High Blood Pressures
Tim Nguyen* and Harold Doerr
Affiliation
The Human Simulation and Patient Safety Center, Department of Anesthesiology, Duke University, USA
Corresponding Author
Tim Nguyen, The Human Simulation and Patient Safety Center, Department of Anesthesiology, Duke University, USA, E-mail: Timothy.Nguyen@uth.tmc.edu
Citation
Tim N., et al. High Blood Pressures. (2014) J Anesth Surg 1(1): 1-9.
Copy rights
© 2014 Tim N. This is an open-access article distributed under the terms of the creative Commons Attribution 4.0 International License.
Introduction
Section 1: Demographics
Patient Name : Roy G Biv
Scenario Name : A day in the OR
Simulation Developer(s): Tim Nguyen and Harold Doerr
Date(s) of Development : 5/11/13 - 7/22/13
Appropriate for following learning groups (circle all that apply)
| Faculty | CME | ||||||
|---|---|---|---|---|---|---|---|
| Residents: (PGY) | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Specialties: | Anesthesiology | Nurse Anesthesia | Surgery | ||||
| Critical Care | Emergency Medicine | Obstetrics | |||||
| Medical Students (yr): | 1 2 3 4 | ||||||
| Nurse Anesthesia Faculty: CEU | |||||||
| Nursing Students (yr): | 1 2 | ||||||
| Other: | |||||||
Section 2: Curricular Information
Educational Rationale
To learn to treat and diagnose pheochromocytoma in the perioperative setting
Learning Objectives:
(ACGME Core Competencies: Medical knowledge (MK), Patient care (PC), Practice-based learning and improvement (PLI), Interpersonal and communication skills (CS), Professionalism (PR), Systems-based practice (SBP))
Objective 1: Medical Knowledge.
Objective 2: Patient Care.
Objective 3: Practice-base learning.
Objective 4: Interpersonal and communication skills.
Guided Study Questions
Question 1: How to diagnose pheochromocytoma?
Question 2: How to treat pheochromocytoma before surgery?
Question 3: How to treat a patient with pheochromocytoma during surgery?
Didactics
Pheochromocytoma[1-3]
1) Only important disease a/w adrenal medulla.
2) Most secrete both epi and norepi.
3) < 0.2% hypertensive patients.
4) Surgery curative in > 90%.
5) 90% are solitary tumors localized to single adrenal gland, usually on the right (non inherited).br> 6) 95% located in abdomen.
Inheritance
1) 5% inherited as familial autosomal dominant trait.
2) MEN type IIA: medullary carcinoma of thyroid, parathyroid hyperplasia, and pheo.
3) MEN type IIB: medullary carcinoma of thyroid, pheo, and neuromas of oral mucoas.
4) a/w von Recklinghausen neurofibromatosis or von Hippel-Lindau disease (retinal and cerebellar angiomatosis.)
5) Rarely extra-adrenal or malignant.
6) 75% bilateral: bilateral adrenalectomy should be considered (familial type.)
Clinical Presentation
1) Most common in young to mid-adult life.
2) Tumors not innervated, catecholamine release independent of neurogenic control.
3) Sustained HTN or paroxysmal leading to risk of CVA, heart failure, dysrhythmias, and MI.
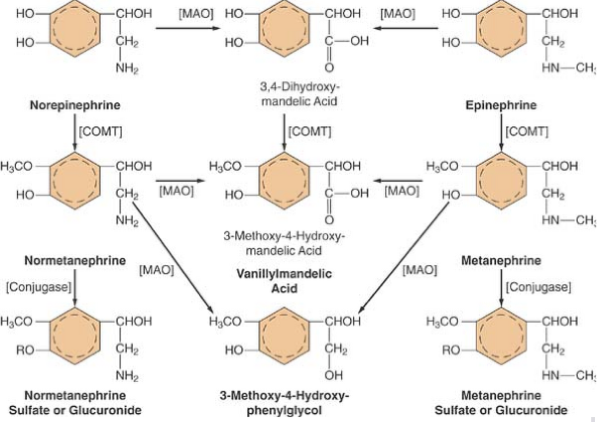
4) HA, palpitations, tremor, profuse sweating, pallor or flushing sometimes confused for malignant hyperthermia (Figure 1).
