Influence of different diagnostic procedures on radiation dose during peripheral interventions.
Magnus Baumhakel*, Michael Kindermann
Affiliation
Caritas Klinikum St. Theresia Saarbrücken, Department of Internal Medicine, Saarbrücken, Germany
Corresponding Author
Magnus Baumhakel, Caritas Klinikum St. Theresia Saarbrücken, Department of Internal Medicine, D-66131 Saarbrücken, Germany, Tel: 0049-681-406-4243, Fax: 0049-681-406-1753; E-mail: magnus@baumhaekel.de>
Citation
Baumhäkel, M., et al. Influence of Different Diagnostic Procedures on Radiation Dose During Peripheral Interventions. (2017) Bioinfo Proteom Img Anal 3(2): 210- 213.
Copy rights
© 2017 Baumhakel, M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Radiation, Peripheral Intervention, Diagnostic Procedure
Abstract
Aim: Interventional radiology procedures using ionizing radiation were frequent and become more and more complex. While determinants of radiation exposure during coronary angioplasty have been examined intensively during the last decade, available data regarding peripheral interventional procedures and especially the influence of pre-interventional diagnostic procedures on radiation exposure are limited.
Materials and Methods: Procedural data of 289 consecutive patients who underwent peripheral were included in this study. Radiation exposure was analysed using the dose area product (DAP, Gy*cm²) and total time of fluoroscopy dependent on region of intervention and type of diagnostic procedure prior to intervention.
Results: Information about vascular status of patients before the intervention led to a significant decrease of the dose area product irrespective of the region of intervention (iliac, femoro-popliteal, crural, multi-vessel, p < 0.05). Reduction of radiation exposure was highest with prior angiography or a CT- or MR-angiography (p < 0.01), whereas a diagnostic vascular ultrasound tended to decrease radiation exposure of patients (n.s.). Fluoroscopy time was not affected by the kind of diagnostic procedure (n.s.).
Conclusions: Patients´ radiation dose during peripheral interventional procedures is strongly dependent on vascular region, precise information about vascular status and previous vascular imaging. Thus, physicians should emphasize accurate vascular diagnostic procedures prior to peripheral intervention.
Introduction
Interventional radiology procedures using ionising radiation such as percutaneous coronary angioplasty and peripheral interventional procedures are frequent and become more and more complex. Thus, radiation exposure of patients increased, particularly in the context of repeated treatment for multi-vessel-diseases or re-stenosis[1]. As a result, deterministic radiation effects are possible and likelihood of stochastic effects may increase[2].
Determinants of radiation exposure of patients and physicians during coronary angioplasty have been examined intensively during the last decade[3-7]. However, available data regarding peripheral interventional procedures are limited. Highest radiation doses were reported during endovascular aneurysm repair and iliac artery stenting with some patients receiving more than one Gy (air kerma), which is suggested to be the threshold of deterministic radiation effects[8,9]. Few recent studies evaluating radiation exposure during interventional treatment of femoro-popliteal or below the knee stenosis demonstrated lower radiation doses, but without sufficient data regarding possible confounders. Despite the region and the complexity of the peripheral interventional procedure, type and performance of x-ray equipment, level of training in radiation protection, patients ´condition and operator´s experience may influence patients´ radiation exposure[10,11]. Moreover, pre-interventional diagnostic procedures as computed tomography, magnetic resonance angiography or vascular ultrasound and/or precise information about localisation of stenosis might influence radiation exposure in peripheral interventional procedures. However, there are no data regarding patients´ radiation exposure during peripheral interventional procedures dependent on type of vascular diagnostic procedures prior to angiography.
Herein, we report about the influence of pre-interventional diagnostic procedures on patients´ radiation dose during peripheral interventional procedures.
Materials and Methods
Procedural data of 289 patients were included into statistical analysis. Patients were predominantly male (male n = 167 (57.8%), female n = 122 (42.2%)) with an average age of 70.6 ± 11.3 years (range 41 - 95 years). Detailed patients characteristics are shown in table 1.
