Institutional Factors Associated with Maternal Mortality That Occurred from 1 January to 31 December 2013 at Major Admitting Health Facilities in Midlands Province, Zimbabwe
Hellen Dziwa, Gilbert Utshudienyema Wembodinga, Elliot Chikaka, Chemhuru Milton, Elizabeth Chadambuka
Affiliation
Faculty of Health Sciences, Africa University
Corresponding Author
Auxilia Chideme-Munodawafa, Faculty of Health Sciences, Africa University, PO Box 1320, Mutare,Zimbabwe; E-mail: chidemea@africau.edu
Citation
Chideme-Munodawafa, A., et al. Institutional Factors Associated with Maternal Mortality that Occurred from 1st January to 31st December 2013 at Major Admitting Health Facilities in Midlands Province, Zimbabwe. (2017) J Gynecol Neonatal Biol 3(1): 14-21.
Copy rights
© 2017 Chideme-Munodawafa, A. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Institutional factors; Maternal mortality; Zimbabwe
Abstract
Introduction: In Midlands Province, Zimbabwe during the period 1st January to 30th September 2013, 43 (80%) maternal mortality had occurred in health facilities raising questions on the quality and timeliness of care rendered to maternity cases when they arrive at health facilities.
Methods: A facility based cross-sectional study was conducted from February to April 2013 to determine institutional factors associated with maternal mortality that occurred in nine major admitting health facilities from 1st January to 31st December 2013. Data was collected using self administered questionnaires on knowledge and skills from 65 HCWs, interview guide on availability of life saving interventions from 18 managers and checklist on 38 maternal mortality cases.
Results: Sixteen (25%) health care workers (HCWs) were trained in Emergency Obstetric Care (EmOC). Only 13(20%) were able to perform vacuum extraction delivery and 57% can perform manual removal of placenta and Manual Vacuum Aspiration (MVA). Incomplete documentation, inadequate investigations and monitoring, delays in getting appropriate care and transportation, lack of blood and blood products, not following guidelines, inappropriate attitudes and lack of follow up of HIV clients were identified as gaps in the care rendered to maternal mortality cases before death. Unavailability and inadequacy of life saving interventions was identified.
Discussion: With these major findings, reduced number of skilled HCWs to perform life saving procedures, substandard quality of care and unavailability and inadequate life saving interventions at the nine major admitting health facilities were associated with maternal mortality that occurred from 1st January to 31st December 2013 in Midlands Province. Scaling up of EmOC training, follow up sessions on EmOC trained HCWs, upgrading of major health facilities to offer all life saving interventions and ensure availability of adequate resources is recommended so as to reduce maternal with the aim of achieving Millennium Development Goal five.
Introduction
Maternal mortality is a global problem more concentrated in developing and low-income regions especially Sub-Saharan Africa (SSA) contributing 56% of the burden[1]. Access to timely and appropriate care during antenatal, child birth and post partum period is critical to survival[2]. Maternal mortality is defined as “the death of a woman while pregnant or within 42 days after the pregnancy ends, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not accidental or incidental causes”[3]. Direct maternal mortality results from obstetric complications of the pregnancy state and indirect mortality occurs due to existing diseases aggravated by physiologic effects of pregnancy[4].
Reduction of maternal mortality is a global priority in line with Millennium Development Goal (MDG-5) which aims at reducing maternal mortality by 75% between 1990 and 2015[5]. Knowledge, skills, functional equipment, supplies and adequate infrastructure are prerequisites for timely and appropriate care. Health Care Worker (HCW) ability to detect problems is critical to timelines and appropriateness of the care[6]. Globally in 2010, 285 000 maternal mortality occurred with 800 women dying daily[7]. The WHO European region maternal mortality ratio decreased from 35 / 100 000 live births in 1990 to 16 / 100 000 live births in 2008[8].
In 2008 all SSA countries had maternal mortality ratio of 280/100 000 live births and higher[9]. SSA has low socio-economic conditions, nutrition, access and provision of life saving obstetric care services[10]. South Asia made a 53% reduction in maternal mortality between 1990 and 2008 but SSA had only 26%[11]. India had more than 100/100 000 live births[12].
In Zimbabwe maternal mortality increased from 283/100 000 in 1994 to 725/100 000 in 2007 then 960/100 000 in 2010/ 2011, approximately ten women dying daily[13,14]. Midlands Province in Zimbabwe had an estimated maternal mortality ratio of 502/100 000 live births[15].
In 2005, 80% of maternal mortality globally were due to Post Partum Hemorrhage (PPH), puerperal sepsis, pre-eclampsia/ eclampsia (PIH), unsafe abortions and obstructed labor. Malaria and AIDS contributed to 20%[16]. In 2007 PPH, PIH, puerperal sepsis and abortion were major direct causes of maternal mortality in Zimbabwe[17]. Risk of maternal mortality is higher in adolescence with probability of dying higher in developing countries[18].