Figure 1: Catabolism of norepinephrine and epinephrine
Diagnosis
1) Free catecholamine concentration and metabolites in urine most common screening test (urinary vanillylmandelic acid and unconjugated NE and EPI levels measured in 24h urine collection).
2) Less specific: ECG (LVH and nonspecific Twave abn), CXR (cardiomegaly), CBC (elevated Hct/hemoconcentration).
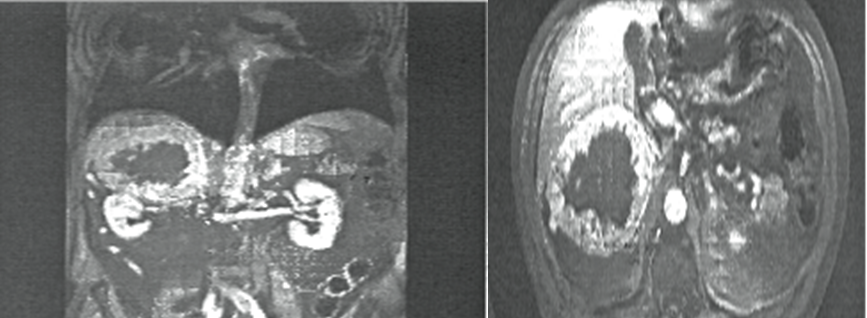
3) US/CT/MRI for noninvasive localization of tumors.
4) Metaiodobenzylguanidine scintigraphy effective in localizing recurrent/extra-adrenal masses (Figure 2.)
Figure 2: CT abdomen
Markers
1) Vanillylmandelic acid excretion: 81% sensitive, 97% specific.
2) Catecholamine excretion: 82% sensitive, 95% specific.
3) Metanephrine excretion: 83% sensitive, 95% specific.
4) Abdominal CT: 92% sensitive, 80% specific.
5) Paroxysmal HTN, HA, sweating, tachycardia: 90% sensitive, 95% specific.
6) Ultrasound has largely been replaced by CT as it is limited because of overlying bowel gas.
Preop Prepartion
1) perioperative mortality was 45%.
2) decreased to 0-3% following α antagonists for preop therapy.
3) α-adrenergic blockade is initiated once diagnosis of pheo is established.
4) Phenoxybenzamine, long-acting (24-48h) is noncompetitive presynaptic (α2 and postsynaptic α1 blocker dosed at 10mg q8h.
5) Doxazosin, terazosin, prazosin is a selective competitive α1 blocker, dosed initially as 1mg PO qHS because of postural hypotension.
Preop cont
1) Phenoxybenzamine or prazosin shown to be equally effective in controlling BP.
2) α blockade therapy recommended at least 10-14days prior to surgery until AM of surgery.
3) Allows for contracted intravascular volume/hematocrit to return to normal and stablize BP.
4) β adrenergic blockade occasionally added after α-blockade in patients with persistent tachycardia/dysrhythmias.
5) Not be given until adequate α blockade α-methyl tyrosine.
6) Inhibits enzyme tyrosine hydroxylase, rate-limiting step in catecholamine biosynthesis.
7) Reserved for those with metastatic disease or those which surgery is contraindicated and long-term medical therapy is required, i.e. patients with decompensated CHF, end stage COPD.
8) When used in combo with α-adrenergic blocking agents, there is significant reduction in catecholamine biosynthesis.
Pregnancy
1) Unrecognized pheochromocytoma during pregnancy may be life-threatening to mom and baby.
2) Adrenergic blockers probably improve fetal survival, but safety has not been established and no well-designed controlled studies have been done to prove this.
3) Perform surgery during first trimester or time of CS.
4) No reason to terminate early pregnancy, but should be aware of risk of spontaneous abortion from surgery.
Perioperative Management
1) If can’t start α-blocker prior to surgery or < 48h of treatment, can use nitroprusside.
2) If solitary tumor w/out mets, surgery involves laparoscopic retroperitoneal approach, and maybe later converted to open if needed.
3) During laparoscopy, pneumoperitoneum may cause release of catecholamines and hemodynamic changes can be controlled with vasodilator.
Periop cont
1) Manipulation of tumor may produce marked elevations in BP.
2) Acute hypertensive crises treated with IV nitroprusside or phentolamine.
