (in favor of life sustaining/prolonging technology) and seven items worded `negatively’ (opposed to life sustaining/prolonging technology). Thus, the scores of negative items were reversed. The mean score greater than 3 indicated positive attitudes and the mean score less than 3 indicated negative attitudes. The second part (`Personal desire’) consists of 8 items in four different hypothetical situations. For the four items related to Cardiopulmonary Resuscitation (CPR), three response choices were given (want, don’t want, and not sure). For the four items related to mechanical ventilation, four response choices were given (want, don’t want, not sure, and for a short time only).
For translation of the questionnaires from English into Farsi, the standard forward– backward procedure was applied. Translation of the items and the response categories was independently performed by two professional translators. Afterward, they were back-translated into English, and, after a careful cultural adaptation, the final versions were provided. Translated questionnaires went through pilot testing. Suggestions from family members of the patients were combined into the final questionnaires versions.
Validity and reliability
Blackhall et al.,[22] reported acceptable internal (construct and content) and external validity (including extensive pilot testing) for this instrument. Also Ko et al.,[10] computed Cronbach’s alpha for the scale with the sample of Korean and Mexican Americans and it was 0.89. In Iran, no study was found that assess the reliability and validity of this scale, so the validity and reliability of the scale was rechecked. The validity of the scale was assessed through a content validity. Ten Faculty members in Nursing and Midwifery School, who were Moslem and had working experience in the intensive care unit, have reviewed the content of the scales from cultural and religious aspects. They agreed on an acceptable validity (CVI = 0.83%). To reassess the reliability of translated scale, the alpha coefficients of internal consistency (Pilot sample size: n = 20) was computed. The alpha coefficient for the instrument was 0.78. So translated scale showed a reasonable reliability and validity.
Data Collection and Analysis
The data collection of this study did not include sensible personal information which is defined as medical information, health status and information about transgression of the law. Further, the research was not an intervention study and there were no questions enabling revelations of any personal identity on the questionnaire. Thus, written informed consent was not obtained from participates. Accompanied by a letter including some information about the aim of the study, the questionnaires were handed out to participants by the third author. By retrieving patient’s medical history, persons who were older than 60 years and were suffered from chronic disease were detected. Patients designated the family member that most involved in decision making regarding their illness (often, but not necessarily the immediate carer). Those family members suggested by patients, were included in the study. Participation in the study was voluntary and anonymous. Data from the questionnaires were analyzed using Statistical Package for Social Scientists (SPSS16). A Kolmogorov-Smirnov test indicated that the data were sampled from a population with a normal distribution. Descriptive statistics were computed for the study variables. The comparison between all measured demographic factors was done using an independent T-test or One-Way ANOVA. The significance level considered in 0.05.
Results
Participants
Of the participants (132), 43.1%were male and 56.9% were female. Descriptive analyses of background information revealed that the majority of participants have less than 35 years old (52.8 %) and were married (67.2 %). Most of them had a diploma or higher level of education (72.3 %) and were clerk or self-employed (68.0 %). Most of them mentioned that pray every day (91.9 %), read Quran (the holy book of Islam) every day or sometime in a week (55.7 %) and always experience the existence of God (95.1%) in their daily living.
Descriptive findings
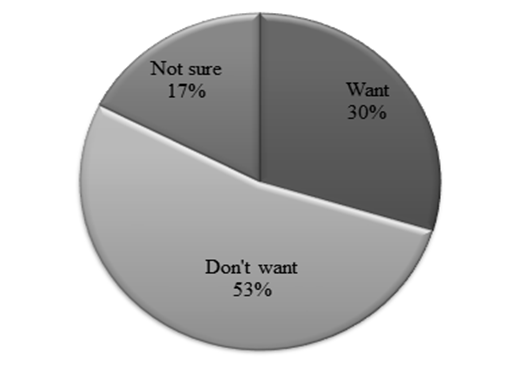
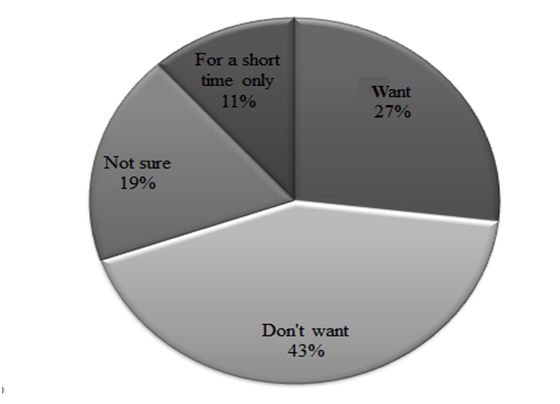
As indicated in table 1, participants had moderately positive attitude towards the use of LSTs (mean: 3.69 ± 0.54 out of 5). The lowest score belonged to the item “Life sustaining machines are often painful.” (Mean: 2.59 ± 1.01) and the highest one belonged to the item “Doctors should generally try to keep their patients alive on machines for as long as possible, no matter how uncomfortable the machines are.” (Mean: 4.55 ± 0.71). Among participants, 53% indicated that they do not have the personal desire for experiencing CPR in different hypothetical situations (Figure 1). Among them, 43% stated that they do not have the personal desire for use of mechanical ventilation in mentioned situations (Figure 2).