Table 1: Baseline characteristics of patients (BMI: body mass index; BSA: body surface area, mean ± SD (range).
| Number of patients (% of total) | |
| Total | 289 |
| Male | 167 (57.8%) |
| Female | 122 (42.2%) |
| Age | 70.6 ± 11.3 (41 - 95) years |
| BMI | 26.9 ± 4.9 (16.2 - 45.2) kg/m² |
| BSA | 1.89 ± 0.23 (1.27 - 2.73) m² |
| Fontaine Stadium I | 0 (00.0%) |
| II | 122 (42.2%) |
| III | 39 (13.5%) |
| IV | 128 (44.3%) |
All clinical procedures were performed with an operating C-arm unit (Allura Expert; Philips Medical Systems, Best, Netherlands). Available image-intensifier field sizes were 15, 22, 27, 31, 42 and 48 cm respectively and were used to the operator’s decision. Radiation exposure was analysed by total time of fluoroscopy as well as the dose area product (DAP, product of air kerma and defined x-ray beam cross-sectional area, Gy*cm²) assessing effective patients dose for evaluation of stochastic risk.
Data were analysed, depending on region of interventional procedures as well as previously available diagnostic information (ultrasound, magnetic resonance angiography (MRA) / computed tomography (CT) or previous angiography).
Statistical Analysis
Data are expressed as mean ± standard deviation (SD) or mean ± standard error of the mean (SEM) where applicable. Statistical significance was assumed at a p-level < 0.05. All variables were found to have Gaussian distribution (Shapiro-Wilk test), thus parametric tests were applied for statistical analysis. Means between two categories were compared with the student ´s-t-test or one-way-ANOVA with Newman-Keul posthoc analysis. Relation of variables was performed with linear correlation. Statistical analysis was performed using PSPP® for MacOs.
Results
Procedural data
Peripheral intervention was performed in 289 patients (iliac artery: 61 patients (21.1%), femoro-popliteal artery: 100 patients (34.6%), crural arteries: 72 patients (24.9%), multi-vessel intervention: 56 patients (19.4%)). Technical success or interventional methods were not considered for further analyses. Procedural characteristics were described in table 2. Patients radiation exposure was highest in iliac-intervention (101.32 ± 87.93 Gy*cm²) compared to multi-vessel intervention (74.67 ± 62.86 Gy*cm²), femoro-popliteal-intervention (68.10 ± 52.83 Gy*cm²) and crural-intervention (42.02 ± 25.41 Gy*cm²).
Table 2: Procedural characteristics of patients (mean ± SD (range)).
| Number of patients (% of total) (range) | |
| Region of interventional procedure | |
| iliac | 61 (21.1%) |
| femoro-popliteal | 100 (34.6%) |
| crural | 72 (24.9%) |
| multi-vessel | 56 (19.4%) |
| Pre-procedural diagnostics | |
| none | 93 (32.2%) |
| ultrasound | 52 (17.8%) |
| CT/MRA | 88 (30.5%) |
| angiography | 56 (19.5%) |
| Total fluoroscopy time | 18.3 ± 10.6 (1.8 - 63.1) min |
| Dose-Area-Product | 69.9 ± 62.4 (5.2 - 511.4) Gy*cm² |
There was a weak, but significant association of total time of fluoroscopy and total dose area product (r = 0.278, p < 0.01).
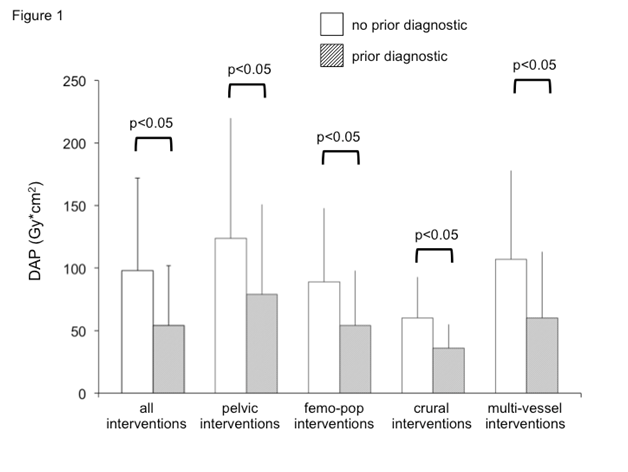
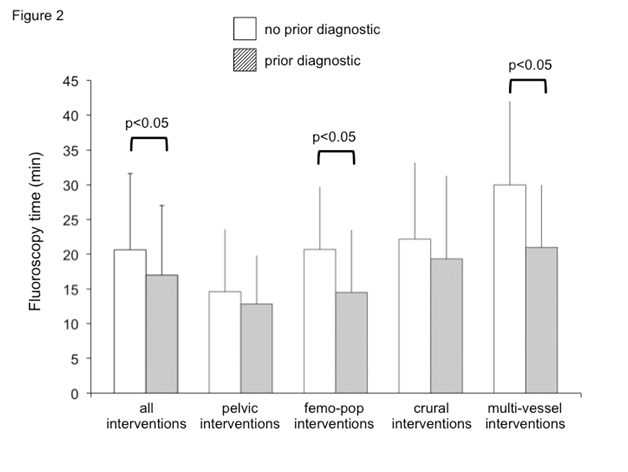
Prior information about vascular status of patients led to a significant decrease of the dose area product exposed to the patient, irrespective of the region of intervention (figure 1). However, fluoroscopy time also decreased in patients with prior vascular diagnostic procedures, but this was significant in femoro-popliteal and multi-vessel-interventional procedures only (figure 2).