Globally about 8 million women have PPH yearly[19]. Active management of the third stage of labor was proved to prevent PPH[20]. Globally, 10 million women develop pre-eclampsia/eclampsia with about 76 000 maternal mortality[21]. Eclampsia is Pre-eclampsia complicated by convulsions and or coma[22] and leads to multiple organ failure[23]. Interventions aim to reduce complications thereby maximizing survival[24]. Sepsis refers to bacterial infection of the genital tract after child birth[25], contributed to 7.8% mortality during 2007, in Zimbabwe[17].
About 21 million unsafe abortions occur yearly, mostly in developing countries[26] Abortion is expulsion of products of conception with fetus weighing below 500 grams or gestational age below 20 weeks[27]. Fetal chromosomal factors contribute to 50 - 60% of abortions[28]. A live birth is complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of the pregnancy, which, after such separation, breathes or shows any other evidence of life for example beating of the heart, pulsation of the umbilical cord or definite movement of the voluntary muscles[29].
Maternal mortality occurs from women who arrive too late, suddenly develop fatal complications and those who fail to get timely and effective appropriate interventions[30]. Reports for Zimbabwe in 2012 showed a drop of skilled attendance from 69% in 2009 to 66.2% in 2010 - 2011 periods[31]. Compromised functionality and accessibility retard provision of emergency care especially in developing countries 32.
Statement of the Problem
In Midlands Province, Zimbabwe, Maternal Mortality was a problem of concern and for the period 1 January to 30 September 2013, 54 maternal deaths were reported with 43 (79.6%) within health facilities, yet it is expected that women receive life saving interventions once they reach the health facilities (Midlands Province Statistics for 2013). Seventeen (31.5%) women were aged between 16 and 24 years. The large percentage of hospital deaths raises questions on the quality of care rendered within health facilities.
Broad objective
The study aimed to determine factors associated with maternal mortality at nine major admitting health facilities during period 1st January to 31st December 2013.
Specific objectives
1. Determine knowledge levels on Emergency Obstetric Care (EmOC) of HCWs in Midlands Province health facilities.
2. To compare the knowledge skills between the HCW trained and untrained
3. To describe the demographic history of the maternal mortality cases who died in the health facilities,
4. To describe the obstetric history of the maternal mortality cases, analyze the emergency obstetric care rendered to each of the maternal mortality cases
5. To determine lifesaving intervention availability at each of the health facilities.
Methods
A facility based cross sectional study was conducted in Midlands Province’s eight districts major admitting health facilities. The total province population was 1 638 701 and 327 740 women of child bearing age with 81 935 expected pregnancies and 65 548 expected births (Midlands Province Statistics for 2013).
Eighteen managers were purposively selected that is 7 District Medical Officer (DMOs,) 2 medical superintendents and 9 Senior Nursing Officers. Convenience sampling was used to select 65 HCWs from the maternity departments of nine major admitting health facilities where nurses and doctors found on duty were recruited. The 2013 maternity admission registers, maternity delivery registers, maternal mortality notification forms, maternal mortality audit reports and medical records of 38 maternal mortality cases were purposively selected for review from the 8 health facilities.
A self-administered, pre-tested questionnaire was used to collect data on EmOC knowledge levels and skills from the HCWs. Excellent score ranged from 20% – 30% , 20 - 25% Very Good, and 10 – 20 % good, 0 -5 poor a checklist was used to summarize demographic and obstetric history and care rendered to cases from time of admission until death. An interview guide was used to collect data on availability of life saving interventions. Quantitative data was analyzed using Epi–Info 7.1.1.1 and qualitative data was analyzed manually.
Ethical Considerations
Permission was sought and granted from Africa University Faculty of Health Sciences, Provincial Medical Director for Midlands Province, District Medical Officers and Medical Superintendents. The proposal was approved by the Africa University Research Ethics Committee. A written, informed Consent was obtained from participants during data collection and anonymity was maintained throughout. Privacy and confidentiality was maintained throughout the study.
