Labial tapping improves oral clinical parameters and the stage of drooling of cerebral palsy children
Cleves Medeiros de Freitas
Affiliation
- 1Caruaruense Association of Higher Education, Caruaru, Pernambuco, Brazil
- 2Southern Cross University, Sao Paulo, Brazil
Corresponding Author
Mariana Ferreira Leite, Pediatric. Dentistry, Southern Cross University, São Paulo, Brazil. Tel: +55 1120375744; E-mail: mariana.leite@cruzeirodosul.edu.br
Citation
Leite, M. F., et al. Labial Tapping Improves Oral Clinical Parameters And The Stage Of Drooling Of Cerebral Palsy Children. (2015) J Dent & Oral Care 1(3): 1- 5
Copy rights
©2015 Leite, M. F. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Cerebral palsy; Drooling; Labial tapping; Saliva
Abstract
Objective: To evaluate oral clinical and salivary parameters following labial tapping using rigid and flexible tapes on cerebral palsy (CP) children.
Study design: Clinical parameters and whole saliva from CP children were collected before and after 30 days using rigid Micropore tape (n = 19) or flexible Kinesio® tape (n = 18). The parameters evaluated were the number of wipes used daily and the clinical stage of drooling, considering frequency and severity. Moreover, the salivary flow rate, pH and buffer capacity (total and in each pH range) were also evaluated.
Results: Micropore or Kinesio® tape reduced the number of wipes used to control saliva escape (55.0% and 40.0%, respectively) and drooling severity and frequency (p ≤ 0.05), without causing any side effect. No clinically relevant salivary changes were associated with the use of either tape. No differences were observed between the parameters measured comparing the two groups treated with distinct tapes.
Conclusion: The labial tapping improves the clinical stage of drooling without influence negatively the salivary secretion and composition in CP individuals.
Introduction
Cerebral palsy (CP) is a disorder characterized by motor impairment caused by a non-progressive lesion in the developing brain. The most common causes of irreversible brain injuries are nervous system infections, hypoxia and head traumas. The type of motion alteration observed in CP is related to the location of the brain injury and the severity of the changes depends on the extent of the lesion. Moreover, CP individuals can present non-motor neurodevelopmental disabilities that compromise performance, communication, perception, sensation, cognition and behavior[1].
The involvement of oral health in CP individuals has been reported in a number of studies[2,3]. Diminished communication ability, higher frequency of sugar intake, limited mouth opening and difficulties in performing proper hygiene are some factors responsible for the higher incidence of dental caries, gingivitis, presence of calculi and periodontal disease in CP individuals[4-6]. Gingival hyperplasia has been reported with frequency in CP due to the use of anticonvulsants, which causes a condition favorable to the development of dental biofilm[7]. Moreover, Class II malocclusion and defects in enamel formation have been observed in CP patients[8].
Children with impaired global motor development show changes in oral motor control that influence mandibular and labial biomechanics, which in turn negatively influence the performance of oral functions, including sucking, chewing, swallowing and controlling saliva escape[9]. One study showed a significantly higher prevalence of drooling in children with poor gross motor function and in those with more severe presentations of CP, including poor head control, difficulty with eating and inability to sustain lip closure[10]. Drooling is a comorbidity of CP associated with diminished quality of life, both for patients and their caregivers[11].
The main therapies for controlling drooling in CP are physiotherapy, intraglandular botulinum toxin application, use of anticholinergic drugs, surgical intervention on salivary gland[12,13]. The use of botulinum toxin and anticholinergic agents presents mild adverse effects, including occurrence of transient dysphagia, dry mouth, diarrhea, neck pain, sialoadenitis, chewing difficulties, short duration, and effects on cognition and salivary secretion[12,13]. While surgical cases present more permanent results, they are more invasive and aggressive methods with side effects such as tonsillar hypertrophy, inflammation or infection in the floor of the mouth, and increased risk of ranula formation and nerve injury[13]. Besides the side effects, there is a lack of long-term studies that evaluate the impact of salivary reduction caused by these therapies on oral biology and on clinical conditions of CP individuals.