Figure 1: Influence of information about vascular status on dose area product.
Detailed information about vascular status is associated with a significant decreased radiation exposure, irrespective of the region of intervention (mean ± standard error of the mean (SEM), dose area product, DAP).
Figure 2: Influence of information about vascular status on fluoroscopy time.
Detailed information about vascular status decreased fluoroscopy time in femoro-popliteal and multi-vessel interventions significantly (mean ± standard error of the mean (SEM).
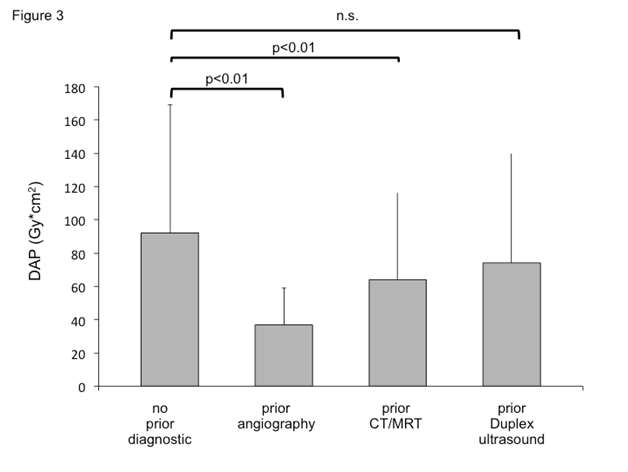
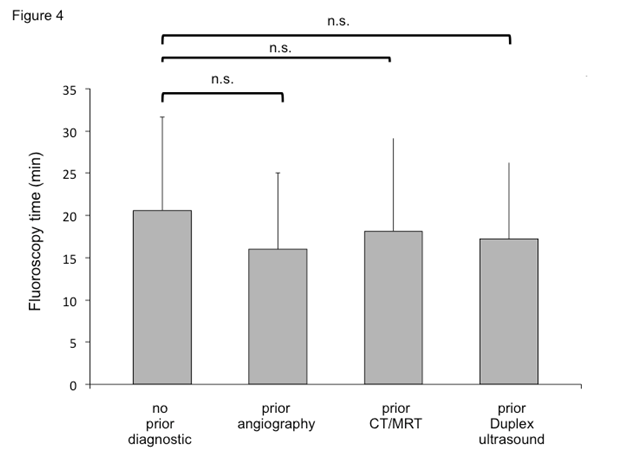
Reduction of radiation exposure was significant in patients with a prior angiography or a CT- or MR-angiography, whereas a diagnostic vascular ultrasound tended to decrease radiation exposure of patients with a subsequent interventional procedure only (figure 3). Fluoroscopy time was not affected by the kind of diagnostic procedure (figure 4).
Figure 3: Influence of previous vascular imaging on patients´ radiation exposure.
Patients´ radiation exposure (dose area product, DAP) is dependent on previous vascular imaging in patients with peripheral intervention (mean ± standard error of the mean (SEM)).
Figure 4: Influence of previous vascular imaging on fluoroscopy time.
Type of vascular imaging prior to peripheral interventional procedures had no influence on fluoroscopy time (mean ± standard error of the mean (SEM)).
Discussion
Recently, more frequent and complex use of peripheral interventional procedures led to an increased radiation exposure of patients. The data presented in this study demonstrate a significant reduction of patients´ radiation exposure by using non-invasive vascular diagnostic procedures as CT- or MRT-angiography prior to the interventional procedure.
Complexity of peripheral interventional procedures was increased during the last decade with subsequently enhanced fluoroscopy times and radiation doses for both, patients and physicians. Highest radiation dose was documented in interventional procedures of the iliac arteries, with a mean DAP of 100 Gy*cm². This is at a lower level compared with previous studies, revealing patients radiation doses of about 150 - 200 Gy*cm2[9,12-14]. Radiation exposure in interventional procedures of femoro-popliteal arteries as well as below the knee interventions were in line with recent data (30 - 100 Gy*cm²)[9,13]. In summary, patient´s radiation doses in peripheral interventional procedures are in a range of about 30 Gy*cm² for below the knee procedures, up to more than 200 Gy*cm² for iliac or combination procedures.
