Iatrogenic Life Threatening Tracheal Tear in Pediatric Patient; A Challenging Case to Manage
Dekel Lait1, Eli Hershmann2, Dan Levy-Faber3, Anat Ilivitzki4 and Michal Barak1*
Affiliation
- 1Department of Anesthesiology, Rambam Health Care Campus and the Bruce Rappaport Faculty of Medicine, Technion
- 2Pediatric Intensive Care Unit, Rambam Health Care Campus and the Bruce Rappaport Faculty of Medicine, Technion
- 3Department of Thoracic Surgery, Carmel Medical Center, Haifa, Israel
- 4Pediatric Radiology Unit, Rambam Health Care Campus and the Bruce Rappaport Faculty of Medicine, Technion
Corresponding Author
Barak, M., Department of Anesthesiology, Rambam Health Care Campus, POB 9602, Haifa 31096, Israel; Tel: 972 4 854-2487/ E-mail: m_barak@rambam.health.gov.il
Citation
Barak, M., et al. Iatrogenic Life Threatening Tracheal Tear in Pediatric Patient; A Challenging Case to Manage. (2015) J Anesth Surg 2(1): 34-36.
Copy rights
© 2015 Barak, M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Tracheal tear; Endotracheal intubation; Complications
Abstract
We present a case in which an 11 month old baby with Johanson–Blizzard Syndrome developed respiratory failure due to respiratory syncytial virus. The baby was intubated and re-intubated several times using different endotracheal tube sizes in an effort to improve ventilation. While in the pediatric intensive care unit, her condition deteriorated and a tear at the posterior wall of the trachea adjacent to the carina was diagnosed. An attempt to correct surgically the tear failed and the child recovered within several days without additional surgical intervention. We discuss the management of a tracheal tear in the pediatric population, particularly the conservative as opposed to the surgical approach.
Introduction
Tracheal injury in the pediatric population is usually the result of blunt trauma involving injury to the head and neck regions[1,2]. Iatrogenic tracheal tear following intubation is rare yet happen[3-5]. In most of the cases documented in the literature, tracheal injury following intubation is usually at the posterior membranous wall, which is a weaker structure than the anterior wall with its tracheal cartilages. The risk of such an injury increases during emergent intubation, when performed by less experienced personnel, and in young babies and neonates[4-6]. The injury is often masked by other respiratory problems, and late diagnosis may further complicate management. Diagnosis is not straightforward, as the injury is usually accompanied by subcutaneous emphysema, pneumothorax or pneumomediastinum secondary to air leakage from the tear. The incidence of iatrogenic injury following intubation is unknown. However, it is a life-threatening condition when it happens[6].
The preferred management in such cases is still a matter of debate, especially in the pediatric population. Several case reports describe successful conservative management, leaving surgical repair as a last resort for patients with larger tracheal defects which are stable enough for operative repair[3,4]. The surgical management of a distal tracheal tear is difficult and challenging and may require a lung isolation technique and occasionally the use of a cardio-pulmonary bypass (CPB) machine. Conservative treatment combined with the utilization of extracorporeal membrane oxygenation (ECMO) may be the ideal method to manage the situation[7]. However, that technology is not always at hand, as was the situation in our case.
Case Report
A 11 month old baby girl with Johanson–Blizzard syndrome was brought to the local clinic by her parents because of thick nasal secretions accompanied by cough and mild fever of 38ºC that started two days earlier. Johanson–Blizzard syndrome is characterized by abnormal nasal and craniofacial development, as well as mental retardation and deafness. At the clinic the baby was found to be bluish and bradypneic (8 breath/min). Her oxygen saturation measured 58% on room air, with a heart rate of 58 beats/min. The clinic physician tried to intubate her but failed, and an emergency medical ambulance was called to transfer her to hospital. While waiting, she was ventilated with a mask and reservoir bag. The emergency team that arrived intubated the baby with an un cuffed endotracheal tube (ETT) size 3.0, ventilated and transported her to our hospital emergency room (ER).
