Fetal Epidural Hemorrhage Following Non Primary CMV Infection: A Case Report
Francesco DAntonio, Barbara Matarrelli, Maurizio Pellegrini, Armando Tartaro, Alessandra Ricciardulli
Affiliation
1Department of Obstetrics and Gynaecology, University “G. d’Annunzio”, Chieti, Italy
2Department of Neuroscience and Imaging, University “G. d’Annunzio”, Chieti, Italy
Corresponding Author
Claudio Celentano, Department of Obstetrics and Gynaecology, University “G. d’Annunzio” Chieti-Pescara, Chieti 66100, Italy. Tel: +39-328-5577305; Fax: +39-0871-540034; E-mail: ccelen@tin.it
Citation
Celentano, C., et al. Fetal Epidural Hemorrhage following Non Primary Cmv Infection: a Case Report. (2015) J Gynecol Neonatal Biol 1(2): 50-51.
Copy rights
©2015 Celentano, C. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Prenatal CMV, Fetal MRI, Cerebral Hemorrhage, Prenatal Diagnosis, Fetal Ultrasound
Introduction
Case Report
Cytomegalovirus (CMV) is a common cause of intrauterine infection, and occurs in 0.2 - 2.2% of all live births in western countries[1]. Primary infection is defined as CMV infection in previously seronegative woman. After the primary infection the virus becomes dormant and exists in a latent state, from which it can be reactivated. In addition, there seem to be several strains of CMV that infect humans, so reinfection can occur. Therefore, secondary infection, may be due to reactivation or exposure to a new strain[2-4].
Congenital infection is the result of viral transplacental transmission. Preconceptional immunity is protective against vertical transmission, with a rate of intrauterine transmission following primary infection during pregnancy of 30 - 40%, compared with only 1% following secondary infection[1]. Within the infected fetuses 10 - 15% will demonstrate symptoms at birth, and 20 - 30% will die[2].
Most of the infected infants have no signs or symptoms at birth, but 5 to 15% will develop sequelae due to peculiar neurotrophic behavior of human CMV2. Screening for CMV infection is based on maternal serology, while virus isolation from amniotic fluid is the mainstay for prenatal diagnosis of fetal infection[5]. Ultrasonographic findings are helpful but not diagnostic, because the features are present in other intrauterine infections and diseases[5]. Commonly observed findings consist in ventriculomegaly, microcephaly, calcifications, periventricular echogenicity and pseudocysts, intracranial hemorrhage, cortical anomalies, intraventricular synechie, cerebellar abnormalities, hepatosplenomegaly and hyperechoic bowel[6]. Fetal MRI may improve the prognostic evaluation, especially when brain abnormalities are detected or suspected by ultrasound[7]. The detection of secondary infection or reactivation with human CMV in pregnant women is a real challenge to obstetricians[4]. The current case is a secondary CMV infection resulting in mid trimester fetus with a severe cerebral epidural hemorrhage.
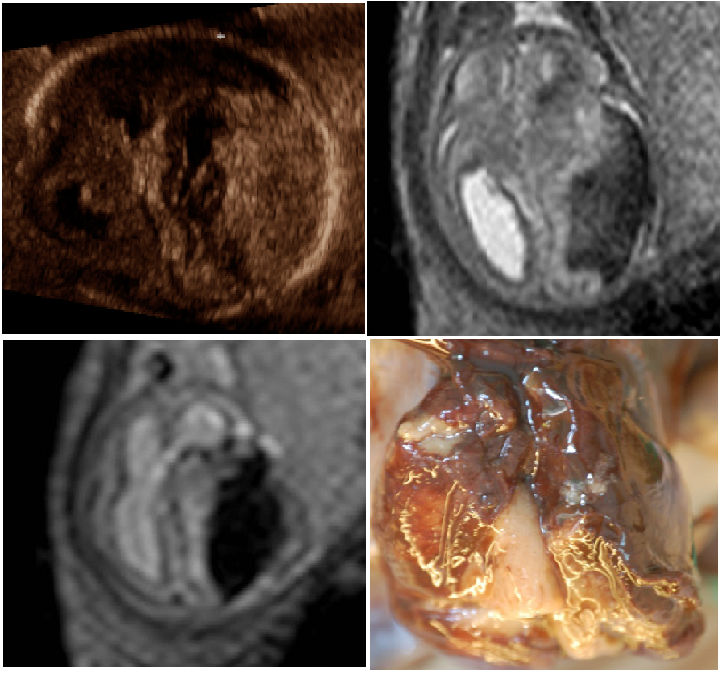
A 30 years-old woman gravida-1 at 20 weeks gestation was referred due to suspected hydrocephaly. A detailed scan revealed a hyper-echoic space-occupying lesion overlying the left temporo-parietal region (Figure 1A). The anterior horns of the ventricles appeared prominent, although the right lateral atria measurement in transverse section was within normal range with mild midline shift. Cavum septum pellucidi and third ventricle were unidentified. The fourth ventricle appeared dilated. Ultrasound scan revealed also a hyper-echoic bowel.