Measures that aim to control the drooling through the reduction of salivary flow rate can compromise the oral health of individuals with CP, because saliva contains a number of components with protective properties within the oral cavity, including antimicrobial, antioxidant, immunomodulating, re-mineralizing, and buffer capacity maintenance[14,15]. Studies indicate that individuals with CP present hyposalivation, with changes not only in salivary flow rate, but also in salivary biochemical components, such as amylase and peroxidase, sialic acid, immunoglobulin A, total protein concentrations, osmolality and salivary pH[16-21]. Thus, it is likely that drooling is caused by the deficiencies in oral motor control associated with CP, rather than by excessive saliva production. Therefore, it is recommended that the drooling is controlled by measures that do not accentuate salivary dysfunctions observed in CP patients.
The control of drooling has been studied with the purpose of improving the quality of life of individuals with CP[11]. Intervention, therapeutic and healing measures are designed to alleviate the signs and symptoms in these individuals. This study aimed to investigate the effects of labial repositioning through mechanical contention using two types of adhesive tapes (rigid or elastic medical tapes) on clinical and salivary parameters of CP patients.
Materials and Methods
Subjects
This observational descriptive (demographic data) and analytical (salivary parameters) interventional clinical study was reviewed by the Human Research Ethics Committee, assessed by the Caruaruense Association of Higher Education Institutional Review Board (IRB) and granted approval under protocol 062/10. After being informed of the aims of the investigation, written informed consent for participation and publication was obtained from the adult responsible for each individual who agreed to participate in the study.
A group of 37 non-institutionalized male and female children, aged 6 to 10 years-old, previously diagnosed with CP and attending the Caruaruense Association of Higher Education, were enrolled in this study. The inclusion criterion was a medical diagnosis of CP (10th International Classification of Diseases and Related Health Problems, ICD-10) and the exclusion criteria were severe breathing problems that required positive airway pressure equipment; a history of head and neck radiation and surgical procedures to reduce drooling.
Children selected for the study were randomly divided in two groups. The first group (n = 19) was treated using rigid labial tapping with Micropore medical tape, and the second group (n = 18) was treated using flexible labial tapping with Kinesio® tape.
Clinical Design
The tape was placed under the lower lip and adhered just over the labial commissure on both sides, following the perioral musculature, as showed in the Figures 1a & b. The standard size was 25 mm x 100 mm for Micropore tape (Figure 1a) and 15 mm x 100 mm for Kinesio® tape (Figure 1b). The tapes were used for 3 hours daily over the 30-day treatment period. The caregivers received a manual with written instructions containing specific information concerning the adhesive tape protocol. The caregivers were instructed on the procedures to be followed in case of skin irritation and regarding the manner, place and time of application of the tapes.
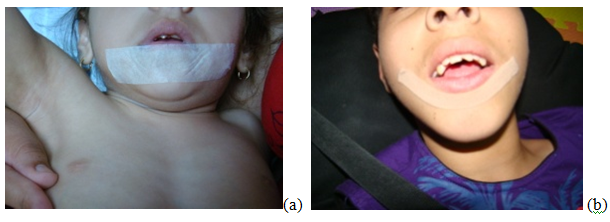
Figure 1: Tapes placed under the lower lip and adhered just over the labial commissure on both sides, following the perioral musculature. (a) Micropore tape, (b) Kinesio® tape.
Parameter Evaluation
Data were collected before and after the experimental period of the study. Patient medical records were reviewed to determine the clinical classification of CP, the level of physical dependence (GMFCS-Gross Motor Function Classification System), and whether the patient was being administered any type of medication.