On admission to the ER, oxygen saturation measured 98%, heart rate was 140 beats/min and blood pressure was72/42. The baby's weight was 5.7kg. At that time, the ETT was exchanged to an uncuffed tube size 3.5 since airway pressures were high and ventilated volumes were low due to an air leak. It was decided to admit the baby to the pediatric intensive care unit (PICU) for ventilation and observation. In the PICU the baby was re-intubated yet again, using a cuffed ETT size 4.0. However, shortly afterwards subcutaneous emphysema appeared in the lower neck and upper thoracic regions. Chest auscultation revealed reduced breathing sounds bilaterally and chest radiography demonstrated a large pneumothorax in the left hemi-thorax with mediastinal shift to the right (Figure 1). A chest tube was inserted to the left side. The baby was hemodynamically stable with frequent desaturations that required manual ventilation using bag valve mask resuscitator.
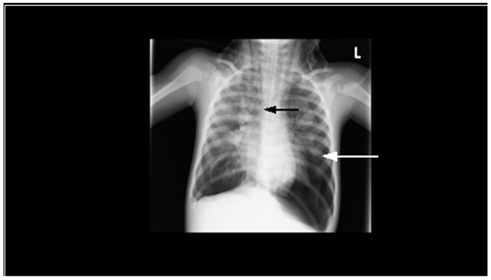
Figure 1: a Chest radiography of the ventilated child in PICU. Note the pneumothorax on the left side (white arrow) and the tip of the endobronchial tube (black arrow). Subcutaneous emphysema is seen around the neck.
During the following days, the baby's condition continued to deteriorate. Sputum examination was positive for respiratory syncytial virus (RSV). She was ventilated using pressure regulated volume control mode, starting with 32/19/5 cm H20 peak/plateau/peep pressure, and increasing gradually. Chest radiography demonstrated bilateral infiltration in all lung fields and bilateral pneumothorax. A chest drain was inserted to the right side, and no leak was initially observed in the drains. Ventilation parameters were modified to cope with the respiratory condition. Arterial blood gases (ABG) were: PH 7.48, PaO2 214 mm Hg, PCO2 38 mm Hg, bicarbonate 28 mEq/L. The respiratory condition was attributed to RSV and bilateral pneumothorax.
On the fourth day, after showing no improvement in respiratory parameters and with increasing subcutaneous emphysema the baby was ventilated using high frequency oscillation to decrease airway pressure and lung injury. To better understand the patient's condition, a chest CT study was performed, which revealed a tracheal tear proximal to the carina at the posterior wall of T3 level, through which the ETT partially penetrated into the mediastinum (Figure 2a & 2b). At that time the patient's condition deteriorated rapidly, oxygen saturation decreased to 70-80%, and an air leak appeared in both chest tubes. It was decided to convert to single lung ventilation mode, to let the tracheal tear heal spontaneously. The ETT was exchanged for a size 4.5 and fiber-optic bronchoscopy was performed. With the bronchoscope in place, the tube was withdrawn back to the trachea from the mediastinum and positioned distal to the tear in the right main bronchus after an unsuccessful attempt to position it on the left side. Afterwards, oxygenation improved rapidly and remained stable. The baby was ventilated using high frequency ventilation at a frequency of 7.5 HZ and a mean pressure of 10- 12 mm Hg. On repeated physical examination the subcutaneous emphysema slowly disappeared.
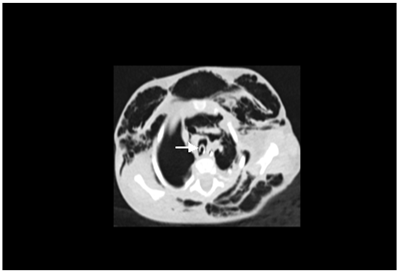
Figure 2a: Chest CT of the patient on her 4th day in PICU. The tip of the endobronchial tube is in the mediastinum, on (a) sagital view, (white arrow).
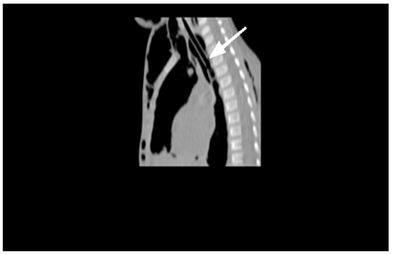
Figure 2b: Chest CT of the patient on her 4th day in PICU. The tip of the endobronchial tube is in the mediastinum, on (b) lateral view (white arrow).
