Interventions to Increase Colorectal Cancer Screening Among African Americans: A Systematic Review
Techksell M. Washington, Celia Chao, Navkiran K Shokar
Affiliation
Department of Internal Medicine, University of Texas Medical Branch, UTMB, Galveston, TX, USA
Corresponding Author
Maen Masadeh, Department of Internal Medicine, 301 Universities Blvd, JSA 4.160, UTMB, Galveston, TX 77555-0561, Tel: 3199360074; Fax 409.7474-2369; E-mail: maen_masadeh@hotmail.com
Citation
Maen M.M., et al. Interventions to Increase Colorectal Cancer Screening Among African Americans: A Systematic Review. (2014) J Cancer Oncol 1(1): 1-10.
Copy rights
© 2014 Masadeh M. M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License
Keywords
Colon cancer screening; African American; Screening; Colon Cancer
Abstract
Colorectal cancer (CRC) continues to affect African Americans disproportionately. Despite medical advances and widely accepted screening recommendations, African Americans are less likely to get the appropriate screening and consequently are more likely to die from colorectal cancer than their white counterparts. Appropriate communication between the patient and the provider and increased patient education may be a part of the solution to this discouraging problem. Increasing provider education and cultural awareness may increase colorectal cancer screening among African Americans. The objective of this paper to perform a systematic review of the published literature to assess the effectiveness of interventions aimed to increase colorectal cancer screening among African Americans. Seven online databases were systematically searched for article published between Jan. 2000 and April 2013 using subject terms taken from the Medical Subject Headings (MeSH), the list of standardized descriptors used by the National Library of Medicine (NLM), to standardize the search. Studies that measured CRC screening rates and met the inclusion/exclusion criteria were selected. Data was extracted and independently reviewed by three reviewers. Study design, population characteristics, experimental intervention, control intervention and outcomes were extracted from the selected article. Of the 649 studies identified as potentially, eleven articles were selected for the review. Four articles reported using culturally tailored interventions and seven articles did not use culturally tailored interventions. Two studies have intervention aimed at physician education. Eight articles reported statistcally significant results. Because of the limited number of quality studies, no conclusive recommendations can be made regarding the contribution of culturally tailored intervention to increasing CRC screening among African Americans.
Introduction
A ccording to the American Cancer Society (ACS)[1], colorectal cancer (CRC) is the third most common cause of cancer death in both men and women (ACS 2013). Although colorectal cancer death rates have decreased in African American men and women over the past two decades, the decline began later and has been slower among African Americans compared to whites, resulting in a widening racial disparity (ACS 2013). Since 1987, CRC screening rates among African Americans (non-Hispanic) have increased from 4% to 56% in 2013. However, this rate remains lower than screening rate in Whites (non-Hispanic) 62% (ACS 2013). The ACS 2013 CRC screening recommendations for individuals over 50 included the following:
1) Yearly Fecal Occult blood Test (FOBT) or Fecal Immunochemical Test (FIT).
2) Yearly FOBT of FIT plus flexible sigmoidoscopy every 5 years.
3) Flexible sigmoidoscopy every 5 years.
4) Colonoscopy every 10 years.
5) Double-contrast barium enema every 5 years.
Inadequate patient education and poor communication with their health care provider may explain some of the racial differences in the CRC screening rate. The aims of this review are:
1) To identify and describe culturally relevant or non-culturally relevant interventions targeting African Americans that has shown to effectively increase colorectal cancer screening.
2) To identify elements in the provider-patient relationship, such as communication, trust, patient education, and provider recommendations that is associated with increased CRC screening among African Americans. Earlier literature on colorectal cancer attributed the higher colorectal cancer death rates in the African American population to a higher proportion of advanced disease at diagnosis[2]. Despite the fact that screening would diagnose disease at an earlier stage which might lead to a better prognosis, African Americans may be less likely to undergo screening for earlier diagnosis because of decreased access to care[3]. Although white women have a higher cancer incidence rate, black women are more likely to die of cancer (US Cancer Statistics Working Group, 2005). The high cancer mortality in the black population may be related to blacks being diagnosed at later stages[4,5] racial differences[6,7] and lack of definitive treatment[6]. Poverty, racial bias, and stereotyping may play a critical role in the willingness of African Americans to seek screening for colorectal cancer. The provider-patient interaction may be negatively affected by racial discrimination and social disparities resulting in barriers in access to high quality care (ACS, 2013).
When attempting to advise patients regarding CRC screening, it is important that providers understand the cultural norms and beliefs in the population they serve, especially if the patient population is mostly of a different ethnic group[8].
Patient education may also influence an individual to seek CRC screening. Studies have shown that African Americans may be less likely to get CRC screening because of lack of knowledge, understanding or the ability to distinguish a screening test from any other test when compared to whites, even when controlling for education levels[9]. A CRC education and screening program in a diverse low-income, uninsured population located in the state of Maryland's largest county was able to raise the screening rates in the uninsured from 13% to 52% over a two-year period[10]. Provider recommendations for CRC screening have also been shown to increase screening rates in African Americans. In a cohort of 1599 veterans in the Veterans Administration (VA) system, when CRC screening was recommended equally among African American and white non-Hispanic patients (71.0% vs. 68.2%, p = 0.44), the African American patients were 1.3 times more likely than whites to receive CRC screening when recommended (36.3% vs. 28.9%, p = 0.03)[11]. There is a general distrust in the African American community of what might be called "official medicine." This has been called the "Tuskegee phenomenon", a reference that stems from the 40-year study that denied syphilis treatment to a group of African American men from 1932 to 1972, even after there was a known cure[12]. Distrust of physicians often leads African Americans to refuse needed procedures and sometimes to reject care[13]. A study conducted in New Orleans, compared African Americans of lower socioeconomic status to members of the Oschner Health Plan (OHP), who were approximately 80% white, and noted the difference in attitudes and beliefs about cancer and health care. Socioeconomically disadvantaged African Americans agreed 35% of the time, versus 12% of the time (p < 0.001) for the OHP group to the statement, "I sometimes find it difficult to talk to doctors." The African American group agreed 35% versus 26% (p < 0.001) to the statement "I sometimes do not trust what doctors tell me"[14].