Through questionnaires completed by caregivers, data were obtained regarding the number of wipes used daily, whether the child was in speech therapy and the occurrence of choking due to the use of the tape. The number of wipes was a parameter evaluated according study published previously[22]. Collaborators were asked to write down how many wipes were used daily and received prior instruction with the aim of standardizing the method. The wipes (cloth diapers) were used until they were completely moistened. Collaborators were asked to dry the lip of patients every time they were wet, avoiding the wetting of clothing.
Clinical stage was assessed by visual clinical examination, considering both the severity and frequency of drooling, using the Thomas-Stonell and Greenberg scale[23]. This scale provides scores for severity (S) ranging from 1 to 5: S1, no drooling; S2, only moist lips; S3, wet lips, chin and throat; S4, damp clothing; and S5, moist wet clothes, hands and objects. Frequency (F) is defined as: F1, no drooling; F2, occasional drooling; F3, frequent drooling; and F4, constant drooling. Thus clinical stage was determined according to the criteria, as follows: grade 1, S1 and F1; grade 2, S2 or S3 and F2; grade 3, S3 and F3; grade 4, S4 or S5 and F3 or F4.
At least 2 h after the previous meal, unstimulated whole saliva was collected using slight suction through a soft plastic catheter between 8 and 10 a.m., to minimize the circadian rhythm effects. Saliva produced in the first 10 s was discarded and the subsequent saliva was collected for exactly 5 min in a graduated cylinder to calculate the initial flow rate (ml/min). During the collection period, all individuals remained comfortably seated in a ventilated and illuminated room. Immediately after saliva collection, both initial pH and buffer capacity were determined using a portable pH meter (Digimed DU-2). The buffer capacity of the whole saliva was determined by titration using 1 ml of saliva and the addition of 0.2 ml of 0.001 N HCl solution. The process of adding acid was repeated and the pH recorded after each addition until pH 5.0. To interpret the results of pH changes, the buffer capacity of whole saliva was analyzed using pH intervals (initial pH-7.0; pH 6.9-6.0; pH 5.9-5.0). For practical purposes, buffer capacity was expressed in the volume (ml) of acid added to 1 ml of saliva, which was considered the equivalent of H+ [17].
Statistical Analysis
The data are presented as mean ± standard deviation (SD). The Anderson-Darling Test was applied to evaluate the frequency distribution of the data. After checking for normality of data distribution, the biochemical parameters and the number of wipes of the groups studied were compared by Analysis of Variance and the Tukey multiple comparisons test. The Chi square test was used to analyze the association between categorical variables, such as demographic data, medication, speech therapy, choking with use of tape, and clinical stage. A logistic regression model was included to verify the influence of medication, speech therapy, and choking with use of tape on salivary parameters. The level of significance adopted was 5% (p < 0.05).
Results
The demographic characteristics of the cerebral palsy children showed no statistically significant differences regarding sex (Chi square test) or age (two-tailed Student t test) comparing the groups using different tapes (Table 1). Among the CP types, 83.8% were spastic and 70.3% were level V GMFCS. The majority of the children was being administered medication (83.7%) and did not choke while following the tape application protocol (86.5%). The use of medications or speech therapy did not influence the parameters studied.
Table 1: Demographic characteristics of the cerebral palsy groups.