During the next several days, the child's respiratory condition remained grave with frequent de-saturations even upon the mildest movement of the ETT. The possibility of operating and repairing the tracheal tear was discussed with the thoracic surgeons who were reluctant to perform the operation due to the child's severe condition. Eventually it was decided to operate without CPB, using right thoracotomy approach. This plan relied on the fact that during the operation the patient was to be ventilated selectively to her left lung.
The baby was taken to the operating room on the ninth day following her admission to the PICU. The ETT was placed in the left main bronchus by the pediatric pulmonologists. Upon chest opening, ventilation became ineffective, probably due to ETT retraction that occurred during that time, which led to extensive air leakage through the tear. Hypoxemia ensued, followed by severe bradycardia and cardiac arrest. The baby was turned to supine position and resuscitation was initiated immediately, including chest compressions, pharmacological support and ETT repositioning with return of spontaneous pulse after approximately 15min. ABG demonstrated ph = 6.91, PCO2 = 112, PO2 = 22. After securing the patient's condition, the surgeons succeeded to rapidly close the posterior tear with several stitches and bio-glue reinforcement.
Through the following days the baby was in a critical condition. Nitric oxide was used and ventilation modes were changed several times. The option for re-operation, with CPB was raised, since it was unknown if the baby would survive without surgery. Gradually, after 14 days of being unstable, the deterioration ceased and her condition improved gradually. Nitric oxide was stopped and the chest drains were removed. Soon afterwards spontaneous breathing resumed and she was extubated without complications. The infant was discharged from the hospital two months after her admission.
Discussion
Tracheal tear after intubation is a life-threatening condition and mortality rates in pediatric patients are reported to be as high as 75%[3,4]. This situation may be managed conservatively or surgically. The goal of conservative treatment is to preserve good oxygenation and ventilation while allowing the tear to heal spontaneously. However, this is not easy, since positive-pressure ventilation through the endotracheal tube often keeps further tearing the tissue, interfering with its healing. At the same time, mediastinal and pleural air leaks prevent effective ventilation.
Surgical treatment, on the other hand, has its difficulties: the trachea is delicate, fragile and short at that age, the tracheal posterior wall is thin and difficult to suture, and there is no adjacent soft tissue that can be used for closing the tear. The surgery is usually performed with the patient on the lateral position, thus, resuscitation, when required, is not feasible, and the patient is to be re-position to the supine position with the chest yet open. Another surgical option is performing the operation while using the CPB machine. For that, full heparinization is required, as well as cannulating the large blood vessels to connect them to the machine's tubes. All this has to be performed in an already borderline cardio-pulmonary state infant.
From the anesthesiologist point of view, ventilation during the surgery is challenging. In the pediatric patient with tracheal tear, minimal ventilation is feasible during the time that the chest is closed since the leak, to some extent, is contained within the mediastinum. As soon as the chest is opened, the leakage of air becomes significant and positive pressure ventilation is no longer possible, as in our patient. The effort to ventilate only one lung is complex, both from practical and physiological reasons. Placing the ETT in the left main bronchus is especially difficult in an infant, due to the angle between the left main bronchus and the trachea. If succeeded, one lung ventilation thereby creates a very large shunt, which may be incompatible with life in a respiratory compromised patient.
Several different criteria have been suggested regarding conservative or surgical management in the adult patient. Conservative management may be a suitable option for patients with uncomplicated ventilation, with small, proximal, superficial or sufficiently covered tears, and moderate and nonprogressive emphysema. Immediate surgical repair remains warranted in those patients whose tear is large and in those who require mechanical ventilation that cannot be delivered past the distal laceration[8,9]. In the subgroup of pediatric patients subjected to this kind of injury, the operation is more difficult, and the majority were treated conservatively[3,4,10]. The ECMO technology offers significant support for the conservative option. It allows oxygenation and removal of carbon dioxide without positive pressure ventilation, hence buying time for tracheal scar healing and recovery. The disadvantages of ECMO use are the need for large vessels cannulation and heparinization[7,11,12]. Unfortunately, the ECMO technology is expensive, requiring experienced personnel and special equipment, and it is not available in all hospitals. In such cases, transfering the child to the closest medical center with an ECMO facility should be considered before any surgical intervention, taking into consideration the risks involved.