Lack of understanding of black culture may lead to distrust and patient resistance to preventive health care such as CRC screening. In efforts to increase CRC screening in African Americans, there have been several studies that address different aspects of the provider-patient relationship, and how it can influence patients' willingness to seek CRC screening. It is important to identify interventions in the provider-patient relationship paradigm that have proven to be effective in increasing CRC screening in African Americans.
Methods
Several online databases were used to identify relevant literature. These included Medline (via PUBMED, Ovid Medline, and the National Library of Medicines Gateway search engine), the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Cochrane Database of Systematic Reviews, Web of Science (including both the Science Social Science Citation and Science Citation Index), and PsycINFO. A search was done for articles published between January 2000 and April 2013 using the Medical Subject Heading (MeSH) database, the U.S. National Library of Medicine's controlled terminology (used for indexing articles for MEDLINE/PubMed). Terms and fragments found in the MeSH database that are relevant to the topic of this treatise were 'professional-patient relationship', 'attitude', 'attitude to health', 'health knowledge', 'practice', 'cultural background', 'customs', 'social psychology', 'beliefs', 'cultural belief', 'communication barriers', 'African American/blacks' and 'colorectal neoplasm'. The MeSH terms allowed a more systematic way to search different databases for articles that use different terminology for the same concepts. Abstracts and articles from the reference lists of the chosen articles were reviewed to identify other articles that may be relevant. The quality of the articles were assessed using a modified version of the U.S. Preventive Services Task Force Hierarchy of Research Design (S. Weller, Personal communication 6/21/08) as shown in table 1.
Table 1: Grades of Evidence for the Professed Quality of a Study Design.*
| Category /Study Design | SCORE |
|---|---|
| A. Randomized controlled trials: in these studies individuals are randomized into study groups. This is the strongest type of study design.(These studies may or may not be double-blinded.) | 1 |
| B. Community trials: in these studies, communities and not individuals are randomized to treatment and control groups. There must be a control group. | 2 |
| C. Pre-post with a single group: In these studies a control group is lacking, and they are considered the weakest | 3 |
*The grades are adapted from of the U.S. Preventive Services Task Force Hierarchy of Research design (S. Weller, personal communication, 6/21/08)
Study selection
The following were the inclusion criteria for the selected studies: (a) studies whose sample population was greater than 50% African Americans, whose interventions addressed specific factors in the patient-provider relationship as it relates to communication, education, or trust (whether or not this was culturally relevant), (b) studies using the ACS-endorsed guidelines for CRC screening, (c) and studies measuring the rate of completed CRC screening by self-report or chart review. Exclusion criteria were studies in which the sample population was less than 50% African Americans and studies that did not stratify results by race. Eleven articles were identified and they are described in details in table 2 (supplemental material).
Main outcomes measures
The primary outcome measure was rates of CRC screening. Other areas of interest were the specific elements of each intervention, including the type of population, type of study, mode of delivery of the intervention(s), use of theory, intervention tailoring, and the identification of elements that were associated with positive outcomes.
Table 2: Colorectal cancer screening in African Americans
| Study Design | Sample Description | Experimental Full Intervention(s) | Control Intervention(s) | Outcome | Design Score |
|---|---|---|---|---|---|
| Powe (2002) Randomized community trial Setting: senior citizen centers Type of control: Tradition Group (Standard Treatment) Intervention(s): Culturally relevant video, calendar, poster, brochure, FOBT Flier Assessments: Baseline and 12 mos. Type: CAI Theory: NR |
Target Population: A A/Black, Elderly N=106 Mean age: 75 A A / Blacks : 100% Whites: 0% Female: 100% |
Videotape: Shown before initial data collection. "Telling the Story…To Live is God's Will" • 20- min. culturally similar person discussion CRC screening. Person also demonstrates how to use the FOBT kit Calendar: "Telling the Story" • Educational calendar that addresses key points about CRC each month using pictures Brochure: "Telling the Story…about Bowel Cancer" • Tri fold brochure expressing the importance of early CRC screening and a picture of FOBT kit and the words "getting checked." Poster: "Can We Talk…About Bowl Caner" • Still pics from the video, picture of a FOBT kit, and signs and symptoms of CRC Flier: "Doing the Kit" • 1 page color flier with FOBT kit. Modified Intervention(s) Group Videotape: "Telling the Story…To Live is God's Will" • 20- min. culturally similar person discussion CRC screening. Person also demonstrates how to use the FOBT kit |
Traditional Group: ACS Videotape: Shown before initial data collection. "Colorectal cancer. The Cancer No One Talks About." • 13 min video on the signs and symptoms of CRC and reasons for FOBT |
Initial Data Collection: Experimental Full Intervention(s) Group 65% participated in FOBT Modified Intervention(s) Group 43% participated in FOBT Control Group 4% participated in FOBT 1 Year Follow-Up Data Collection Experimental Full Intervention(s) Group 63% participated in FOBT Modified Intervention(s) Group 34% participated in FOBT Control Group 7% (n = 5) participated in FOBT (chi-square = 29.37; df = 2; P < .0001) |
2 |
| Powe et al. (2004) Randomized community trial Setting: senior citizen centers Type of control: Tradition Group (standard treatment) Intervention(s): Culturally relevant video, calendar, poster, brochure, FOBT Flier Assessments: Baseline, 6 and 12 mos. Type: CAI Theories: NR |
Target Population: A A/Black, Elderly N=134 Mean age: 73.8 A A / Blacks: 84% Whites: 16% Female: 88% CAI |