MRI was performed by using Philips Achieva 1,5T (Philips Medical Systems, Netherlands) and a phased-array Sense-XLTorso coil. Fetal brain was evaluated with a single-shot turbo spin echo sequence (TSE) in the coronal, sagittal and axial planes. Gradient echo (GE) T1-weighted, GE T1-weighted with selective water excitation (WATS) and GE T2*-weighted sequences were acquired and confirmed the diagnosis of epidural hemorrhage (Figure 1B-1C). Predisposing maternal conditions at risk for cerebral hemorrhage were examined. The patient blood was checked for Parvovirus B19, and CMV infections. Her previous serology charts at 8 and 14 weeks’ gestation respectively revealed an unremarkable result for CMV (positive anti-CMV-IgG and negative anti-CMV-IgM). 20th week of gestation blood serum sampling revealed elevated IgG and IgM, with elevated IgG avidity test (67%).
CMV DNA were detectable either on maternal blood and urine. In amniotic fluid sample 1,680,000 CMV DNA copies/ml were detected. Fetal CMV infection and affection of the fetus by severe cerebral epidural hemorrhage was diagnosed. After counseling, the couple opted for termination of the pregnancy. The post-mortem examination confirmed the presence of a epidural hemorrhage mainly in the parieto-occipital area, which was mainly organized. Multiple cytomegalic cells with nuclear inclusions surrounded by a clear halo were detected either on fetal tissues, or in placental samplings. (Figure 1D).
Figure 1: Prenatal Ultrasound Scan (A). Fetal Mri. S-Sh Tse T2-Weighted Images In The Axial(B), And T1-Weighted Sequence (C). Post-Mortem Evaluation (D).
To date, this is the first case of fetal epidural hemorrhage following ascertained not primary CMV infection. In this case previous serological screenings were unsuspicious, despite ongoing secondary infection. The detection of CMV specific DNA in plasma and urine samples, and particularly the very high CMV concentration in the amniotic fluid revealed the ongoing infection. Albeit maternal immunity to CMV, the presence of high avidity IgG antibodies does not exclude the possibility of vertical CMV infection[8]. Fetal hemorrhage may occur within ventricles, in subdural and epidural space. Possible etiologies include coagulations disorders, intracranial tumors, infections, hypoxia, maternal trauma, medications and drug abuse. Prognosis is poor, especially for high-grade lesions. Intracranial hemorrhage due to CMV has been reported. The pathophysiology of cerebrovascular damage is not completely ascertained yet and may be due to direct endothelial damage, thrombocytopenia or hypoxemia[9].
Conclusion
In conclusion this is the first case of fetal epidural hemorrhage following non primary CMV infection.
References
- 1. Stagno, S., Pass, R.F., Cloud, G., et al. Primary cytomegalovirus infection in pregnancy. Incidence, transmission to fetus, and clinical outcome. (1986) JAMA 256(14): 1904-1908.
- 2. Ornoy, A., Diav-Citrin, O. Fetal effects of primary and secondary cytomegalovirus infection in pregnancy. (2006) Reprod Toxicol 21(4): 399-409.
- 3. Boppana, S.B., Rivera, L.B., Fowler, K.B., et al. Intrauterine transmission of cytomegalovirus to infants of women with preconceptional immunity. (2001) N Engl J Med 344(18): 1366-1371.
- 4. Ross, S.A., Novak, Z., Pati, S., et al. Mixed infection and strain diversity in congenital cytomegalovirus infection. (2011) J Infect Dis 204(7): 1003-1007.
- 5. Malinger, G., Lev, D., Lerman-Sagie, T. Imaging of fetal cytomegalovirus infection. (2011) Fetal Diagn Ther 29(2): 117-126.
- 6. Malinger, G., Lev, D., Zahalka, N., et al. Fetal cytomegalovirus infection of the brain: the spectrum of sonographic findings. (2003) AJNR Am J Neuroradiol 24(1): 28-32.
- 7. Benoist, G., Salomon, L.J., Mohlo, M., et al. Cytomegalovirus-related fetal brain lesions: comparison between targeted ultrasound examination and magnetic resonance imaging. (2008) Ultrasound Obstet Gynecol 32(7): 900-905.
- 8. Adler, S.P., Nigro, G. Findings and conclusions from CMV hyperimmune globulin treatment trials. (2009) J Clin Virol 46 suppl 4: S54-57.
- 9. Ghi, T., Simonazzi, G., Perolo, A., et al. Outcome of antenatally diagnosed intracranial hemorrhage: case series and review of the literature. (2003) Ultrasound Obstet Gynecol 22(2): 121–130.