Our case report demonstrates a few of the problems that are characteristic for an iatrogenic tracheal tear and its management in an infant. The baby was sick and weak to begin with. She was repeatedly intubated by several caregivers, as sometimes happens in an infant with respiratory disease, in an effort to improve ventilation. Afterward, the diagnosis was delayed since the patient's symptoms were attributed to the underling respiratory disease. Subsequently, conservative treatment was tried for some time, with minimal or no success. Finally, when the baby was in the worst condition, an operation was conducted, as a last resort. The operation caused further deterioration in the baby's condition, towards the need of resuscitation. During all that time, the baby's life was hanging in the balance.
In conclusion, a tracheal tear in a pediatric patient is a complex, life-threatening condition that is very difficult to manage. The decision whether to manage it conservatively or surgically should be taken in each patient individually, according to the specific clinical circumstances, being prepared to change strategy in the event of deterioration in the patient's condition.
Conflict of Interest Statement: No Conflict of Interest
References
- 1. Eipe, N., Choudhrie, A. Tracheal rupture in a child with blunt chest injury. (2007) PaediatrAnaesth 17(3): 273-277.
- 2. Claes, I., Van Schil, P., Corthouts, B., et al. Posterior tracheal wall laceration after blunt neck trauma in children: a case report and review of the literature. (2004) Resuscitation 63(1): 97-102.
- 3. Cunningham, L.C., Jatana, K.R., Grischkan, J.M. Conservative management of iatrogenic membranous tracheal wall injury: A discussion of 2 successful pediatric cases. (2013) JAMA OtolaryngolHead Neck Surg 139(4): 405-410.
- 4. Doherty, K.M., Tabaee, A., Castillo, M., et al. Neonatal tracheal rupture complicating endotracheal intubation: a case report and indications for conservative management. (2005) Int J PediatrOtorhinolaryngol 69(1): 111-116.
- 5. Wei, J.L., Bond, J. Management and prevention of endotracheal intubation injury in neonates. (2011) CurrOpinOtolaryngol Head Neck Surg 19(6): 474-477.
- 6. Mahieu, H.F., de Bree, R., Ekkelkamp, S., et al. Tracheal and laryngeal rupture in neonates: complication of delivery or of intubation? (2004) Ann OtolRhinolLaryngol 113(10): 786-792.
- 7. Simpao, A.F., Javia, L.R., Schwartz, A.J., et al. Shoulder dystocia, laryngeal tear, mediastinal intubation, and extracorporeal membrane oxygenation in a neonate. (2014) Anesthesiology 120(2): 480.
- 8. Schneider, T., Storz, K., Dienemann, H., et al. Management of iatrogenic tracheobronchial injuries: a retrospective analysis of 29 cases. (2007) Ann ThoracSurg 83(6): 1960-1964.
- 9. Deja, M., Menk, M., Heidenhain, C., et al. Strategies for diagnosis and treatment of iatrogenic tracheal ruptures. (2011) Minerva Anestesiol 77(12): 1155-1166.
- 10. Van Dorn, C.S., Sittig, S.E., Koch, C.A., et al. Selective fiberoptic left main-stem intubation to treat bronchial laceration in an extremely low birth weight neonate. (2010) Int J PediatrOtorhinolaryngol 74(6): 707-710.
- 11. Maslach-Hubbard, A., Bratton, S.L. Extracorporeal membrane oxygenation for pediatric respiratory failure: History, development and current status. (2013) World J Crit Care Med 2(4): 29-39.
- 12. Rehder, K.J., Turner, D.A., Cheifetz, I.M. Extracorporeal membrane oxygenation for neonatal and pediatric respiratory failure: an evidence-based review of the past decade 2002-2012. (2013) PediatrCrit Care Med 14(9): 851-861.