Videotape: "Telling the Story…To Live is God's Will" • 20- min. culturally similar person discussion CRC screening. Person also demonstrates how to use the FOBT kit Calendar: "Telling the Story" • Educational calendar that addresses key points about CRC each month using pictures Brochure: "Telling the Story…about Bowel Cancer" • Tri fold brochure expressing the importance of early CRC screening and a picture of FOBT kit and the words "getting checked." Poster: "Can We Talk…About Bowl Cancer." • Still pics from the video and of a FOBT kit Flier: "Doing the Kit" • 1 page color flier with FOBT kit. Modified Intervention(s) Group Videotape: "Telling the Story…To Live is God's Will" • 20- min. culturally similar person discussion CRC screening. Person also demonstrates how to use the FOBT kit |
Traditional Group: ACS Videotape: Shown before initial data collection. "Colorectal cancer. The Cancer No One Talks About." • 13 min video on the signs and symptoms of CRC and reasons for FOBT |
1 Year Follow-Up Data Collection Experimental Full Intervention(s) Group 61% (n = 33) participated in FOBT Modified Intervention(s) Group 46% (n = 15) participated in FOBT Control Group 15% (n=5) participated in FOBT |
2 |
| Campbell et al. (2004) Randomized community trial Setting: rural North Carolina churches Type of control: Educational speakers on non related topics Intervention(s): (WATCH) Wellness for AA Through Churches 1. Tailored print and video, (TPV) 2. Lay health advisor (LHA) 3. Both Assessments: Baseline and 12 mos. Type: CAI Theory: SCT The stage of change transtheoretical framework HBM SSM |
Target Population: A A/Black N=587 Mean age: 52 A A / Blacks : 99% Other: 1% Female: 74% |
TPV Newsletter: • Computer tailored newsletters mailed to participants homes at 2, 4 ,6 and 9th month. • Newsletters were personalized with the participants' name, pastor, and church. • Newsletters contained information on food, screening, spiritual messages and community resources Videotape • 4 videotapes tailored to compliment the newsletters. Community member and pastors were featured on the tapes giving testimonials. • Pastor also delivered a sermon LHA • Indigenous member of the community whom others come to for help. • They were picked by members of the church and then asked to participate in a 16 hr training course over 7 months. • Each of 62 HLV (47 women) were trained to deliver information about eating healthy, exercise and the importance of CRC. They also included some Biblical passages • The HLV was also expected to host church-wide activities to promote the above topics. • Funds where provided for refreshments but the HLV received no monetary incentives. |
Control Churches: • Control churches were offered health education and speakers on subjects not related to study. • Each church could chose from the following topics: HIV/AIDS, adolescent health, child care and health, prostate cancer awareness and elderly health issues. |
Initial Data Collection: (FOBT and other CRC screening test in past year) Control: (30.4% and 20.3%) LHA: (23.5% and 16.6%) TPV: (19.7% and 23.7%) Combined: (19.5% and 26.4%) 1 Year Follow-Up Data Collection Control: (21.7% and 27.5%) LHA: (33.3% and 25.5%) TPV: (36.8% and 21.1%) Combined: (31.0 and 14.9%) No significance difference fo FOBT and of other CRC screening after 1 year (p = .08 and ns) |
2 |
| Basch et al. (2006) Randomized control trail. ) Setting: New York City metropolitan area Type of control: mailed printed materials about CRC screening Intervention(s): Tailored telephone interventions Assessments: Baseline and 6 mos. Type: NCAI Theory:NR |
Target Population: A A/Black N = 456 Mean age: 75 AA/Blacks: 63.2% Whites: 16.2% Other 19.7 Female: 71.1% |
Tailored telephone call: N = 226 • Tailed base on behavior and educational theory (Granz, et al., 2002). • 2 weeks after randomization. • Attempts were made to establish a rapport with the participant while addressing fear, beliefs and misconceptions • Emphasis was placed on positive reinforcement while proving emotional and social support. • Median number of calls 5 per recipient and the median number of minutes was 23.5 min total per recipient |
Mailed printed material: N = 230 Letter: • Mailed I week after randomization • The letter welcomes the person to the program Brochure:"Lets Break the Silence" * • Tri-old brochure that discusses what CRC is and who is at risk. It expresses the importance of early CRC screening and it explains each screening modality. |
Initial Data Collection: At baseline everyone was called. Subjects were excluded from the study if they had had recent CRC screening 6 month Follow-Up Data Collection: Any CRC screening modality. • Control group: 6.1% (14) • Intervention group: 27% (61) • Screening rates 4.4 times higher (95% CI = 2.2, 7.7) in the controls |
1 |
| Khankari et al. (2007) Single arm, pretest-posttest design Setting:Urban federally qualified health center Intervention(s): Mailing letters and brochures, training to improve physician in-pt communication Assessments: Baseline and 1 year. Type: NCAI Theory: NR |
Target Population: Low-income and racial/ethnic minorities N = 154 Mean age: 60.1 y/o AA/Blacks: 51.7% Hispanics: 44.8% Female: 67.8% |
Tracking Patients: • Chart review of pt over 50 who had been to the clinic 3 times between 1-1-02 and 1-28-05 who did not receive CRC screening Letter and Brochure: • Before each visit a physical letter and brochure from the "Screen for Life" campaign developed by the CDC were mailed to the pt. The letter and brochure explained why the pt needed CRC screening. Physician communication training: • 8 physicians went through a l hour educational session which review current CRC screening guidelines and communication skills to reduce medical jargon and improve pt understanding. Feedback loop: • Designed to monitor screening recommendations and completion rates. |
No controls | Initial Data Collection: 11.5% CRC screening 1 Year Follow-Up Data Collection 27.9% CRC screening P = < 0.001 |
3 |
| Katz et al. (2007) Nonrandomized community-based intervention study Setting: Eleven cities in North and South Carolina with subsidized housing. Type of control: Tradition Group (standard treatment) Intervention(s): Culturally relevant brochures, direct mailing, posters, newspaper and local radio ads. Assessments: Baseline and 12 mos. Type: CAI Theory: SLT HBM TTM |