Results
Table 1: The professional characteristics and Emergency Obstetric Care (EmOC) training of participants in the study on INSTITUTIONAL FACTORS ASSOCIATED WITH MATERNAL MORTALITY THAT OCCURRED FROM 1st JANUARY TO 31st DECEMBER 2013 AT MAJOR ADMITTING HEALTH FACILITIES IN MIDLANDS PROVINCE, ZIMBABWE.
| N-65 | ||
|---|---|---|
| Gender | F - 53 (80%) | M - 13 (20%) |
| Age | 31- 40 years | Median 35 years |
| Trained midwives | 48 (74%) | |
| State Certified Maternity Nurses | 7 (11%) | |
| Registered General Nurses (no midwifery) | 3 (5%) | |
| Doctors | 2 (3%) | |
| Primary Care Nurses (Nurses’ aides) | 16 (25%) | |
| Trained in EmOC Midwives | 13 | |
| Trained in EmOC Doctors | 2 | |
| Trained in EmOC state certified maternity nurse. | 1 | |
| Total Trained in EmOC | 16 (25%) | |
Fifty one (78.5%) were able to describe eclampsia and 61 (94%) mentioned magnesium Sulphate as the recommended drug used in pre-eclampsia/eclampsia.
HCW knowledge
Table 2: HCW skills summary.
| VARIABLE | CHARACTERISTIC | TRAINED n = 16 (%) | UNTRAINED n = 16 (%) | Odds Ratio (95% Confidence Interval) | P-value |
|---|---|---|---|---|---|
| Antibiotic administration | Yes | 14 (88) | 45 (92) | 0.6 (0.10, 3.77) | 0.630 |
| No | 2 (12) | 4 (8) | |||
| Oxytocin administration | Yes | 15 (94) | 47 (96) | 0.6 ( 0.05,7.54) | 1.000 |
| No | 1 (6) | 2 (4) | |||
| Mag Sulphate administration | Yes | 15 (94) | 46 (94) | 0.98 (0.09, 10.12) | 1.000 |
| No | 1 (6) | 3 (6) | |||
| Manual | Yes | 15 (94) | 22 (45) | 18.4 (2.25,150.10) | < 0.001* |
| Removal of placenta | No | 1 (6) | 27( 55) | ||
| Removal of retained products | Yes | 14 (88) | 23 (47) | 7.9 (1.62,38.58) | 0.007* |
| No | 2 (12) | 26 (53) | |||
| Vacuum extraction delivery | Yes | 8 (50) | 5 (10) | 8.8 (2.29,33.86) | 0.001* |
| No | 8 (50) | 44 (90) | |||
| Blood transfusion | Yes | 14 (88) | 45 (92) | 0.6 (0.10,3.77) | 0.630 |
| No | 2 (12) | 4 (8) | |||
| Operative delivery | Yes | 2 (12) | 1 (2) | 0.15 (0.01, 1.73) | 0.147 |
| NA | 14 (88) | 48 (98) |
*P- value < 0.05 = statistically significant and p-value > 0.05 = not statistically significant
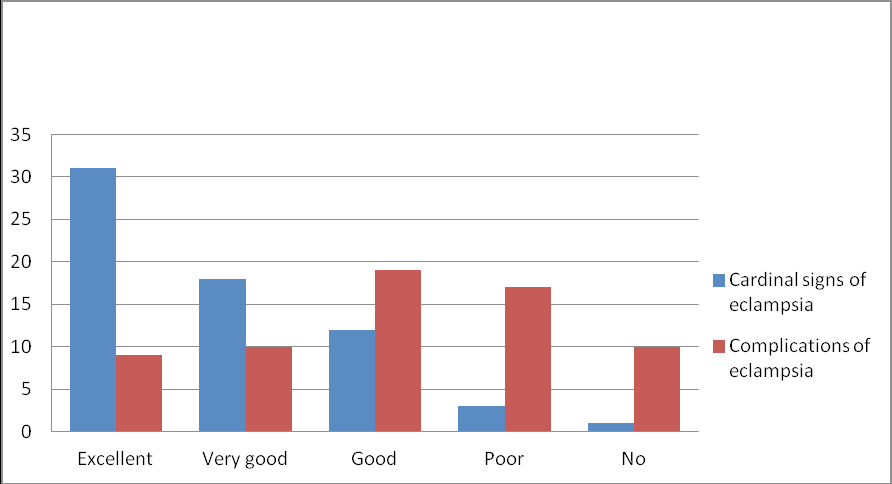
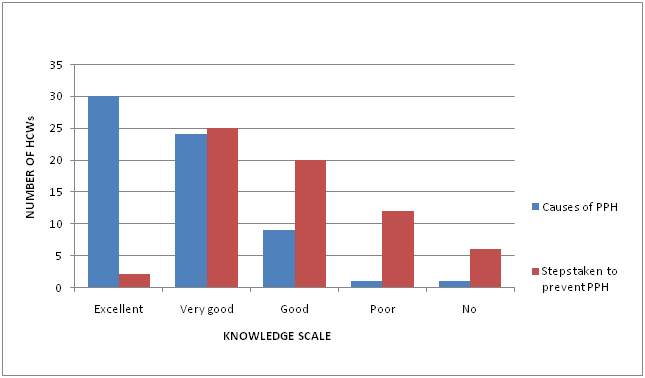
More than 50 %?) 32 (48%) could describe the cardinal signs of eclampsia and 9 (14%) had knowledge on the complications of eclampsia Forty six (71%) of the participants were able to describe Post partum hemorrhage (PPH) while 30 (46%) had knowledge on the causes of PPH and only two (3%) had knowledge on steps taken to prevent PPH (Figure 2)
Figure 1: Knowledge on cardinal signs and complications of eclampsia.