| Micropore | Kinesio® tape | Total | ||
|---|---|---|---|---|
| Age | 7.0 ± 3.1 | 8.0 ± 2.5 | ||
| Sex | Female | 36.8% (n = 7) | 55.5% (10) | 45.9% (n = 17) |
| Male | 63.1% (n = 12) | 44.4% (n = 8) | 54.0% (n = 20) | |
| CP type | Spastic | 84.2% (n=16) | 83.33% (n=15) | 83.8% (n=31) |
| Extrapyramidal | 5.3% (n=1) | 11.1% (n=2) | 8.1% (n=3) | |
| Others | 10.5% (n=2) | 5.6% (n=1) | 8.1% (n=3) | |
| GMFCS | I | 15.7%(n=3) | 0.5%(n=1) | 10.8% (n=4) |
| II | 0% (n=0) | 0% (n=0) | 0% (n=0) | |
| III | 0%(n=0) | 0.5 % (n=1) | 2.7% (n=1) | |
| IV | 10.5% (n=2) | 22.2% (n=4) | 16.2% (n=6) | |
| V | 73.6% (n=14) | 66.6% (n=12) | 70.3% (n=26) | |
| Medication | Yes | 89.4% (n=17) | 77.8% (n=14) | 83.7% (n=31) |
| No | 10.5% (n=2) | 22.2% (n=4) | 16.2% (n=6) | |
| Speech therapy | Yes | 63.1% (n=12) | 55.5% (n=10) | 59.5% (n=22) |
| No | 36.8% (n=7) | 44.4% (n=8) | 40.5% (n=15) | |
| Choking with use of tape | Yes | 5.3% (n=1) | 22.22% (n=4) | 13.5% (n=5) |
| No | 94.7% (n=18) | 77.8% (n=14) | 86.5% (n=32) |
GMFCS: Gross Motor Function Classification System
The number of wipes and the distribution of CP individuals according to clinical stage, before (initial) and after (final) the use of Micropore or Kinesio® tape is presented in Table 2. Mechanical labial contention with Micropore or Kinesio® tape reduced the number of wipes used to control drooling by 55.0% and 40.0%, respectively (ANOVA and Tukey test, p ≤0 .05). Before the use of Micropore tape, 21.1% of CP children presented clinical stage 2 and 57.8% stage 4; in contrast, following the use of Micropore tape, 84.2% presented clinical stage 2 and 5.6% stage 4 (Chi square test, p ≤ 0.05). The use of Kinesio® tape showed similar results: before application, 22.2% presented clinical stage 2 and 61.1% stage 4; and after, 61.1% stage 2 and 11.1% stage 4, (Chi square test, p ≤ 0.05).
Table 2: Number of wipes and distribution of CP individuals according to clinical staging before (initial) and after (final) the use of the Micropore and Kinesio® tapes. (*) Statistically significant difference compared with initial time of the respective tape, p ≤ 0.05. (?) Statistically significant difference compared with initial and final time of the respective tape in each clinical staging, p ≤ 0.05
| Groups | Number of wipes | Clinical staging | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Micropore (n=19) | Initial | 5.32 ± 3.63 | 0.0% (n=0) | 21.1% (n=4) | 21.1% (n=4) | 57.8% (n=11) |
| Final | 2.37 ± 2.16* | 5.6% (n=1) | 84.2% (n=16)? | 5.6% (n=1) | 5.6% (n=1) ? | |
| Kinesio® tape (n=18) | Initial | 4.00 ± 3.16 | 0.0 % (n=0) | 22.2% (n=4) | 16.7% (n=3) | 61.1% (n=11) |
| Final | 2.50 ± 2.57* | 5.6% (n=1) | 61.1% (n=11) ? | 22.2% (n=4) | 11.1% (n=2) ? | |
Salivary flow rate, pH, buffer capacity (total and in each pH range, pHi-7.0; 6.9-6.0; 5.9-5.0) of whole saliva from cerebral palsy children before (initial) and after (final) the use of Micropore or Kinesio® tape are presented in Table 3. Patients treated with the Micropore tape presented a reduction in salivary flow rate and pH (ANOVA and Tukey test, p ≤ 0.05%). No differences were observed in the remaining parameters studied following the use of these tapes.