Target Population: Low income women in North and South Carolina N = 2098 Age: 62% > 65 y/o AA/Blacks: 78% Other: 22% Female: 100% |
Mass Media Campaign: Local newspaper ads: Radio announcements Focus groups: • Randomly selected participants from the selected study community were selected to participate in a focus group to evaluate the materials used in the intervention (brochures, poster, etc.) Brochure: details not provided Poster: details not provided. |
Traditional Group: Communities serve as their own control group with baseline measures of CRC screening rates. | Initial Data Collection: 49.3% (95% CI 46.%, 52.6% ) CRC screening rate 1 Year Follow-Up Data Collection 55.6% (95% CI, 47.9%, 63.0%) CRC screening rate |
2 |
| Freidman and Borum (2007) Quasi experimental pretest-posttest design Setting: Internal Medicine clinic Type of control: none Intervention(s): Physician-directed educational intervention Assessments: 6 months pre-test and 6 months post-test. Type: NCAI Theory: NR |
Target Population: A A/Black, N = 116 pre-intervention N= 132 post-intervention Mean age: did not specify A A / B l a c k s : 100% Whites: 0% Female: did not specify |
Didactic Seminars: Lead by attendings • Case-base didactic seminars on surveillance recommendations • Observation of colonoscopies and flexible sigmoidoscopies • 25 question pre and post-test Required charting: • Cancer screening summary forms that where charted in the medical records |
No controls | Initial Data Collection Pre-intervention Rectal Exam n = 48 (41.4%) FOBT n = 46 (33.7%) Endoscopic procedure n = 31 (26.7%)* Initial Data Collection Post-intervention Rectal Exam n = 51 (38.6%) FOBT n = 50 (39.7%) Endoscopic procedure n = 78 (59.1%)* There was no statistical difference in the pre- and post- intervention screening rate using rectal exam (p = 0.6605) or FOBT (p = 0.7748) *There was a significant difference in the pre- and post-intervention screening with an endoscopic procedure (p = 0.0001) |
3 |
| Katz and Fisher (2011) Randomized controlled trial Setting: Federally Qualified Health Center Type of control: Education about CRC screening Intervention(s): Patient activation and barrier counseling Assessments: Two months after intervention Type: NCAI Theory: PMT |
Target Population: Low socioeconomic status N = 270 Median age: 56 y both study group and control AA/Blacks: 72% Female: 64% |
Videotape: Shown before initial data collection. "Ask your doctor about colon cancer screening" • 12- min. video that encouraged the patients to ask their doctors about CRC screening Brochure: • focused on having the patients ask their providers about CRC screening test • PACE communication system (Presenting information, Asking questions, Checking for understanding, Expressing concerns) which Focused on communication training for the patient to ask their healthcare provider about CRC screening 1 month after the medical visit, if CRC screening test ordered and did not complete the test, telephone barriers counseling to address patient identified CRC screening barriers was conducted. If a patient did not have a screening test ordered, telephone barriers counseling focused on activating them to ask for a CRC screening test by calling their provider or asking their provider at their next medical visit. |
Traditional Group: Videotape: • Shown before initial data collection. "Colorectal cancer screening." • the same as shown to the intervention group except the patient activation section was not included in this video Brochure: • Tips to prevent CRC |
Experimental Full Intervention(s) Group 39.1% had CRC screening test ordered and 19.6% had it done Control Group 17.6% had CRC screening test ordered and 9.9% had it done P = 0.001 |
1 |
| Xirasagar et al. (2011) Pre-intervention and post-intervention design Setting: South Carolina Intervention(s): Training African American PCP to perform colonoscopy Assessments: Baseline and 7 years Type: CAI Theory:NR |
Target Population: A A/Black N = 2167 Mean age: 63 AA/Blacks: 92% Female: 76.4% |
Intervention group • Seven African American PCPs were trained to perform colonoscopy. Period of training was 1999-2006. Number of patients in this group was 483 pre-training and 1199 post-training. Comparison group • Five African American PCPs that are not trained to perform colonoscopy. Number of patients in pre-training period was 234 and in post training period was 900 |
No control | Pre-training to post-training CRC screening rates among the study group (9.3% to 48.3% P < .001) Pre-training to post-training CRC screening rates among the comparison group and 9.8% to 29.6% P < .001) Post-training, the trained group CRC screening rate was higher than the comparison group rate (48.3% vs 29.6%; P < .001) Significant increase was observed among African Americans (10.4% pre-training vs 52.8% post-training, P < .0001). |
3 |
| Blumenthal et al. (2010) Randomized community trial Setting: Georgia Type of control: Patients attended an introductory meeting, where they received logo gift bags containing a cookbook, message fan, pamphlets, and CRC screening information, including a National Cancer Institute-developed pamphlet Intervention(s): Same as control and then divided into 3 groups: 1.One on one education 2.Group education 3.Financial support Assessments: 6 months Type: CAI Theory:SET SCT |
Target Population: A A/Black N = 369 Mean age: 67 AA/Blacks:100% Female: 72.9% |
Three groups: • One-on-one education: A health educator met individually with participants in this group for 3 45-minute sessions over 3 weeks to review educational materials on CRC risk and screening. • Group education: a health educator met with participants in groups of 4 to 14 individuals (average, 5 individuals) to review the educational material. Although the material was identical to that covered in the one-on-one counseling, there were more individuals at each meeting, and 4 sessions over 4 weeks were required to cover the material • Financial support: participants were offered financial reimbursement up to $500 for out-of-pocket expenses incurred for CRC screening, including transportation and other nonmedical expenses. A health educator was available to assist with negotiating direct payment and arranging transportation to the physician's office or medical clinic for the screening test. |