Table 1: Demographic factors affecting participants’ attitude towards life sustaining treatment.
| Characteristics | N (%) | Attitude (range 1-5) | Desire (range 0-8) | ||
|---|---|---|---|---|---|
| Mean (SD) | p-value | Mean (SD) | p-value | ||
| Gender | |||||
| Female | 70 (56.9) | 3.74 (0.58) | 0.26 | 3.16 (2.46) | 0.23 |
| Male | 53 (43.1) | 3.63 (0.48) | 2.61 (2.54) | ||
| Marital status | |||||
| Single | 40 (32.8) | 82 (67.2) | 0.29 | 2.23 (2.50) | 0.03* |
| Married | 82 (67.2) | 3.74 (0.59) | 3.28 (2.46) | ||
| Age | |||||
| < 25 | 40 (32.5) | 3.69 (0.43) | 0.18 | 2.76 (2.41) | 0.22 |
| 25-35 | 25 (20.3) | 3.56 (0.67) | 2.55 (2.69) | ||
| 36-45 | 31 (25.2) | 3.71 (0.46) | 2.96 (2.30) | ||
| 46-55 | 18 (14.6) | 3.66 (0.51) | 2.80 (2.59) | ||
| >55 | 9 (7.3) | 4.08 (0.76) | 4.78 (2.59) | ||
| Level of education | |||||
| Illiterate | 9 (7.6) | 4.30 (0.51) | 0.008 | 4.22 (2.39) | 0.47 |
| Primary | 6 (5.0) | 3.53 (0.43) | 2.97 (1.42) | ||
| Guidance or high school | 18 (15.1) | 3.65 (0.43) | 3.22 (2.36) | ||
| Diploma | 36 (30.3) | 3.82 (0.44) | 3.01 (2.50) | ||
| Graduated | 50 (42.0) | 3.57 (0.60) | 2.58 (2.74) | ||
| Occupation status | |||||
| clerk | 53 (44.5) | 3.66 (0.55) | 0.55 | 2.48 (2.62) | 0.18 |
| Self-employed | 28 (23.5) | 3.79 (0.53) | 3.51 (2.43) | ||
| Others | 38 (31.9) | 3.66 (0.56) | 3.13 (2.46) | ||
| Praying | |||||
| Daily | 113 (91.9) | 3.72 (0.54) | 0.09 | 2.99(2.53) | 0.76 |
| Some time in a week | 4 (3.3) | 3.57 (0.50) | 2.52(1.37) | ||
| Some time in a month | 1 (0.8) | 3.92 (0.0) | 3.20(0.0) | ||
| Some time in a year | 1 (0.8) | 3.00 (0.0) | 0.00 (0.0) | ||
| Never | 4 (3.3) | 2.94 (0.08) | 2.22(2.98) | ||
| Reading Quran | |||||
| Daily | 26 (21.3) | 3.83 (0.55) | 0.14 | 3.60 (2.67) | 0.63 |
| Some time in a week | 42 (34.4) | 3.71 (0.46) | 2.72 (2.45) | ||
| Some time in a month | 32 (26.2) | 3.70 (0.58) | 2.78 (2.29) | ||
| Some time in a year | 19 (14.8) | 3.56 (0.60) | 2.71 (2.78) | ||
| never | 4 (3.3) | 3.05 (0.23) | 2.35 (2.86) | ||
| Experience of God existence | |||||
| Always | 117 (95.1) | 3.71 (0.54) | 0.13 | 2.90 (2.48) | 0.60 |
| Sometime | 6 (4.9) | 3.37 (0.52) | 3.45 (3.07) | ||
| never | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
Figure 1: Participant’s personal desire for experiencing CPR.