Table 3: Salivary flow rate (mL/mim), pH, buffer capacity - total and in each pH range (pHi-7.0; 6.9-6.0; 5.9-5.0) - (mL HCl 0.01N) of whole saliva from cerebral palsy individuals before (initial) and after (final) the use of the Micropore and Kinesio® tapes. (*) Statistically significant difference compared with initial time of the respective tape, p ≤ 0.05.
| Groups | Salivary flow rate | pH | Total buffer capacity | pHi-7.0 | 6.9- 6.0 | 5.9-5.0 | |
|---|---|---|---|---|---|---|---|
| Micropore (n=19) | Initial | 0.34 ± 0.27 | 7.61 ± 0.64 | 2.93 ± 0.82 | 1.18 ± 0.81 | 1.37± 0.52 | 0.83±0.31 |
| Final | 0.20 ± 0.08* | 7.28 ± 0.75* | 3.37±1.63 | 1.88 ±1.08 | 1.71±0.95 | 0.96±0.65 | |
| Kinesio® tape (n=18) | Initial | 0.28 ± 0.12 | 7.40 ± 0.65 | 3.47 ±1.73 | 1.88 ± 1.49 | 1.47± 0.70 | 0.77±0.34 |
| Final | 0.26 ± 0.21 | 7.14 ± 0.54 | 3.40 ±1.77 | 1.48 ±1.47 | 1.71±1.25 | 0.84±0.28 | |
Discussion
Drooling presented by CP children is associated with physical and psychosocial health impairment and diminished quality of life, both in patients and their care givers[11]. For this reason, the control of drooling is a focus of interest in cases of CP. This study showed that adhesive tapes fixed under the lower lip promoted a reduction in the number of the wipes used to dry saliva and an improvement in both the severity and frequency of drooling. Moreover, labial tapping presented no clinically relevant changes in the salivary parameters involved in maintaining oral health. These results were observed following the use of two types of tapes, rigid (Micropore) and flexible (Kinesio® tape).
The majority of patients in this study presented spasticity, which is in agreement with the literature regarding the clinical classification of CP[24]. In addition to oral motor limitations, CP individuals are frequently administered medications that can cause perioral muscle relaxation and other side effects[25-27], particularly in cases of spasticity. Botulinum toxin application is another method of controlling the saliva escape that is often used for CP patients; however, it can present complications, including edema, involves reapplication every six months and its high cost make it difficult to use on a large scale[28]. For this reason, the benefits of botulinum toxin need to be weighed against the potential for serious adverse events[28]. Removal of the salivary glands is a highly invasive procedure that is also performed to treat drooling in cases of CP[29].
The development of minimally invasive therapies is one of the challenges in the treatment of drooling associated with CP. The application of rigid and flexible tapes has been reported by multidisciplinary professionals for different types of functional deficits to treat a number of motor problems, including CP[22,30-32]. In maxillary orthopedic therapy, elastic labial tapes that mimic the normal function of the orbicularis oris muscle were applied in babies born with complete cleft lip and palate, redirecting the infant's natural growth[32]. The effects of Kinesio® tape application were evaluated on sitting posture, gross motor function and the level of functional independence of children with CP and presented a beneficial assistive treatment approach when combined with physiotherapy[31]. Another study showed that the placement of Kinesio® tape under the mandible, in the chin region, reduced the number of wipes used to contain the saliva escape in children with CP[22].
Studies evaluating the use of medical tapes for reposition of the lips of children with CP for controlling drooling are scarce[22], particularly those that also evaluate oral clinical parameters. The use of labial tapping reduced the number of wipes used to control drooling after 30 days of treatment. Is worth mentioning that the groups varied widely, suggesting that the measure may have had some bias, considering that each collaborator may have understood differently the need or not to change the wipe. Despite the heterogeneity of the group, this data had a relevant, particularly when associated with positive qualitative results in control of drooling after the use of adhesive tapes.