• Participants attended the introductory session but received no intervention other than accepting the contents of the gift bag with the educational pamphlets. | Screening rate was 17.7% in control, 22.2% in financial support cohort, 25.4% in one-on-one education cohort and 33.9% in group education cohort. A statistically significant difference was only found in the group education cohort when compared to control (P = 0.039) |
2 |
| Siddiqui et al. (2011) Randomized controlled trail. Setting: Philadelphia Type of control: patients received usual care Intervention(s): Standard intervention (SI) Tailored intervention (TI) Tailored intervention plus reminder (TIP) telephone call Assessments: Twelve months after randomization. Type: NCAI Theory: NR |
Target Population: A A/Black N = 1430 Mean age: not mentioned A A / B l a c k s : 59.5% Whites: 40.5% Female: 66.9% |
Standard intervention: N = 362 • Participants received a mailed standard intervention (i.e., amailed CRC screening invitation letter, informational booklet, a stool blood test [SBT], and reminder letter). The screening invitation letter encouraged recipients to complete any recommended CRC screening test. Tailored intervention: N = 349 • Participants received standard intervention plus 2 tailored message pages. These pages included brief messages addressing personal barriers to screening reflected by responses to Preventive Health Model variables (i.e., perceived salience and coherence, susceptibility, worries and concerns, response efficacy, social support and influence) measured on the baseline survey. Tailored intervention plus a reminder telephone call: N = 358 • Participants were mailed the standard intervention and the tailored message pages. Additionally, they received a reminder telephone call |
N = 361 Participants in control group only received the usual care without any of the three interventions | Initial Data Collection: CRC screening rate: 33% in control, 46% in SI, 44% in TI and 48% in TIP. Screening was significantly higher in the 3 intervention groups compared to the control group (odds ratio [OR] of 1.7 [95% confidence interval (95% CI), 1.3–2.5],OR of 1.6 [95% CI, 1.2–2.1], and OR of 1.9 [95% CI, 1.4–2.6], respectively) |
1 |
CAI= culturally appropriate intervention(s), NCAI= Non-Culturally appropriate intervention(s)
* http://www.cdc.gov/Cancer/colorectal/pdf/CCSilencebrochure.pdf
NR= Not reported, SLT=Social learning theory, HBM= Health belief model, TTM= Transtheoretical Model, SCT= Social cognitive theory, SSM=Social Support model, PMT= Protection Motivation Theory, SET= Social Ecology Theory
Data extracted
Once articles were selected for review, abstraction forms were developed by two reviewers, T. Washington (TW) and N. Shokar (NS) to discuss what data should be extracted. The data was initially extracted by TW and Maen Masadeh (MM) and the completed tables were checked by Celia Chao (CC). These reviewers (TM, MM and CC) assessed the eligibility of the chosen articles based on the exclusion and inclusion criteria described above. Each reviewer independently reviewed the articles and decided on the accuracy of the extracted data. The data that was extracted included the following: study design, setting, detailed descriptions of the intervention(s)/methods, whether the intervention was culturally tailored, number of participants, average age of the participants, percentage of African Americans, percentage of women, number of patients in each arm of the intervention, length of study and follow up, theory used if any, and outcome.
Results
Study Selection
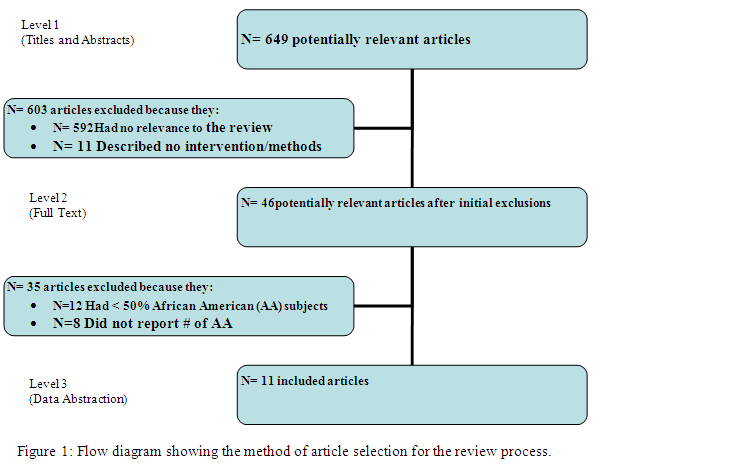
Overall 649 articles were initially identified by titles and abstracts and were screened. Forty six remained after the initial screening and full-text reports of these articles were reviewed by TM and MM and only 11 articles met the inclusion criteria[17-25]. Of the original articles, 603 were excluded because they were not relevant to the review (n = 592) or because the article did not have an intervention or did not describe an intervention in the methods section (n = 11). Thirty five were excluded because of one of more of the following: they reported less than 50% African American participation (n = 12), or they did not stratify their data by race and, therefore, did not report the number of African Americans at all (n = 8), or they did not measure rates of CRC screening at the end of their intervention (n = 15), (See Figure 1).
Study design and selection
Three of the included studies were randomized controlled trials (RCT)[18,22,24], three were randomized community trials[15-17],two studies were a pre- and post-intervention[21,23]. There was a single randomized community interventional trial[25], onesingle-arm, pretest-posttest design[20], and one nonrandomized community-based intervention study[19].The setting for the studies varied: two studies were done in nursing homes[14,16]. Two studies were set in North Carolina, of those, one was done in churches situated in African American communities[17] and one was community-wide[19]. Two studies were in South Carolina[19,23]. Three studies were located in urban areas[18,20,24], and one study was set in a rural area[18]. The others did not specify a rural or urban location. One study was set in an Internal Medicine clinic[21], a specific location for the clinic was not given. One study was done in federally qualified health center that serves low socioeconomic status patients in Ohio[22].
Study population
The study populations ranged from as large as 2167[23] to as small as 106[15]. Ten studies had a majority of female participants (see Table 2 supplemental material), of those, two studies targeted only females[15,19]. The mean ages of the subjects ranged from 52 years[17] to 75 years[18]. Friedman and Borum's 2007 and Blumenthal et al.,2010 studies were done with a population that was 100% African American but gender or average age was not specified in Friedman and Borum et al 2007. Two studies targeted elderly African Americans[15,16], the other studies followed the screening age recommended by the ACS of > 50 years old. Three studies targeted low-income populations[19,20,22] while others did not specify an income target.