3) Phentolamine is a short acting α adrenergic antagonist that’s given as 2-5mg IV bolus or continuous infusion as the half-life is 19 mins.
4) Tachydysrhythmia controlled with IV propranolol (1mg incrememts) or continuous infusion of ultrashort-acting selective β1 adrenergic antagonist esmolol.
Periop cont
1) Long-acting beta blockers disadvantages: persistence of bradycardia/hypotension after tumor removed.
2) Magnesium sulfate infusion with intermittent boluses has been successful to control BP after maximizing α adrenergic antagonists.
3) Nicardipine, nitroglycerin, diltiazem, fenoldopam, and prostaglandin E1 have all been used anecdotally.
Periop cont- hypotension
a) Reduction of BP after ligation of tumor's venous supply can be dangerously abrupt, and close communication required.
b) Initial therapy: Restore intravascular fluid deficit.
c) If remains hypotensive: phenylephrine.
d) After surgery: catecholamines return to normal over several days.
e) 75% patients are normotensive within 10 days.
Assessment Instruments
a) Mac3 or Miller
b) Endotracheal tube
c) Arterial line set up
Section 3: Preparation
Monitors Required
| 1 | Non-Invasive BP Cuff | ||||
|---|---|---|---|---|---|
| 1 | Arterial Line | ||||
| CVP | |||||
| PA Catheter | |||||
| 1 | 5 Lead EKG | ||||
| 1 | Temperature Probe | ||||
| 1 | Pulse Oximeter | ||||
| 1 | Capnograph | ||||
| 1 | BIS |
Other equipment required
| 1 | Anesthesia Machine | 1 | EIT | ||
|---|---|---|---|---|---|
| 1 | Pumps | LMA | |||
| Brochoscope | 1 | Laryngoscope | |||
| Defibrillator | |||||
| Hotline | |||||
| Nerve Stimulator | |||||
| Echo Machine and Probe |
Supporting Files (cxr, ekg echo, assessment, handouts, etc)
1. Chest xray–no pulmonary infiltrates pleural effusions, or pneumothorax.
2. Electrocardiogram–sinus tachycardia and inverted T wave on leads V5 and V6.
3. Trans-Thoracic Echocardiogram –Ejection Fraction of 55% with no regional wall motion abnormalities Abdominal Computerized Tomography: possible acute appendicitis.
Time Duration
| Set-up | 20 Min |
|---|---|
| Preparation | 4 Hours |
| Simulation | 20 Mins |
| Debrief | 20 Mins |
| Programming/Scripting | 8 Hours |
Case Stem
Case Stem (one to two paragraphs on pertinent patient and scenario information-this should be the stem for the learner and should include location, physician/help availability, family present, etc.)
60 year old male with no past medical or surgical history presented to the Emergency Room with sudden onset dyspnea and palpitations[1,2]. For the past 2 weeks, he had been experiencing include intermittent headaches, palpitations, anxiety, and occasional shortness of breath on exertion, which is what brought him to the hospital. This morning, his wife noted increased anxiety leading to "he can’t catch his breath." Work up includes an Electrocardiogram, cardiac enzymes, chest x-ray, stress test, and transthoracic echocardiography, all of which were normal. Incidentally, a abdominal Computerized tomography (CT) scan was performed, and an acute appendicitis could not be ruled out, so he was sent to the Operating Room to do a diagnostic laparoscopy and appendectomy.
Background and briefing information for Facilitator/coordinator's eyes only
In the ER, his blood pressure ranged from noninvasive systolic 140-280 millimeters mercury over diastolic 30-150 millimeters mercury, so a CT (computerized tomography) abdomen showed a 6-centimeter round mass retroperitoneally on the right adrenal gland suggesting pheochromocytoma[4,5], but this was missed initially as it only showed a possible acute appendicitis. Serum epinephrine was 18.6 nanogram/milliliter (normal: 0.01-0.18 nanogram/milliliter), norepinephrine 24.2 nanogram/milliliter (normal: 0.06-0.45 nanogram/milliliter), and dopamine 4.8 nanogram/milliliter (normal 0-0.09 nanogram/milliliter). No metaiodobenzylguanidine (MIGB) scan performed because of acute renal failure.