The qualitative evaluation of frequency and severity of drooling presented positive results after the use of adhesive tapes used under the lips of CP child. It was observed a reduced proportion of patients with clinical stage 4 and increased proportion of patients with clinical stage 2. Before treatment, 57.8% of the patients in the Micropore group and 61.1% in the Kinesio® tape group presented clinical stage 4, and following the treatment 84.2% of the patients from the Micropore group and 61.1% from the Kinesio® tape group presented clinical stage 2. Only one patient in each group presented clinical stage 1 after the use of adhesive tape. The clinical stage 1 presents no drooling. The clinical stage 2 presents occasional drooling and only moist lips. The clinical stage 3 presents frequent drooling and wet lips, chin and throat. The clinical stage 4 involves constant saliva escape that wets hands, clothes and objects[23]. The results of this study provide a positive perspective concerning the control of drooling in CP through a noninvasive method.
The majority of children in the study used several anticonvulsant and muscle relaxant drugs: phenobarbital, oxcarbazepine, clonazepam, benzisoxazole, lamotrigine, pericyazine, benzodiazepines, topiramate, diazepam, and ranitidine hydrochloride. Even though these medications compromise labial tonicity, the labial tapping used was efficient in both groups, independent of the use of medications or speech therapy. Movements that involve the act of swallowing are difficult to perform for children with CP due to incomplete lip sealing, low suction pressure, and extended time between the suction and ejection of food[33]. Another positive result is that the use of rigid or elastic tape did not cause choking and permitted partial sealing of the lips in CP.
Comparisons between the two groups that were treated with distinct tapes revealed no differences between the parameters measured. However, it is important to highlight the main differences in the use of different tapes. The rigid Micropore tape should be applied with a minimum dimension of 25 mm in width and 100 mm in length to achieve good adhesion and prevent its removal due to excessive saliva. It has the advantage that it is low cost and easy to apply, independent of the type of malocclusion presented by the individual with CP. Since it is rigid, care must be taken to ensure that the Micropore does not promote excessive force on the lips, allowing the act of swallowing to gradually adapt to the new condition.
The elastic Kinesio® tape also showed positive results on drooling control, with some recommendations. Its elasticity means caregivers need to pay additional attention, particularly in the selection of the tape. Kinesio® tape must be at least 15 mm wide by 100 mm long, and stretch only 10% more than its original size. This pressure is sufficient for the body to feel the presence of an opposing force, providing a tone different from that in the lower lip before application. If higher pressure is applied, this may characterize inappropriate use and worsen the drooling in certain types of malocclusion in that occur in CP (Class II, angle associated with anterior open bite). Use of the elastic tape may show great resistance on the part of caregivers due to the higher price and the restricted number of sales points.
The somatosensory temporal discrimination is a purely sensory process that allows the brain to select relevant sensory inputs for processing information coming from external sources. A study showed that Kinesio Taping-induced reduction of pain in patients with focal dystonia may indirectly contribute to the modulation in sensory discrimination ability[34]. Despite the altered somatosensory brain processing in CP[35], it is expected that proprioception induced by the contact of tape on the lip transmits information to the central nervous system that enables the child with CP not to become get dependent on it over the long term. Despite the positive clinical results, further studies need to be developed in order to elucidate the mechanism of action of the labial tapping in cerebral palsy Individuals.
Cerebral palsy patients present several salivary alterations that can be involved with poor oral health, such as a reduction in salivary flow rate[16-21]. A rigid or flexible mechanical labial contention can help increase the quality of life of individuals with CP and their caregivers by reducing the amount of daily wipes needed to contain the uncontrolled escape of saliva and improve the clinical stage of drooling in children with CP. This was achieved by a simple labial reposition and without adopting measures that reduce the salivary flow rate and other salivary parameters related to oral health, such as pH and buffer capacity.
Conclusion
In conclusion, this study showed that the labial tapping improves the drooling severity and frequency in CP without impairing parameters related to oral health. Whereas the study showed a reduction of the number of wipes used to control saliva escape, further studies need to be developed in relation to quality of life of CP children after the labial tapping. Furthermore, the study contributes to the formation of knowledge for the development of research and therapies using noninvasive methods in controlling drooling in cerebral palsy.