Interventions
All but two studies incorporated patient educational materials such as posters, brochures or letters. This was done either in the control group, intervention group, or both. Four studies used videos[15-17,22]. Katz (2007) and his team embarked upon the task of educating entire communities by launching a community-wide, mass media campaign for 12 months using newspaper advertisements, radio announcements, and focus groups to develop culturally tailored brochures and posters. They used social learning theory (SLT), the health belief model (HBM) and the trans-theoretical model (TTM) learning theories in the design of the intervention. For a one year period, Khankari (2007) and his colleagues focused on educating individual patients and improving physician communication skills. Patients were mailed a brochure (Screen for life) and a letter explaining the importance of CRC screening just before their scheduled visit, while the physicians prepared for the visit by attending a one hour educational session to review the CRC screening guidelines and to improve their communication skills. The Friedman and Borum (2007) study was the only one whose intervention was entirely focused on education for the physicians. Using a quasi- experimental before and after study design, they incorporated didactic seminars and case-based learning sessions to educate Internal Medicine residents on appropriate screening recommendations.
Basch (2007) and associates educated their study participants by delivering tailored telephone interventions. During a 12-month period, an average of five phone calls were made to selected members in a New York City community, while simultaneously mailing a brochure (Lets Break the Silence) and a letter to the controls welcoming them to the study. Campbell (2004) and his associates decided to randomize and offer education to different African American churches to implement an intervention termed, "Wellness for African Americans Through Churches (WATCH)", instead of randomizing individual subjects.
Campbell et al. (2004) divided the participating churches into four different groups. For some churches the intervention involved printed newsletters and videos (TPV) every 2nd, 4th, 6th, and 9th months. Some churches were given a lay health advisor, and other churches received both interventions. The control churches were offered health education on a variety of subjects other than CRC screening. The HBM, social cognitive theory (SCT) model and social support model (SSM), plus the stage-of-change, and the trans-theoretical framework were learning theories used by Campbell (2004) and his associates.
Powe (2002, 2004) and her associates used the same 12-month, multi-component, educational intervention in both studies targeted towards educating elderly African Americans in senior citizen centers. The senior citizen centers were randomized into three groups. The first group of centers received a culturally tailored video (Telling the Story…To Live is God's Will) that discussed CRC prevention from a spiritual prospective. A calendar, (Telling the Story), a brochure (Telling the Story…About Bowel Cancer), and a poster (Can We Talk…About Bowel Cancer) and a flyer (Doing the Kit) was also used. Another group of centers received a modified intervention which was just the culturally tailored video (Telling the Story…To Live is God's Will). The control group of centers was shown a non-culturally specific video developed by the ACS (Colorectal cancer. The Cancer No One Talks About). Each component of the intervention used images, language, food, dress, and customs that were familiar to the study population (Table 2 supplemental material).
Katz and Fisher (2012) randomized patients into 2 groups: the control group received CRC screening education and the intervention group received CRC screening education in addition to patient activation and barrier counseling. The intervention group watched a 12-minute video entitled "Ask your doctor about colon cancer screening", received a brochure that supplemented the video and focused on asking their provider for a CRC screening test, and received a second brochure on tips to prevent CRC (e.g., the importance of daily exercise). The patient activation section was not included in the video for the control group participants. One month after the medical visit, if a patient in the intervention group had a CRC screening test ordered but not completed, telephone barriers counseling to address patient identified CRC screening barriers was conducted. If a patient in the intervention group did not have a screening test ordered, telephone barriers counseling focused on activating them to ask for a CRC screening test by calling their provider or asking their provider at their next medical visit. Xirasagar et al (2011) compared colonoscopy rates among established patients of purposively sampled African American PCPs, both trained and untrained in colonoscopy. It was a retrospective observational study based on patient chart review of age-eligible patients of colonoscopy-trained African American PCPs (or those in-training) and patients of untrained PCPs practicing in the same geographic region. This study also compared pre-training and post-training colonoscopy rates among the PCP's patient panel. Siddiqui et al., (2011) randomly assigned participants to 1 of 4 study groups as follows: a control group (received standard care), a standard intervention (SI) group (received a mailed standard intervention i.e., a mailed CRC screening invitation letter, informational booklet, a stool blood test [SBT], and reminder letter), a tailored intervention (TI) group (received the standard intervention plus 2 tailored message pages that included brief messages addressing personal barriers to screening reflected by responses to Preventive Health Model variables measured on the baseline survey) or a tailored intervention plus reminder phone call (TIP) group. Blumenthal et al (2010) objective was to test 3 interventions to increase CRC screening rates among African Americans. Two of the interventions were educational, and the third responded to financial barriers. The educational interventions were consistent with the contention that education could increase screening. Participants were randomized into 4 cohorts: control, one-on-one education, group education and reduce out of pocket expense (participants in financial support group were offered financial reimbursement up to $500 for out-of-pocket expenses incurred for CRC screening). All eleven studies had multiple components to the interventions that were offered to the experimental groups. Six of the studies had baseline data collection, the intervention and then follow-up data collection one year after the baseline[15-17,19-21,23], and one study had baseline data collection, the intervention, and then a six-month follow-up data collection[18]. Four studies required community cooperation to deliver the proposed intervention(s)[15-17,19]. The Campbell group (2007) and Siddiqui et al.,2011 used telephone outreach as the primary intervention, while Katz and his group of researchers were the only ones who used a mass-media campaign to get the message across to their target population. Two studies used specific theories to guide the delivery of their interventions[17,19]. Only Four studies were culturally tailored[15-17,19].