Figure 2: Knowledge on causes and steps to prevent PPH.
Fifty (77%) correctly described puerperal sepsis. Only two participants (3%) were able to describe knowledge on infection control measures and 31 (48%) had good knowledge while 24 (37%) had poor knowledge.
HCW skills on EmOC
HCWs trained in EmOC were able to perform life saving skills compared to the untrained
Demographic history of participants
Minimum age was 15 years and the maximum 44 years. Twenty (52%) were in the 25 to 34 years age group and had attained secondary school level of education. Thirty two (84%) were housewives. Twenty one (55%) resided in the rural areas and 35 (92%) were married.
Obstetric history
Table 3: Summary of obstetric history of maternal mortality cases.
| VARIABLE | CHARACTERISTICS | FREQUENCY Total number = 38 (percentage) |
|---|---|---|
| Parity | First pregnancy | 5 (13) |
| Multigravida | 33 (87) | |
| Gestational age | Unknown | 7 (18) |
| First trimester | 1 (3) | |
| Second trimester | 4 (11) | |
| Third trimester | 26 (68) | |
| Booking status | Booked 24 | (61) |
| Unbooked | 13 (34) | |
| Unknown | 1 (3) | |
| HIV status | Positive | 15 (39) |
| Negative | 13 (34) | |
| Unknown | 10 (26) | |
| Timing of death | Post delivery | 22 (58) |
| Before delivery | 16 (42) |
Care rendered
In 12 (32%) cases proper documentation and adequate history taking was lacking. Adequate monitoring was lacking in 11 (29%) cases. Inadequate investigations were noted in 9 (24%) cases. Lack of blood and other blood products for resuscitation was identified as a contributing factor on 5 (13%) cases Lack of following guidelines in eclampsia, diabetes mellitus and malaria in pregnancy was identified during the care of 4 (11%) cases. Inappropriate attitudes and poor communication between facilities was noted in 3 (8%) cases. Delays in transportation and insufficient ambulances were identified in 7 (18%) cases.
Availability of life saving interventions
Administration of parenteral antibiotics, oxytocin, magnesium sulphate and manual removal of placenta were available at all facilities. Manual Vacuum Aspiration (MVA) and Vacuum Extraction Delivery (VED) interventions were available at 8 (89%) facilities. Surgical intervention (Caesarian Section) and blood transfusion was available at 7 (78%) facilities. All the facilities were providing transport to refer out maternity cases and also reported having a doctor on call for 24 hours. Eight (89%) provided transport to referred in clients and at one facility clients were using own transport, public transport or hiring private vehicles. Six (67%) of the facilities had an anesthetist available for 24 hours. None of the nine facilities had an Intensive Care Unit (ICU) for the care and monitoring of critically ill patients.
Discussion
The study aimed to find institutional factors contributing to maternal mortality. Financial, physical, socio-cultural and health system factors were seen to be interrelated in influencing maternal mortality[33]. Only 16 (25%) HCWs working at the major admitting health facilities had been trained in EmOC yet there is need for efficiency and effectiveness in emergency obstetric care which is achieved through training. Similar results were found in Nigeria[35] on HCW training where only 9% had been trained and were not managing the pregnant women according to global best practices. In Somalia, evaluation after EmOC training showed that training had impacted positively on the knowledge and skills resulting in the HCWs reporting improved confidence[36]. Increasing the number of HCWs trained in EmOC will go a long way in reducing maternal mortality as training empowers HCWs with knowledge and skills thereby enabling provision of quality care.
Thirty two (32%) had excellent knowledge on cardinal signs of eclampsia and of concern only nine (14%) had excellent knowledge on the complications of eclampsia. Poor knowledge hinders HCWs ability to give health education on danger warning signs and complications of eclampsia. Also results in poor screening, monitoring and care of pregnant women with abnormal blood pressure. Complication of pre-eclampsia to eclampsia can be rapid hence the need for proper monitoring and care aimed at reducing further complications thereby maximizing survival. Results in this study imply that if HCW skills are not improved then maternal mortality will not be reduced hence MDG five will not be achieved.