Figure 2: Participant’s personal desire for use of mechanical ventilation.
The results revealed that there was a significant difference between participants’ attitude towards LSTs based on their level of education (p-value: 0.008). Illiterate persons showed the highest positive attitude towards LSTs (Mean: 4.30 ± 0.51) compared to others. There was a difference between participant’s personal desire for LSTs based on their marital status (p-value: 0.03). Married persons had more desire for LSTs compared to single persons. table 2
Table 2: Participant’s general attitude towards life sustaining treatments.
| Items | Mean(SD) |
|---|---|
| 1. If life-prolonging technology exists it should always be used. | 4.10 (0.89) |
| 2. Doctors should generally try to keep their patients alive on machines for as long as possible, no matter how uncomfortable the machines are. | 4.55 (0.71) |
| 3. If a patient is dying it is best not to prolong their lives by medical means. | 3.72 (1.03) |
| 4. Life sustaining machines should never be stopped even if the patient appears to be dying because there is always the chance of a miracle. | 3.78 (1.16) |
| 5. It is a doctor's duty to stop life prolonging treatments of patients if the patient does not want them anymore. | 3.58 (1.07) |
| 6. Even if I were terminally ill, I would want everything done to keep me alive as long as possible. | 3.95 (1.17) |
| 7. Life sustaining machines are often painful. | 2.59 (1.01) |
| 8. When a person is permanently unconscious (in a coma), with no hope of waking up, medical treatments usually should not be used to keep them alive. | 3.50 (1.21) |
| 9. Even if my condition is hopeless I would want my life prolonged as much as possible. | 3.40 (1.25) |
| 10. I would not want machines used to keep me alive | 3.42 (1.23) |
| 11. Present day medical care frequently prolongs dying without providing any real benefit to the patient. | 3.83 (0.93) |
| 12. If a patient is unable to breathe without a breathing machine it would be wrong to take them off the machine (even if the condition is hopeless) because that would bekilling the patient. | 3.81 (1.27) |
| 13. The use of life sustaining machines can be humiliating to the patient | 3.89 (0.98) |
Discussion
The results of this study indicated that participants had moderately positive attitude towards the use of life sustaining treatments (mean: 3.69 ± 0.54 out of 5). Among all items in the questionnaire the highest mean score (mean = 4.55) belonged to the item” doctors should generally try to keep their patients alive on machines for as long as possible, no matter how uncomfortable the machines are”. It is consistent with findings of previous study that examined South East Iranian nurse’s attitude towards different aspects of palliative care[28]. Examined nurses in this study were not positive towards withholding and withdrawing life sustaining treatments and they were likely to continue of life-prolonging cares for dying persons[28]. Consistently, Razban et al.,[23] examined critical care nurses attitude towards LST in South East Iran. They reported that nurse’s were likely to accept LSTs. This is contradicted by findings of some studies which evaluated people’s attitudes towards LSTs in some other countries. Participants in mentioned studies were on the general idea that life prolonging treatments should be forgone when there is no hope of recovery[10,18-21]. These results could be related to the participant’s religious beliefs.
All respondents were Muslim and shia. The majority of participants (95.1%) stated that they always experience the existence of God`s in their daily living. All of them claimed that they do religious activities with different regularity. Since this is one of the first assessments of Muslim/Iranian attitudes to LSTs it might be useful to know Islam’s views on LSTs. According to Islam, life and death are in the hand of God, and so individuals have no right to arrange their death or to kill themselves (this is referred to as the doctrine of the sanctity of life) and cannot be terminated by any form of active or passive human intervention[29]. Consistently, this study finding showed that persons, who pray, read the holy Quran and experience the existence of God more frequently, had more positive attitudes towards LSTs compared to individuals that perform these religious activities less frequently, although this finding was not statistically significant.