Conflicts of Interest: The authors report no conflicts of interest and alone are responsible for the content and writing of the paper.
References
- 1. Rosenbaum, P., Paneth, N., Leviton, A., et al. A report: the definition and classification of cerebral palsy April 2006. (2007) Dev Med Child Neurolsuppl 109: 8- 14.
- 2. Guaré, R.O., Ciamponi, A.L. Dental caries prevalence in the primary dentition of cerebral-palsied children. (2003) J Clin Pediatr Dent 27(3): 287- 292.
- 3. Dos Santos, M.T., Nogueira, M. L. Infantile reflexes and their effects on dental caries and oral hygiene in cerebral palsy individuals. (2005) J Oral Rehabil 32(12): 880- 885.
- 4. Chu, C. H., Lo, E. C. Oral health status of Chinese teenagers with cerebral palsy. (2010) Community Dent Health 27(4): 222- 226.
- 5. Ferreira de Camargo, M. A., Frias, A. C., Antunes, J. L. The incidence of dental caries in children and adolescents who have cerebral palsy and are participating in a dental program in Brazil. (2011) Spec Care Dentist 31(6): 210- 215.
- 6. Abanto, J., Carvalho, T. S., Bönecker, M., et al. Parental reports of the oral health-related quality of life of children with cerebral palsy. (2012) BMC Oral Health 12- 15.
- 7. De Oliveira Guare, R., Costa, S. C., Baeder, F., et al. Drug-induced gingival enlargement: biofilm control and surgical therapy with gallium-aluminum-arsenide (GaAlAs) diode laser-A 2-year follow-up. (2010) Spec Care Dentist 30(2): 46- 52.
- 8. De Carvalho, R. B., Mendes, R. F., Prado RR, Jr., et al. Oral health and oral motor function in children with cerebral palsy. (2011) Spec Care Dentist 31(2): 58- 62.
- 9. Erasmus, C. E., Van Hulst, K., Rotteveel, L. J., et al. Drooling in cerebral palsy: hypersalivation or dysfunctional oral motor control? (2009) Dev Med Child Neurol 51(6): 454- 459.
- 10. Reid, S. M., Walstab, J. E., Chong, D., et al. Secondary effects of botulinum toxin injections into salivary glands for the management of pediatric drooling. (2013) J Craniofac Surg 24(1): 28- 33.
- 11. Chang, S. C., Lin, C. K., Tung, L. C., et al. The association of drooling and health-related quality of life in children with cerebral palsy. (2012) Neuropsychiatr Dis Treat 8: 599- 604.
- 12. Lakraj, A. A., Moghimi, N.,Jabbari, B.Sialorrhea: Anatomy, pathophysiology and treatment with emphasis on the role of botulinum toxins. (2013) Toxins(Basel) 5(5): 1010- 1031.
- 13. Khadivi, E., Ashraf Zadeh, F., Bakhshaee, M., et al. Bilateral submandibular duct rerouting: Assessment of results on drooling in cerebral palsy cases. (2013) Auris Nasus Larynx 40(5): 487– 490.
- 14. De Almeida Pdel, V., Grégio, A. M., Machado, M. A., et al.Saliva composition and functions: a comprehensivereview. (2008) J Contemp Dent Pract 9(3): 72- 80.
- 15. Fábián, T. K., Hermann, P., Beck, A., et al. Salivary defense proteins: their network and role in innate and acquired oral immunity. (2012) Int J MolSci 13(4): 4295- 4320.
- 16. Santos, M. T., Guaré, R. O., Leite, M. F., et al.Salivary osmolality in individuals with cerebral palsy. (2010) Arch Oral Biol 55(11): 855- 860.
- 17. Santos, M. T., Guaré, R., Leite, M., et al.Does the neuromotor abnormality type affect the salivary parameters in individuals with cerebral palsy? (2010) J Oral Pathol Med 39(10): 770- 774.