Similar results were found in Zimbabwe during an assessment in 2012[37] where 2% screened for pre-eclampsia during antenatal care, 12% did counseling on danger warning signs and 11% screened for pre-eclampsia and eclampsia during labor and delivery.
Thirty (46%) of the respondents had excellent knowledge on causes of PPH and only two (3%) had excellent knowledge on the steps taken to prevent PPH. HCWs need to be highly knowledgeable to enable them to act swiftly in preventing and arresting hemorrhage. These findings may be the reason why the cases would get substandard care from the time they were admitted hence contributing to maternal mortality.
Sepsis was found to be among maternal complications contributing to 80% of maternal deaths[38]. Poor knowledge on infection control measures was noted and no one had excellent knowledge on when to give prophylactic antibiotics. Prevention of sepsis by following recommended infection control measures and administration of prophylactic antibiotics is important. Inadequate knowledge on these aspects contributes to none practice thereby leading to sepsis. Similarly during 2012 in Zimbabwe only 46% of HCWs provided prophylactic drugs when indicated 37.
Fifty two (80%) of the respondents were unable to perform VED, 43% are unable to perform MVA and manual removal of placenta. HCW skills are important and if not prioritized poor quality care is provided to the pregnant women. In Nairobi 20% could perform manual removal of placenta, 16% dilatation and curettage, 9% MVA and 8% assisted vaginal delivery[39]. MVA and manual removal of placenta are major skills needed in management of the leading cause of maternal mortality, hemorrhage. If HCWs cannot readily perform the procedures, time is lost waiting for the few who are skilled hence lack of timely and appropriate care.
HCWs trained in EmOC were more likely able to perform VED, Manual removal of placenta and removal of retained products. Findings indicate need for training as a strategy to improve HCWs skills hence help them to offer quality care and avoid the delay in getting appropriate care once women have reached a health facility.
Demographic history participants
20 (52%) of the 38 cases were aged 25 to 34 years almost similar to results of 2011 in Ghana where mortality was highest among women aged 25 to 29 years[40] and different from 2013 results in Zimbabwe where majority were aged 16 to 20 years[41].
Twenty (53%) of cases had attained secondary school level of education. As a result of the low level of education majority 32 (84%) of the cases were housewives. Reaching tertiary level of education and becoming a professional woman impacts on a woman’s decision making and understanding of health education given thereby reporting early to a health facility. In a similar study in Zimbabwe unprofessional women had contributed to 83% of the deaths in 2011[42]. Findings therefore indicate that unprofessional women are more likely to die of pregnancy related complications.
Majority 35 (92%) of the cases in this study were married and similarly in Zimbabwe 82% of cases were married in 2011[42]. Marital status of a woman impacts on decision making on seeking medical help as in-laws and husbands must be consulted first and time is lost during the process.
Place of residence affects access to quality care in time. Twenty one (55%) resided in the rural area. Similarly during 2013 in India it was found that 87% resided in rural areas and time was lost whilst travelling to health facilities 43. Bad road network increased time taken travelling to nearest health facility and major hospital, thereby highlighting the need for availability of life saving interventions within reach so as to save lives. The high percentage of cases from the rural areas indicates the discrepancy in resource distribution between rural and urban health facilities where the rural facilities are disadvantaged.
Obstetric history
Parity, not booking, having bleeding complications in labor, delivery and post delivery were identified to be contributing factors to maternal mortality. Thirty three (84%) of the cases were multigravida and these findings show that the risk of dying increases with each subsequent pregnancy. Similarly in India, in a study done in 2011 majority 22 (58%) of the cases were multigravida women[44].
Booking with ANC is one strategy in reduction of maternal mortality and women are expected to be screened for risk factors, abnormalities like anemia corrected, infections treated, health education given and the mode of delivery decided. Twenty four (61%) of the cases were booked and 13 (34%) were unbooked. The high number of booked mothers raises questions on the quality antenatal care being offered in the health facilities. One booked woman with 4 ANC visits did not have a single blood pressure reading recorded on her card and later died of eclampsia. Different findings were reported from India in 2013 where 94.32% of the cases were unbooked[43]. These results indicate the need to equip HCWs with knowledge and skills to provide quality antenatal care hence reduce maternal mortality.
Twenty two (58%) of the cases died post delivery and 17 (45%) after having vaginal delivery. Most complications are concentrated around labor, delivery and immediate post delivery period especially the first 24 hours. Therefore there is need for quality care and monitoring including proper estimation of blood loss. Similar findings were reported in India in 2013 where 71.16% of the cases died post delivery[43].