Interventions results
In all of the studies, there appeared to have been an increase in the percentage of CRC screening participation in the intervention groups compared to the control groups. Eight had statistically significant results,[15,18,20-24]. Both studies by Powe and associates (2002, 2004) had many parts to the intervention, and they both seemed to show an increase in CRC from the baseline. However, the p- value was reported only in Powe (2002), and it was significant among the groups (chi-square = 29.37; df = 2;P < .0001). Although CRC screening participation was low after the intervention in the experimental group (27%), Basch (2006) and his colleagues reported that the participants who received the telephone intervention had CRC screening rates that were 4.4 times higher than the controls (95% CI 2.2-7.7) after one year. The Friedman and Borum study (2007) showed a statistically significant difference in pre- and post-intervention CRC screening using the endoscopic procedure (26.7%, n = 31 vs. 59.1%, n = 78; p = 0.0001) but not screening rectal exams (41.4%, n = 48 vs. 38.6%, n = 51; p = 0.6605) or FOBT (33.7%, n = 46 vs. 39.7%, n = 50;p = 0.7748). The Wellness for African Americans Through Churches (WATCH) project reported an apparent increase in CRC screening intervention group; however, it was not statistically significant[17]. Katz (2007) and his team also reported an increase in CRC screening, but there was no statistical difference from baseline (baseline = 49.3% (95% CI 46%, 52.6%) vs. a one year follow-up of 55.6% (95% CI, 47.9%, 63.0%; p = 0.49). Katz and Fisher et al, 2012 reported a statistically significant increase in CRC screening among intervention group (odds ratio 2.35 (1.14–5.56) P = 0.02). In Xirasagar et al., (2011) post-training rates among both the study and comparison groups increased over pre-training rates (9.3% to 48.3% among trained PCPs, P < .001, and 9.8% to 29.6% among comparison patients, P < .001). Post-training, the trained group rate was higher than the comparison group rate (48.3% vs 29.6%; P < .001); the large increase was observed among African Americans (10.4% pre-training vs 52.8% post-training, P < .0001). Siddiqui et al. 2010 also reported significantly higher screening rates in the 3 intervention groups when compared to control. (Odds ratio of 1.7 [95% confidence interval (95% CI), 1.3–2.5] in SI, OR of 1.6 [95% CI, 1.2–2.1] in TI, and OR of 1.9 [95% CI, 1.4–2.6] in TIP, but did not vary significantly across intervention groups.
In Blumenthal et al., 2010 the Group Education intervention resulted in significantly more participants screened (33.9%) compared with the Control cohort (17.7%; P = .039). Although the financial support cohort and the One-on-One cohort rates exceeded that of the control cohort but they did not differ statistically. Of the four culturally tailored interventions[15-17,19] only Powe, 2002 reported a statistically significant increase in CRC screening. In all of the non-culturally tailored interventions statistically significant increases were reported in CRC screening[18,20-25]. It is important to note that three of these studies only used insured participants[18,20,21].
Analysis according to evidence of quality
Basch et al. (2006), Katz and Fisher et al. (2012) and Siddiqui et al. (2011) was the only randomized control trials. These studies had the best design and received a design score of 1 (table 1) since individuals were randomized into study groups and control groups and they were not culturally tailored. Three culturally tailored studies, classified as community trials, used randomized locations instead of individuals[15-17] and one study classified as randomized community trial[24] were assigned a study score of 2. The designs for the other four studies[19-21,23] had the lowest study design score of 3, the weakest category, as they did not have a control group.
Discussion
Some investigators have suggested that increased knowledge and a realistic perception of CRC screening among African Americans could increase CRC screening rates[26-28]. While others suggested that culturally tailored educational interventions may be more successful at increasing the rate of CRC screening in African Americans compared to traditional outreach[29,30]. Although culturally tailored interventions are thought to be successful, there has not been a thorough review of the effectiveness of interventions that aim to increase CRC screening in the African American population. The current treatise is a review of recent studies whose interventional aims were to increase CRC screening in the African Americans. Individual-centered educational interventions (tailored or non-tailored) were found to be more successful than the interventions focused on educating entire communities. This current review suggests that increased provider education and training in communication skills play an important role in elevating CRC screening rates in African Americans, since this resulted in greater increases in CRC screening rates than community-based interventions, but does not eliminate or support the need to continue to develop more culturally tailored interventions to increase CRC screening in African Americans; however it does suggest that educational and communication gaps may be wider than the cultural gap.
Community-wide interventions may play a role in efforts to increase awareness in African American communities; however, awareness may not immediately translate to increased CRC screening participation[31]. The lower success of community intervention trials, compared with individual-centered provider-education interventions could be explained by several different factors. One could be that community-wide interventions may lack the inter-personal communication and interaction needed to properly inform someone about their individual risk and need for CRC screening. Also, the community intervention in the analyzed studies did not always provide an avenue for individuals who were interested in CRC screening but did not have the means. The interventions aimed at increasing physician awareness may have been successful for several reasons. One reason could possibly be that these studies used chart reviews to identify patients who had not been previously screened for CRC but were eligible for screening and had the means to get screened. Secondly, these studies use a pre- and post-test study design, which is an inferior study as compared to randomized community trail study design used in the culturally tailored studies. Most importantly, several other authors have documented the importance of the recommendations by physicians for CRC screening in African American patients[32-34].
A limitation of this current review is that the participants in the selected studies were mostly women. Because of decreased participation of African American men, the benefit of these interventions may be limited to African American females. Another limitation is that the interventions that could be evaluated were heterogeneous and each one had multiple components; a fact that limits any conclusion about what part of the intervention was the most effective, or if one component was not effective at all. Because of the inferior quality and poor methodological quality of some of the studies available for the review, it is difficult to make any definitive assumptions about the effectiveness of recent interventions designed to increase CRC screening in African Americans. More research is needed on the effect of culturally tailored interventions on African American CRC screening. There is also a need for collaborative research involving the community and health care providers. Further research is necessary to identity the role (if any) of standardized education interventions for patient and primary care providers.
References
- 1. American Cancer Society. Cancer Facts & Figures 2013. (2013) Atlanta: America Cancer Society.
- 2. Day, H., Polissar, L., Yang, C.Y., et al. Race, Socioeconomic status, and other prognostic factors of survival from colorectal cancer.(1987) J Chronic Dis. 40(9): 857-864.
- 3. Palmer, C.R., Schneider, C.E. Social disparities across the continuum of colorectal cancer: a systematic review.(2005) Cancer Cause Control.16(1): 55-61.
- 4. Mayberry, R.M., Coates, R.J., Hill, H.A., et al. Determinants of black/white differences in colon cancer survival. (1995) J Natl Cancer Inst. 87(22): 1686-1693.