The results showed that participants’ attitude towards LSTs in the following study is more positive compared to that of participants in the other studies conducted in different countries could be related to fear of death. Iranmanesh et al.,[30] compared Iranian and Swedish nursing students’ attitude towards caring for dying people. They reported that Iranian nursing students tend to a have greater fear of death than Swedish nursing students (Iranmanesh et al., 2010). In a qualitative study that was conducted by Iranmanesh et al.,[31] they stated that Iranian oncology nurses face many barriers while caring for dying persons. One of these barriers they mentioned is that dying people do not accept that they are close to death and still expected something to be done for them. Nurses in that study narrated that many of dying patients experience a difficult death.
Another possible reason for respondents’ positive attitudes towards LSTs could be their low level of knowledge about LSTs. This assumption can be supported by the finding that, respondents with higher levels of education showed less positive attitude towards LSTs. It is consistent with the finding of previous study[22] that evaluated attitude of different ethnicities towards LSTs in America. Based on the results, among all of the items, the lowest mean score belonged to the item “Life sustaining machines are often painful.” (Mean: 2.59 ± 1.01). So, it seems that participants were not sufficiently aware of pain and suffering derived from LSTs.
The findings of the present study indicated that, married persons had more desire for life prolonging/sustaining technology compared to single persons. Kinship relationship is as sources of Iranian emotionalism and Iranians show a greater cohesion between parts of their family compared to western countries[32]. According to[33] in the Iranian context, the family not only fulfills psychological needs of their members, but practical ones and provide a permanent support network on which one can call in times of need[33]. It seems that married persons exhibit greater death anxiety because of their concern for the wellbeing of their children and spouse. Cole (1978) revealed that married women with children had higher level of death anxiety compared to others. Cole[34] stated that married women are “typically other-oriented in relation to death anxiety”. It seems that married women with children will exhibit greater death anxiety because of their concern for the wellbeing of their children and spouse.
It should also be mentioned, the convenience sample of participant and small sample size, which is not representative of all Family members of Muslim patients with chronic illness in South-East Iran, could limit the generalization of the findings.
Conclusion
The findings of this study showed that most participants believed that LSTs should be used, regardless of challenges behind that. Since life-sustaining treatment and its related issues such as advanced directive are not well established in Iran, more effort is needed to be planned as public education in this regard. A globally and suitable strategy about how to withdraw and withhold LST may never be accepted by the general public and may not be appropriately established since these issues individualized to each person through public education. The education may focus on the clarification of LST from different aspects such as medical and religious aspects. The education also should be included of LST’s advantages and disadvantages and about the situations that LST is preferable to use. Health care personnel are also required to formulate strategies to clarify the concept of LST for patients’ family members, specially those who are involved or may be involved with this issue. It is also required to elaborate policies and guidelines regarding use of LTs and forgoing of them form Muslim population. Since persons’ specific culture and religion could impact on their attitude and practice regarding LSTs, It is essential to explore the Iranian’s experience regarding LSTs through some qualitative studies and to develop a cultural based questionnaire. Also conduction of some transcultural studies in this field, could give the opportunity to benefit from the experience of the other cultures.
References
- 1. Straker, N. Facing Cancer and the Fear of Death: A Psychoanalytic Perspective on Treatment. (2012) Jason Aronson Incorporated.
- 2. Coleman, J.L., Buchanan, A. In harm's way: essays in honor of joel Feinberg. (2007) Cambridge University Press.
- 3. Negri, S. Self-determination, Dignity and End-of-life Care: Regulating Advance Directives in International and Comparative Perspective. (2012) Martinus Nijhoff Publishers.
- 4. Höllwarth, M.E. Pediatric Surgery. (2009) Springer.
- 5. Mauk, K. Gerontological Nursing: Competencies for Care. (2010) Jones & Bartlett Learning.
- 6. Jacobsen, B. Invitation to existential psychology: a psychology for the unique human being and its applications in therapy. (2008) Wiley com.
- 7. Adorno, G., Connor, S.R. (2009) Hospice and palliative care: The essential guide. (2012) Journal of Social Work in End-Of-Life & Palliative Care 8(2): 199-201.
- 8. Peirce, A.G., Smith, J.A. Ethical and Legal Issues for Doctoral Nursing Students: A Textbook for Students and Reference for Nurse Leaders. (2013) DEStech Publications.
- 9. Votroubek, W., Tabacco, A. Pediatric home care for nurses: A family-centered approach. (2010) Jones & Bartlett Learning.
- 10. Ko, E., Cho, S., Bonilla, M. Attitudes toward Life-Sustaining Treatment: The Role of Race/Ethnicity. (2012) Geriatr Nurs 33(5): 341-349.