Twenty seven (71%) of deaths were due to direct causes with bleeding accounting for the larger proportion 18 (47%) with the common causes being PPH, APH, ruptured uterus, ectopic pregnancy and abortion. Management of bleeding complications requires prompt appropriate action as delays will lead to more blood being lost leading to death. Similar findings were reported during 2013 in Ethiopia where hemorrhage was found to be a major cause of death[45]. Early referrals, quick efficient and well equipped transport facilities will reduce time lost during transportation of clients between facilities. Improvement in blood investigation, proper interpretation of blood results, availability of blood and fresh frozen plasma will reduce hemorrhage related deaths there by reducing maternal mortality.
Care rendered
On admission baseline vital observations were not recorded yet every client is expected to have the vital signs observations checked for future comparison and if done they pave way for correct assessment hence appropriate interventions. Poor monitoring in terms of no vital signs observations being monitored as well as intake and output recordings during follow up care was observed and this results in incorrect evaluation. If monitoring is done it helps in evaluation of effectiveness of care being rendered thereby promoting timely and appropriate interventions. The lack of monitoring indicates the need for monitors and ICU especially at the provincial hospital where critically ill maternity cases are referred to by the district hospitals. Similar findings were reported in Morocco in 2013 where insufficient follow up of care was identified in 45.6% of the cases[46].
Gaps in care were also identified in terms of incomplete investigations, unavailability of blood and blood products with two facilities not having blood bank. Hemorrhage was found to be the major cause of death and this study was found to be attributable to delayed or failed blood transfusion. In 2010 in Bangladesh it was also found out that delayed or failed blood transfusion contributed to 40% of maternal mortality[47].
Delays in providing appropriate and prompt care was identified due to several aspects for example inappropriate interventions, taking too long in transfer process resulting in clients dying on the way to next level or before departure, inappropriate fluids and delays in arresting hemorrhage. Improving HCW knowledge and skills will help in solving the delays. Not following guidelines was noted especially in the management of malaria, eclampsia, and diabetes mellitus in pregnancy and in HIV clients who were pregnant. Use of guidelines is important in the management of conditions as the set protocols are research based and proven to be among the best practice to maximize maternal survival hence the need to ensure availability of the guidelines at all health facilities.
Negative attitudes and poor communication among HCWs was identified and contributed to maternal mortality in the care of pregnant women with complications where treatment was denied and this resulted in delay in getting quality care as time was lost travelling between health facilities. Findings reveal the importance of client’s needs versus physical boundaries and referral channels. Access to quality care is also affected by HCW attitudes besides distance, transport and availability. Similar negative attitudes of doctors were found to be a contributing factor to maternal mortality in Bangladesh during a 2010 study[47].
Availability of life saving interventions
Gaps in the existence and functionality of EmOC services compromise quality care thereby affecting maternal survival. Lack of the life saving interventions at any one health facility expected to offer the interventions leads to delays in getting quality care once the woman has reached the health facility as time will be lost during transfer to the next facility. All nations need to invest in providing equitable and adequate maternal health services by improving availability, accessibility, quality and utilization of life saving interventions to achieve MDG 5.
MVA and VED interventions were not available at all health facilities due to lack of infrastructure and equipment therefore women requiring the intervention were transferred to the next level including surgical interventions and blood transfusion. Remote health facilities with poor road network were mostly having unavailability and inadequate life saving interventions. Unavailability coupled with distance increased the risk of delay in getting timely and appropriate care. These interventions are very important in the reduction of maternal mortality related to hemorrhage which was found to be a major cause of death in this study and audit done in Zimbabwe during 2010/11 period[48]. Other identified factors for the unavailability of surgical interventions were none availability of anesthetist or use of untrained ones who are incompetent thereby compromising quality of care and contributing to maternal mortality. Due to unavailability of ICU critically ill cases were nursed in a special bay without equipment and monitors and vital signs observations done manually with the same HCWs taking care of the other patients, disadvantaging the critically ill. Lack of ICU compromises follow up of care and proper monitoring and in this study lack of monitoring was identified as a contributing factor to maternal mortality in nine cases and need for ICU was noted also in nine cases that needed critical care, support and monitoring. Similarly availability of life saving interventions was below expected standards in Malindi District, Kenya in 2013[49] and in Nigeria during 2009[50].
Implications
Findings have implications on practice, policy and education. Training needs on EmOC need to be prioritized to empower HCWs with appropriate skills especially in the management of emergency cases. Inclusion of follow up practice sessions at health facilities after EmOC training will improve practice. Policy priority would be on setting effective and efficient transport and referral policies to deal with transport delays as well as on availability of all life saving interventions at all major admitting health facilities. Education curricula for nurses and doctors have to adopt EmOC training guidelines so as to produce competent graduates rather than waiting to train them after graduation.