Patient Data Background and Baseline State
Patient History (should follow standard H and P format)
Review of Systems:
a) Central Nervous System: + headache, no strokes or seizures or focal deficits.
b) Cardiovascular: + palpitations and chest pain, no murmurs/arrhythmias.
c) Pulmonary: + dyspnea with exertion and now at rest, no wheezing or asthma or cough.
d) Renal / Hepatic: + decreased urine output, acutely, no cirrhosis or liver problems.
e) Endocrine: no diabetes or excessive thirst[2].
f) Hematology/Coagulation: no easy bruising or bleeding.
Current Medications and Allergies: No current meds, No known drug allergies
Physical Examination: General: No acute distress, well developed, well nourished Weight, Height: 77kg, 170 centimeters, Vital Signs: noninvasive blood pressure 180/100 mmHg (millimeters of mercury) Heart Rate 101 beats per minute Temperature 99.9 Fahrenheit, Respiratory rate 20 breaths per minute Oxygen saturation: 95% on Room Air, Airway: Mallampati I, normal mouth opening, full range of motion of the neck, Lungs: bilateral equal breath sounds, no wheezes, rales, rhonchi, Heart: sinus tachycardic, no murmurs, gallops, rubs.
Laboratory, Radiology, and other relevant studies: Hematocrit: 45%, Chest XRay: no pulmonary infiltrates, pleural effusions, or pneumothorax, Electrocardiogram: sinus tachycardia and inverted T wave on leads V5 and V6.
Baseline Simulator State: What underlying alterations in physiology would this patient have when compared to "perfect" 70 kg man or woman? Include target numbers. This will comprise your baseline state
a) Vitals: Blood Pressure 180/100 mmHg (millimeters Mercury) Heart Rate 141 beats per minute Temperature 99.9 Farenheit Respiratory Rate 20 breaths per minute Oxygen saturation:97% on Room air.
b) Neurologic: alert and oriented to person, place, time, and no focal deficits.
c) Respiratory: bilateral equal breath sounds.
d) Cardiovascular: sinus tachycardia.
e) Gastrointestinal: positive bowel sounds, diffusely mildly tender to palpation.
f) Genitourinary: decreased urine output.
g) Metabolic: normal.
h) Environmental: normal OR setting.
| State | Patient Status | Student learning outcomes or actions desired and trigger to move to next state | |
|---|---|---|---|
| 1. BASELINE | Awake, alert and oriented to person, place, time, responsive, noninvasive BP (Blood Pressure) 120s-180s/60-90s mmHg. HR (heart rate) 70-150s BPM (beats per minute) | Learner Actions: a) IV (intravenous) phentolamine (i.e. 5 milligrams IV x 1). b) Preop PO alpha antagonist i.e. phenoxybenzamine (i.e. 10milligrams by mouth once daily) or doxazosin (i.e. 1 milligram by mouth once daily), terazosin (i.e. 1milligram by mouth once daily), prazosin (i.e. 1milligram by mouth once daily). |
Operator: a) Decrease systolic BP by 10-20 points if alpha antagonist started. b) Proceed to MILD if started on alpha antagonists. c) Proceed to Moderate if not. d) Teaching Points. e) Starting alpha 1 blockade before beta blockers. f) Control HTN. Trigger: alpha blockers- proceed with MILD, if given beta blockers without alpha blockers, proceed to SEVERE, if student fails to start alpha blockers at all, proceed to SEVERE and after 10mins DEATH. |
| 2. MILD | Awake, alert and oriented to person, place, time, responsive before induction. Invasive BP 120s-180s/60-90s mmHg. HR 70-150s BPM, then converted over to general anesthesia with same vitals. | Learner Actions: a) General anesthesia, regular induction. b) Avoid Desflurane. c) Propofol 50 microgram/kilogram/hour + Sufenta 0.2 microgram/kilogram/hour with ½ MAC of Sevoflurane or Isoflurane. d) Continue IV phentolamine 5milligram IV every 5 mins |
Operator: a) Proceed to general anesthesia state. b) Teaching Points. c) Careful attention to vital signs. d) Avoid Desflurane because of tachycardia and non-neurogenic catecholamine release. e) Extremely important to achieve adequate depth of anesthesia before proceeding with Direct laryngoscopy to minimize sympathetic nervous system response. Trigger: 5 minutes, proceed to MODERATE, unless student used desflurane, proceed to SEVERE; if student did not adequately anesthetize patient before direct laryngoscopy, proceed to SEVERE for 2 minutes and return to moderate. |