Although radiation doses are strongly dependent on technical equipment and individual skill of the physician, there were no data in literature regarding possible reduction of radiation doses dependent on pre-interventional diagnostic procedures[9,15]. We demonstrated a significant decrease of the DAP by nearly one half, when information of vascular status was present. Precise information about vascular status and localisation of possible stenosis renders imaging of vessels proximal and distal of the region of interest redundant and might therefore limit radiation exposure of both patients and physicians. In comparison to the reduction of DAP, the demonstrated effects were weaker regarding fluoroscopy time. A significant decrease was shown in femoro-popliteal and multi-vessel interventions only. However, registration of fluoroscopy time alone does not seem to be sufficient for assessment of deterministic and stochastic radiation effects, as about 70% of the total DAP is suggested to be the result of acquisition frames and 30% being applied by fluoroscopy only[16]. In our patients, we found a weak correlation of DAP and fluoroscopy time only, which is in line with previous data of peripheral interventional procedures[11]. Thus, fluoroscopy time information might underestimate patients´ radiation exposure, especially in peripheral interventional procedures. In contrast, recent studies demonstrated a strong correlation of fluoroscopy time and DAP in coronary interventions, which might rely on a mainly static x-ray tube in coronary procedures[15].
Decrease of radiation exposure during peripheral intervention was highest in patients with prior conventional angiography. Reduction of DAP was nearly two third in those patients. Prior CT- or MR-angiography resulted in a dose reduction of one third, which accords to a decrease of about 30 Gy/cm² or estimated 6 mSv. In patients with previous duplex ultrasound, there was a slight, but not significant reduction of 18 Gy/cm². This is likely due to both, operator and patient dependent limitation of duplex ultrasound as well as limited accuracy in certain vascular regions (i.e. iliac and crural arteries)[17]. The lower sensitivity (88%) and specificity (95%) of duplex ultrasound compared to CT- or MRT-angiography corresponds to the result of slight dose limitation in subsequent peripheral interventional procedure[17]. However, duplex ultrasound should be the first choice in vascular diagnostic procedure due to the cost effectiveness and abdication of ionizing radiation, especially in patients with femoro-popliteal lesions. If duplex ultrasound fails to identify precise localisation of stenosis, especially in the pelvic region as well as below the knee, CT- or MR-angiography both provide accurate assessment of vascular status with a decrease of radiation exposure in following interventional procedures. However, whenever possible, MR-angiography should be the first choice due to the absence of any radiation. Radiation exposure of prior CT-angiography might outweigh subsequent reduction during the interventional procedure. In a direct comparison of digital subtraction angiography with a 16-slice CT-angiography, effective radiation dose was about four times higher with DSA, but nevertheless with an estimated dose of 8 - 20 Gy/cm² for the CT-angiography[18]. Recently, a study with a 64-slice CT-angiography equipment showed increased radiation doses of estimated 25 - 50 Gy/cm²[19]. However, this level of radiation exposure is suggested to out value the benefit demonstrated in our study.
The study is limited by measuring fluoroscopy time and DAP, but not the effective dose of patients´ radiation exposure. Nevertheless, DAP was demonstrated to have a strong correlation with the effective dose estimated by multiplying DAP with specific conversion coefficients in patients undergoing angiography of the lower limb[20].
In conclusion, patients´ radiation dose during peripheral interventional procedures is strongly dependent on vascular region, precise information about vascular status and previous vascular imaging. Thus, physicians should emphasize accurate vascular diagnostic procedures prior to peripheral intervention.
Conflict of interest:
Both authors have neither a conflict of interest nor a financial disclosure.
References
- 1. Krüger, K., Bödeker, M., Hellmich, M., et al. Effect of a one-session versus two-session procedure on different parameters of interventional therapy for peripheral arterial occlusive disease: results of a retrospective cohort study. (2010) J Vasc Interv Radiol 21(4): 452-458.
Pubmed || Crossref || OThers - 2. Bor, D., Toklu, T., Ol?ar, T., et al. Variations of patient doses in interventional examinations at different angiographic units. (2006) Cardiovasc Intervent Radiol 29(5): 797-806.
Pubmed || Crossref || OThers - 3. Padovani, R., Bernardi, G., Malisan, M.R., et al. Fioretti PM. Patient dose related to the complexity of interventional cardiology procedures. (2001) Radiat Prot Dosimetry 94(1-2): 189-192.