- 11. Bernat, J.L. Ethical issues in neurology. (2008) Lippincott Williams & Wilkins Philadelphia.
- 12. Sole, M.L., Klein, D.G., Moseley, M.J. Introduction to critical care nursing. 6th ed: Elsevier Saunders (2010).
- 13. Islamic Republic of Iran statistics. (2013) World Health Organization.
- 14. Zahedi, F., Larijani, B., Tavakoly, B.J. End of life ethical Issues and Islamic views. (2007) Iran J Allergy Asthma Immun 6(s5): 5-15.
- 15. Rocker, G., Puntillo, K., Azoulay, E., et al. End of Life Care in the ICU: From advanced disease to bereavement. (2010) Oxford University Press.
- 16. Bloomer, M.J., Al-Mutair, A. Ensuring cultural sensitivity for Muslim patients in the Australian ICU: Considerations for care. (2013) Aust Crit Care 26(4): 193-196.
- 17. Peteet, J.R., D'Ambra, M.N. The soul of medicine: Spiritual perspectives and clinical practice. (2011) JHU Press.
- 18. Mok, E., Ting, F.H., Lau, K.p. Advance directives and life‐sustaining treatment: informed attitudes of Hong Kong Chinese elders with chronic disease. (2010) Journal of Nursing and Healthcare of Chronic Illness 2(4): 313-319.
- 19. Williams, N., Dunford, C., Knowles, A., et al. Public attitudes to life‐sustaining treatments and euthanasia in dementia. (2007) Int J Geriatr Psychiatry 22(12): 1229-1234.
- 20. Bayer, W., Mallinger, J.B., Krishnan, A., et al. Attitudes toward life-sustaining interventions among ambulatory black and white patients. (2006) Ethn Dis 16(4): 914-919.
- 21. Lee, J., Chen, P., Yeo, J., et al. Hong Kong Chinese teachers' attitudes towards life-sustaining treatment in the dying patients. (2003) Hong Kong Med J 9(3): 186-191.
- 22. Blackhall, L.J., Frank, G., Murphy, S.T., et al. Ethnicity and attitudes towards life sustaining technology. (1999) Soc Sci Med 48(12): 1779-1789.
- 23. Razban, F., Iranmanesh, S., Aliabadi, H.E., et al. Critical care nurses' attitude towards life-sustaining treatments in South East Iran. (2016) World J Emerg Med 7(1): 59-64.
- 24. Mogadasian, S., Abdollahzadeh, F., Rahmani, A., et al. The attitude of Iranian nurses about do not resuscitate orders. (2014) Indian J Palliat Care 20(1): 21-25.
- 25. Abdollahzadeh, F., Rahmani, A., Paknejad, F., et al. Do not resuscitate order: attitude of nursing students of Tabriz and Kurdistan Universities of Medical Sciences. (2013) Iranian Journal of Medical Ethics and History of Medicine 6(5): 45-56.
- 26. Ghajarzadeh, M., Habibi, R., Amini, N., et al. Perspectives of Iranian Medical Students About Do-Not-Resuscitate Orders. (2013) Maedica 8(3): 261-264.
- 27. RUMS. Introduction of Ali-ebn Abitaleb hospital.
- 28. Razban, F., Iranmanesh, S., Rafiei, H. Nurse's attitudes towards palliative care in south-east Iran. (2013) Int J Palliat Nurs 19(8): 403-410.
- 29. Campbell, A.V. Bioethics: The Basics. (2013) Routledge.
- 30. Iranmanesh, S., Axelsson, K., Häggström, T., et al. Caring for dying people: Attitudes among Iranian and Swedish nursing students. (2010) Indian Journal of Palliative Care 16(3): 147.
- 31. Iranmanesh, S., Axelsson, K., Sävenstedt, S., et al. A caring relationship with people who have cancer. (2009) J Adv Nurs 65(6): 1300-1308.
- 32. Bar, S. Iran: cultural values, self images and negotiation behavior. (2004) Institute for Policy and Strategy, The Lauder School of Government, Diplomacy and Strategy IDC.
- 33. Koutlaki, S. Among the Iranians: A guide to Iran's culture and customs. (2010) Intercultural Press.
- 34. Cole, M.A. Sex and marital status differences in death anxiety. (1979) OMEGA Journal of Death and Dying 9(2): 139-47.