Conclusion
There was a low percentage of EmOC trained HCWs, not all were able to perform life saving skills expected. Maternity cases were not getting quality care in time when they had reached the health facilities. Life saving interventions was not available at all nine major health facilities and those providing at times failed to do so due to lack of resources especially blood and other blood products. Absence of trained personnel, equipment and infrastructure also contributed to unavailability of the life saving interventions. These institutional factors were associated with maternal mortality that occurred during 2013 in Midlands Province, Zimbabwe.
Recommendations
With these findings the following recommendations are expected to reduce maternal mortality in Midlands Province. Training of HCWs is vital in the reduction of maternal mortality Therefore scaling up of EmOC training to increase percentage of trained HCWs from current estimation of 25% to above 50% is recommended. Practical follow up sessions on EmOC trained HCWs to strengthen skills. HCWs encouraged following of guidelines when rendering care. Responsible authorities are encouraged to improve availability of resources and upgrade facilities with inadequate life saving interventions.
References
- 1. Olagunju, L. MDG 5: Africa’s progress in improving maternal health. (2013). Carmma.
Crossref - 2. World Health Organization Maternal Mortality Fact Sheet No. 348 May 2012
- 3. World Health Organization. International Classification of Diseases (ICD) 10th revision, Geneva 2004.
- 4. Maternal and Perinatal Death Review Guide. Third edition, Reproductive Health Division, Ministry of Health, Republic of Uganda 2010.
- 5. World Health Organization: Monitoring emergency obstetric care: A Handbook 2009.
- 6. Olenja, J., Gordia, P., Kibaru, J., et al. Influence of provider Training and Quality of emergency obstetric care in Kenya. (2009) Kenya Working Papers No 3.
Crossref - 7. 7. Maternal mortality estimates and MDG 5 attainment by country 1990-2011. (2011) Institute for Health Metrics and Evaluation (IHME).
Crossref - 8. World Health Organization Europe. Maternal and newborn health- Data and Statistics 2014.
Crossref - 9. Hogan, M., Foreman, K., Naghavi, M., et al. Maternal mortality for 181 countries, 1980-2008: A systematic analysis of progress towards Millennium Development Goal 5. (2010) The Lancet 375(9726): 1609-1623.
Crossref - 10. The National Health Strategy for Zimbabwe: Ministry of Health and Child Welfare, Zimbabwe, 2009- 2013.
- 11. United Nations Population Agency (UNFPA). Medicines for maternal health. Prepared for United Nations Commission on commodities for women and children’s health 2012.
Crossref - 12. Park, K. Preventive Medicine in obstetric, Paediatrics and Geriatrics: Park’s Text Book of Preventive and Social Medicine, 20th edition. (2009) Jabalpur M/S Banarasi Das Bhanot 479-483.
- 13. Zimbabwe Demographic Health Survey (ZDHS). Ministry of Health and Child Welfare 2010-2011.
- 14. Kubatana, A. Maternal mortality in Zimbabwe: evidence, costs and implications- UN women- Kubatana (2013).
- 15. Zimbabwe. Census Midlands Provincial Report. (2012) Zimbabwe National Statistics Agency (ZIMSTAT).
Crossref - 16. The World Health Report: make every mother and child count, 2005.
Crossref - 17. Munjanja, S., Nyastrom, L., Nyandoro, M., et al. Maternal and Perinatal Mortality Study. (2007) Ministry of Health and Child Welfare, Zimbabwe.
Crossref - 18. Patton, G.C., Coffey, C., Sawyer, S.M., et al. Global patterns of mortality in young people: a systematic analysis of health data. (2009) Lancet 374(9693): 881-892.
Pubmed || Crossref - 19. Carroli G., Guesta, C., Abalos, E., et al. Epidemiology of postpartum hemorrhage: a systematic review. (2008) Best Pract Res Clin Obstet Gynaecol 22(6): 999-1012.
Pubmed || Crossref - 20. World Health Organisation. Guidelines for the management of post partum hemorrhage and retained placenta.
Crossref - 21. World Health Organisation. Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA and World Bank (2007).
Crossref - 22. Marie, E. Midwifery for nurses. (2010) CBS publishers and distributors.
Crossref - 23. Duley, L. The global impact of pre-eclampsia and eclampsia. (2009) Semin Perinatol 33(3):130-137.
Pubmed || Crossref - 24. World Health Organisation. Recommendations for prevention and treatment of pre-eclampsia and eclampsia. (2011).
Crossref - 25. World Health Organisation. Managing Puerperal Sepsis (2008).
Crossref - 26. orld Health Organization Maternal Mortality Fact Sheet 2012.