| 3. Moderate | Unresponsive, under general anesthesia, very labile blood pressures (BP 70-200s/40-110smmHg). (beginning to middle of the surgery). | Learner Actions: a) Continuous infusion of IV phentolamine 5 milligrams IV every 5 minutes. b) IV magnesium 2grams IV over 30 minutes. c) IV beta blocker i.e. esmolol infusion 50 micrograms/kilogram/minute or propranolol 1 milligram IV x once. d) IV nitroprusside 0.3-4 microgram/kilogram/minute e) IV nicardipine 3-5 milligram/hour. |
Operator: a) Labile blood pressures, but not as bad as SEVERE. Teaching Points: a) Blood pressure will rapidly decrease after resection of the tumor Trigger: 5 minutes, or if student does not use anything besides alpha antagonist, proceed with SEVERE, if student uses IV beta blockers, nitroprusside, or any other antihypertensive agent, proceed with MILD again and then RESOLUTION afterwards in 5 minutes |
| 4. SEVERE | Unresponsive, under general anesthesia, very labile blood pressures (BP 150-200s/40-110s mmHg). Heart Rate is 120-180s BPM (surgeon is manipulating the tumor or no alpha antagonist started) | Learner Actions: a) Continuous infusion of IV phentolamine, may need to increase dose. b) Need to add beta blockade like propranolol 1 milligram IV x once or esmolol 50 micrograms/kilogram/minute or metoprolol IV 1-2 milligram x once |
Operator: a) Tell student that surgeon also sees an adrenal mass that he would like to take out as well. b) Tell the examinees that the surgeon has just resected the tumor before proceeding with the RESOLUTION state. c) Very labile blood pressures as surgeon is manipulating tumor releasing a lot of catecholamines. Teaching Points: a) Blood pressure will rapidly decrease after resection of the tumor. Trigger: after starting beta blocker proceed to MILD for 2 minutes before proceeding to RESOLUTION or 5 minutes proceed to RESOLUTION if student fails to add anything in addition to alpha blockers; DEATH if student did not add any antihypertensives at all since the beginning, especially alpha antagonists. |
| 5. RESOLUTION | Blood pressure low: 60s/40s mmHg as surgeon just resected tumor. HR 50s (beats per minute) if learner used long acting beta blocker or still on Esmolol drip. | Learner Actions: a) Start a pressor i.e. norepinephrine to maintain blood pressure, and preferably a drip i.e. Norepinephrine 0.2 micrograms/kilogram/minute b) IV (Intravascular) fluids: 1-2Liters Lactated Ringers or Normal Saline. |
Operator: a) Increased the Blood Pressure (BP) to normal values 120s/80s mmHg if the examinees titrate in a pressor. Teaching Points: a) Ligation of tumor’s venous supply can be cause reduction in BP abruptly. b) May need to start a pressor after tumor is resected. c) Long acting beta blocker i.e. propranolol may lead to persistence of bradycardia/hypotension after tumor removal. d) Need to restore intravascular fluid deficit Trigger: student starts a pressor like Norepi or phenylephrine, return to normal vital signs 120s/80s mmHg Heart Rate 80s beats per minute. If student fails to start a pressor, IV fluids, go to hypotension 60s/40smmHg and DEATH in 5 mins. |
References
- 1. Roizen, M.F. Anesthetic Implications of Comorbid Diseases. (2010) Miller's Anesthesia. Philadelphia: Churchill Livingstone/Elsevier.
- 2. Barash., Paul, G. Endocrine Function. (2009) Clinical Anesthesia. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
- 3. Uchida, N., Ishiguro, K., Suda, T., et al. Pheochromocytoma Multisystem Crisis Successfullly Treated by Emergency Surgery: Report of a Case. (2010) Surg Today 40(10): 990-996.
- 4. Domi, R., Laho, H. Management of Pheochromocytoma: Old Ideas and New Drugs. (2012) Niger J Clin Pract 15(3): 253-257.
- 5. Myklejord, D.J. Undiagnosed Pheochromocytoma. (2004) Clin Med Res 2(1): 59-62.