- 18. Santos, M. T., Ferreira, M. C., Leite, M. F., et al. Salivary parameters in Brazilian individuals with cerebral palsy who drool. (2011) Child Care Health Dev 37(3): 404- 409.
- 19. Santos, M. T., Batista, R., Guaré, R. O.,et al. Salivary osmolality and hydration status in children with cerebral palsy. (2011) J Oral Pathol Med 40(7): 582- 586.
- 20. Guaré, R. O., Ferreira, M. C., Leite, M. F., et al. Dental erosion and salivary flow rate in cerebral palsy individuals with gastroesophageal reflux. (2012) J Oral Pathol Med 41(5): 367- 371.
- 21. Leite, M. F., Aznar, L. C., Ferreira, M. C., et al.Increased salivary immunoglobulin A and reduced α-amylase activity in wholesaliva from spastic cerebral palsy individuals. (2013) J Oral Pathol Med 42(6): 480- 485.
- 22. Ribeiro, M. O. The use of the Kinesio taping method in the control of sialorrhea in children with cerebral palsy. (2009) Acta Fisiatrica 16: 168- 172.
- 23. Thomas-Stonell, N., Greenberg, J. Three treatment approaches and clinical factors in the reduction of drooling. (1988) Dysphagia 3(2): 73- 78.
- 24. Bax, M., Goldstein, M., Rosenbaum, P., et al. Proposed definition and classification of cerebral palsy, April 2005. (2005) Dev Med Child Neurol 47(8): 571- 576.
- 25. Depositario-Cabacar, D. F., Zelleke, T. G.Treatment of epilepsy in children with developmental disabilities. (2010) Dev Disabil Res Rev 16(3): 239- 247.
- 26. Mato Montero, A.,Limeres Posse, J., Tomás Carmona, I., et al. Control of drooling using transdermal scopolamine skin patches: A case report. (2008) Med Oral Patol Oral Cir Bucal 13(1): E27- E30.
- 27. Eiland, L. S.Glycopyrrolate for chronic drooling in children. (2012) Clin Ther 34(4): 735- 742.
- 28. Rodwell, K., Edwards, P., Ware, R. S., et al. Salivary gland botulinum toxin injections for drooling in children with cerebral palsy and neurodevelopmental disability: a systematic review. (2012) Dev Med Child Neurol 54(11): 977- 987.
- 29. Reed, J., Mans, C. K., Brietzke, S. E. Surgical management of drooling: a meta-analysis. (2009) Arch Otolaryngol Head Neck Surg 135(9): 924- 931.
- 30. ?im?ek, T. T., Türkücüo?lu, B., Çokal, N., et al.The effects of Kinesio® taping on sitting posture, functional independence and gross motor function in children with cerebral palsy. (2011) Disabil Rehabil 33(21- 22): 2058- 2063.
- 31. Mostafavifar, M., Wertz, J., Borchers, J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. (2012) Phys Sportsmed 40(4): 33- 40.
- 32. Choo, H., Maguire, M., Low, D.W. Modified technique of presurgical infant maxillary orthopedics for complete unilateral cleft lip and palate. (2012) Plast Reconstr Surg 129(1): 249- 252.
- 33. Lespargot, A., Langevin, M. F., Muller,S., et al.Swallowing disturbances associated with drooling in cerebral palsied children.(1993) Dev Med Child Neurol 35(4): 298- 304.
- 34. Pelosin, E.,Avanzino, L.,Marchese, R., et al. Kinesiotapingreduces pain and modulates sensory function in patients with focal dystonia: a randomized crossover pilot study. (2013) Neurorehabil Neural Repair 27(8): 722- 731.
- 35. Riquelme, I., Montoya, P. Developmental changes in somatosensory processing in cerebral palsy and healthy individuals. (2010) Clin Neurophysiol 121(8): 1314- 1320.