- 27. Rao, K., Kashyap, C. Textbook for midwifery and obstetrics for nurses: Elsevier. New Delhi. (2011).
- 28. Yakintepe, S., Silan, F., Hacivelioglu, S., etal. Fetal Vegf Genotype is More Important for Abortion Risk than Mother Genotype. (2014) Int J Mol Cell Med 3(2): 88-94.
Pubmed - 29. World Health Organization. (2014).
Crossref - 30. Ronsmans, C., Graham, W. Maternal mortality: who, when, where, why. (2006) Lancet 368(9542): 1189-1200.
Pubmed || Crossref - 31. Millennium Development Goal Progress Report. (2012) Zimbabwe.
Crossref - 32. Gabrysch, S., Simushi, V., Campell, O. Availability and distribution of and geographic access to emergency obstretric care in Zambia. (2011) Int J Gynecol Obstet 114(2): 174-179.
Pubmed || Crossref - 33. Abotzabire, A. (2008). Factors contributing to maternal mortality: The case of Bawku West District in the Upper East region, Ghana.
Crossref - 34. Bradely, S., McAuliffe, E. Mid-level providers in emergency obstetric and newborn health care: factors affecting their performance and retention within the Malawian health system. (2009) Hum Resour Health 7: 14.
Pubmed || Crossref - 35. Ijadunola, K., Ijadunola, M., Esimai, O., et al. New paradigm old thinking: the case for emergency obstetric care in the prevention of maternal mortality in Nigeria. (2010) BMC Women’s Health 10: 6.
Pubmed || Crossref - 36. Ameh, C., Adegoke, A., Hofman, J., et al. The impact of emergency obstetric care training in Somaliland, Somalia. (2012) Int J Gynaecol Obstet 117(3): 283-287.
Pubmed || Crossref - 37. National Integrated Health Facility Assessment, Ministry of Health and Child Welfare, Zimbabwe 2012.
- 38. Cousens, S., Blencowe, H., Stanton, C., et al. National, Regional and Worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. (2011) Lancet 377 (9774): 1319-1330.
Pubmed || Crossref - 39. Ziraba, A., Mills, S., Madise, N., et al. The state of Emergency obstetric care services in Nairobi informal settlements and environs: Results from maternity health facility survey. BMC Health Serv Res 9: 46.
Pubmed || Crossref - 40. Asamoah, B., Moussa, K., Stafstrom, M., et al. Distribution of causes of maternal mortality among different socio-demographic groups in Ghana: a descriptive study. (2011) BMC Public Health 11:159.
Pubmed || Crossref - 41. Mlambo, C., Chinamo, C., Zingwe, T. An investigation of the causes of maternal mortality in Zimbabwe. (2013) Mediterranean Journal of Social Sciences. 4(14): 615-620.
Crossref - 42. Zimbabwe Ministry of Health and Child Welfare: An analysis of notified institutional maternal deaths January 2010 to December 2011. Government of Zimbabwe.
- 43. Yadav, K., Namadeo, A., Bhargava, M. A retrospective and prospective study of maternal mortality in a rural tertiary care hospital in Central India. (2013) Indian J Comm Health 25(1).
Crossref - 44. Vidyadhar, B., Purushottam, A.G., Ruchika, G. Maternal mortality at a tertiary care teaching hospital of rural India: A retrospective study. (2011) Int J Biol Med Res 2(4): 1043-1046.
Crossref - 45. Girma, M., Yaya, Y., Gebrehanna, E., et al. Lifesaving emergency obstetric services is inadequate in south-west Ethiopia: a formidable challenge to reducing maternal mortality in Ethiopia. (2013) BMC Health Serv Res 13: 459.
Pubmed || Crossref - 46. Abouchadi, S., Alaoui, A., Meski, F., et al. Preventable maternal mortality in Morocco: the role of hospitals. (2013) Trop Med Int Health 18(4): 444-450.
Pubmed || Crossref - 47. Baby, H., Shaha, D. Institutional factors affecting maternal mortality in a teaching hospital. (2010) J Bangladesh Coll phys Sur 28(1): 5-9.
Crossref - 48. Zimbabwe Maternal Mortality Audit report 2010/11. Ministry of Health and Child Welfare, Government of Zimbabwe.
- 49. Echoka, E., Kombe, V., Dubourg, D., et al. Existence and functionality of emergency obstetric care services at district level in Kenya: theoretical coverage versus reality. (2013) BMC Health Serv Res 13: 113.
Pubmed || Crossref - 50. Okoye, M., Adeniji, F., West, C., et al. Status of emergency obstetric care in Local Government Area in South-South Nigeria. (2012) Afr J Reprod Health 16(3): 171-179.
Pubmed || Crossref