Pubmed || Crossref || OThers - 4. Fransson, S.G., Persliden, J. Patient radiation exposure during coronary angiography and intervention. (2000) Acta Radiol 41(2): 142-144.
Pubmed || Crossref || OThers - 5. Bernardi, G., Padovani, R., Morocutti, G., et al. Clinical and technical determinants of the complexity of percutaneous transluminal coronary angioplasty procedures: analysis in relation to radiation exposure parameters. (2000) Catheter Cardiovasc Interv 51(1): 1-9.
Pubmed || Crossref || OThers - 6. Yo, S., Chino, M., Hasegawa, T., et al. Actual state of radiation exposure during coronary angioplasty: a multicenter study in the nationwide database for cost analysis of percutaneous transluminal coronary angioplasty in Japan. (2003) Circ J 67(8): 676-681.
Pubmed || Crossref || OThers - 7. Bakalyar, D.M., Castellani, M.D., Safian, R.D. Radiation exposure to patients undergoing diagnostic and interventional cardiac catheterization procedures. (1997) Cathet Cardiovasc Diagn 42(2): 121-125.
Pubmed || Crossref || OThers - 8. Greenhalgh, R.M., Brown, L.C., Kwong, G.P., et al. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. (2004) Lancet 364(9437): 843-848.
Pubmed || Crossref || OThers - 9. Majewska, N., Blaszak, M.A., Juszkat, R., et al. Patients' radiation doses during the implantation of stents in carotid, renal, iliac, femoral and popliteal arteries. (2011) Eur J Vasc Endovasc Surg 41(3): 372-377.
Pubmed || Crossref || OThers - 10. Pantos, I., Patatoukas, G., Katritsis, D.G., et. Patient radiation doses in interventional cardiology procedures. (2009) Curr Cardiol Rev 5(1): 1-11.
Pubmed || Crossref || OThers - 11. Arif, S., Bartus, S., Rakowski, T., et al. Comparison of radiation dose exposure in patients undergoing percutaneous coronary intervention vs. peripheral intervention. (2014) Postepy Kardiol Interwencyjnej 10(4): 308-313.
Pubmed || Crossref || OThers - 12. Dendy, P.P. Radiation risks in interventional radiology. (2008) Br J Radiol 81(961): 1-7.
Pubmed || Crossref || OThers - 13. Peruzzo Cornetto, A., Pasquino, M., Aimonetto, S., et al. Interventional radiology at a single institution over 9 years: a comprehensive evaluation of procedures and an estimation of collective effective dose. (2012) J Vasc Interv Radiol 23(12): 1665-1675.e2.
Pubmed || Crossref || OThers - 14. Segal, E., Weinberg, I., Leichter, I., et al. Patient radiation exposure during percutaneous endovascular revascularization of the lower extremity. (2013) J Vasc Surg 58(6): 1556-1562.
Pubmed || Crossref || OThers - 15. Walsh, S.R., Cousins, C., Tang, T.Y., et al. Ionizing radiation in endovascular interventions. (2008) J Endovasc Ther 15(6): 680-687.
Pubmed || Crossref || OThers - 16. Pitton, M.B., Kloeckner, R., Schneider, J., et al. Radiation exposure in vascular angiographic procedures. (2012) J Vasc Interv Radiol 23(11): 1487-1495.
Pubmed || Crossref || OThers - 17. Owen, A.R., Roditi, G.H. Peripheral arterial disease: the evolving role of non-invasive imaging. (2011) Postgrad Med J 87(1025): 189-198.
Pubmed || Crossref || OThers - 18. Willmann, J.K., Baumert, B., Schertler, T., et al. Aortoiliac and lower extremity arteries assessed with 16-detector row CT angiography: prospective comparison with digital subtraction angiography. (2005) Radiology 236(3): 1083-1093.
Pubmed || Crossref || OThers - 19. Oca Pernas, R., Delgado Sánchez-Gracián, C., Silva Priegue, N., et al. Comparison of image quality and radiation dose in computed tomography angiography of the peripheral arteries using tube voltage of 80 kV versus 100 kV. (2014) Radiologia 56(6): 541-547.
Pubmed || Crossref || OThers - 20. Smans, K., Struelens, L., Hoornaert, M.T., et al. A study of the correlation between dose area product and effective dose in vascular radiology. (2008) Radiat Prot Dosimetry 130(3): 300-308.
Pubmed || Crossref || OThers