- 5. Doubeni, C.A., Field, T.S., Buist, D.S.,et al. Racial differences in tumor stage and survival for colorectal cancer in an insured population.(2007) Cancer 109(3): 612-620.
- 6. Du, X.L., Fang, S., Vernon, S.W., et al.Racial disparities and socioeconomic status in association with survival in a large population-based cohort of elderly patients with colon cancer. (2007) Cancer110(3): 660-669.
- 7. Chu, K.C., Miller, B.A., Springfield, S.A. Measures of racial/ethnic health disparities in cancer mortality rates and the influence of socioeconomic status. (2007) J Nat Med Assoc99(10): 1092-1104.
- 8. Agrawal, S., Bhupinderjit, A., Bhutani, M.S., et al. Colorectal cancer in African Americans. (2005) Am J of Gastroenterol100(3): 515-523.
- 9. Shokar, N.K., Vernon, S.W., Weller, S.C. Cancer and colorectal cancer: knowledge, beliefs, and screening preferences of diverse patient populations. (2005) Fam Med 37(5): 341-347.
- 10. Sarfaty,M., and Peng, S. Choice of screening modality in a colorectal cancer education and screening program for the uninsured. (2006)JCancerEduc21(1): 43-49.
- 11. Dolan, N.C., Ferreira, M.R., Fitzgibbon, M.L.,et al. Colorectal Cancer Screening among African-American and White Male Veterans.(2005) Am J Prev Med28(5): 479-482.
- 12. Jones, J.H., Bad Blood: The Tuskegee Syphilis Experiment. (1993) Simon & Schuster Adult Publishing Group.
- 13. Jacobs, E.A., Rolle, I., Ferrans, C.E., et al. Understanding African Americans' views of the trustworthiness of physicians. (2006) J Gen Intern Med 21(6): 642-647.
- 14. Scroggins, T.G.,Bartley, T.K. Enhancing cancer control: Assessing cancer knowledge, attitudes and beliefs in disadvantaged communities. (1999)JLa State MedSoc151(4): 202-208.
- 15. Powe, B.D. Promoting fecal occult blood testing in rural African American women. (2002) Cancer Practice 10(3): 139-146.
- 16. Powe, B.D., Ntekop, E., Barron, M. An intervention study to increase colorectal cancer knowledge and screening among community elders. (2004) Public Health Nurs21(5):432-442.
- 17. Campbell, M.K., James, A., Hudson, M.A., et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. (2004) Health Psychol23(5): 492-502.
- 18. Basch, C.E., Wolf, R.L., Brouse, C.H., et al. Telephone outreach to increase colorectal Cancer Screening in an urban minority population. (2006) Am J Public Health 96(12): 2246-2253.
- 19. Katz, M.L., Tatum, C., Dickinson, S.L., et al. Improvingcolorectal cancer screening by using community volunteers: results of the Carolinas cancer education and screening (CARES) project. (2007) Cancer 110(7): 1602-1609.
- 20. Khankari, K., Eder, M., Osborn, C.Y., et al. Improving colorectal cancer screening among the medically underserved: a pilot study within a federally qualified health center. (2007)JGen Intern Med 22(10): 1410-1414.
- 21. Friedman, M., Borum, M.L. Colorectal cancer screening of African Americans by internal medicine resident physicians can be improved with focused educational efforts. (2007) J Natl Med Assoc99(9): 1010-1012.
- 22. Katz, M.L., Fisher, J.L., Fleming, K., et al.Patient activation increases colorectal cancer screening rates: a randomized trial among low-income minority patients. (2012)Cancer Epidemiol Biomarkers Prev21(1): 45-52.
- 23. Xirasagar, S., Thomas, G.H., Burch, J.B., et al. Colonoscopy screening rates among patients of colonoscopy-trained African American primary care physicians. (2011) Cancer 117(22): 5151–5160.
- 24. Siddiqui,A.A., Randa. S., Hyslop, T., et al. Race and response to colon cancer screening interventions. (2011) Prev Med 52(3-4): 262–264.
- 25. Blumenthal, D.S., Smith, S.A., Majett, C.D., et al. A Trial of 3 interventions to promote colorectal cancer screening in African Americans. (2010) Cancer 116(4): 922–929.
- 26. O'Malley, A.S., Sheppard, V.B., Schwartz, M., et al.The role of trust in use of preventive services among low-income African-American women. (2004) Prev Med 38(6): 777-785.
- 27. Lipkus, I.M., Lyna, P.R., Rimer, B.K. Colorectal cancer risk perceptions and screening intentions in a minority population. (2000) J Nat Med Assoc92(10): 492-500.
- 28. Rawll, S.M., Skinner, C.S., Perkins, S.M., et al. Computer-delivered tailored intervention improves colon cancer screening knowledge and health beliefs of African-Americans. (2012) Health Educ Res 27(5): 868-885.
- 29. Hamlyn, S.M. Reducing the incidence of colorectal cancer in African Americans. (2008) GastroenterolNurs31(1): 39-42.
- 30. Chin, M.H., Walters, A.E., Cook, S.C., et al. Interventions to reduce racial and ethnic disparities in health care. (2007) Med Care Res Rev 64(5): 7S-28S.
- 31. Pinsky, P.F., Ford, M., Gamito, E., et al. Enrollment of racial and ethnic minorities in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. (2008) JNatl MedAssoc100(3): 291-298.
- 32. Palmer, R.C., Midgette, L.A., Dankwa, I. Colorectal cancer screening and African Americans: findings from a qualitative study. (2008) Cancer Cause Control 15(1): 72-79.
- 33. Lasser, K.E.,Ayanian, J.Z., Fletcher, R.H., et al.Barriers to colorectal cancer screening in community health centers: a qualitative study. (2008) BMC FamPract 9: 15.
- 34. Brenes, G.A,.Paskett, E.D. Predictors of stage of adoption for colorectal cancer screening. (2000) Prev Med 31(4): 410-416.