Leprosy, Two Cases of the Tuberculoid Form in Venezuela, and A Short Review
Lapenta, J M
Affiliation
1) Dr. Lapenta, J Medic Surgeon, Specialty Dermatology, 24 years of exercise. Highly trained in the field of Leprology; University of Carabobo, Venezuela. CEO DERMAGIC EXPRESS.
2) Dr. Lapenta, JM. Medic Surgeon. University of Carabobo. Diplomat in Facial Aesthetics Occupational Medicine and Prehospital Auxiliary. Resident Doctor Ambulatorio del Norte Maracay Aragua State. COO DERMAGIC EXPRESS.
Corresponding Author
Jose Lapenta, University of Carabobo, J Medic Surgeon, Specialty Dermatology, 24 years of exercise. Highly trained in the field of Leprology, CEO Dermagic express, Venezuela, Email: dermagicexpress@gmail.com
Citation
Lapenta, J., et al. Leprosy, Two Cases of the Tuberculoid Form in Venezuela, and A Short Review. (2018) Invest Demerol and Venereol Res 4(1): 22- 29.
Copy rights
© 2018 Lapenta, J. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License
Keywords
Hansen’s disease; Leprosy; Tuberculoid leprosy; Paucibacillary leprosy; Mycobacterium leprae; Borderline leprosy
Abstract
Leprosy is an ancestral disease mentioned in the Holy Bible in the Chapter of Leviticus, discovered its causal agent by the German Armauer Hansen in the year 1.873 being the Mycobacterium Leprae bacterium, which even with the great therapeutic advances in the last Century still persists in our world. From this disease classically (5) variants have been described, according to the immunity of the patient, defined by the World Health Organization: In 1.) Indeterminate, (Initial phase- (LI)), Tuberculoid (TT or paucibacillary), 2.) Borderline (BB), with two variants: 3.) Borderline Tuberculoid (BT, paucibacillary) and 4.) Borderline Lepromatous (BL, multibacillary), 5.) Lepromatous or diffuse (LL) (Multibacillary). Tuberculoid or Paucibacillary leprosy has a great characteristic has the great characteristic of being lesions that can occur in any part of the body even face, but more frequent in the limbs, often unique that usually affect the limbs, erythematous with a defined border, central atrophy, with loss of sensitivity, (anesthesia), the Mitsuda test is highly positive, 2 or 3 ++ Ulnar nerves, external sciatic-popliteal and branches of the superficial cervical plexus are infiltrated. The investigation of acid-fast bacilli in the lymph of the ears and in the nasal mucus is usually negative. The skin biopsy shows atrophy of the epidermal stratum with rectification of the dermal epidermal junction, and inflammatory infiltrate around the nervous fillets, and absence of epidermal appendages mainly hair follicles. The Mycobacterium Leprae may or may not be present in the biopsy in the Tuberculoid (TT) spectrum, and is usually present in the Tuberculoid Borderline (BT) spectrum.We describe two cases of Tuberculoid Leprosy, one of them borderline variant.
Introduction
Main objective
Describe two (2) cases of tuberculoid leprosy in the Republic of Venezuela, years 2017 and 2018 with more than 8 and 10 years of evolution respectively, with the main purpose of demonstrating that this ancestral disease persists even in the modern world.
Secondary objectives
• Teach and educate the population in general and students of medicine and dermatology, the characteristics of this disease, means of contagion, classification and diagnostic methods.
• Demonstrate scientifically that this stigmatizing disease even having decreased its incidence in many countries, still exists, and is a reality which we can see into in our hospitals and private practices. Due to the global travel and migrations, M. leprae can be a world-wide problem.
• Make a public recognition in the dermatological medical field to Dr. Pedro Lapenta, Dermatologist, and Leprólogist, who was director of the two Leprosariums of Venezuela, Providencia Island and Cape white for almost 20 years. He was also one of the discoverers of the underlying pathology of Diffuse Anergic Cutaneous Leishmaniasis.
Clinical case no.1: We present a 31-year-old female from San Juan de Los Morros, in the State of Guárico. She is a housewife who was referred to the Skin Disease Clinic in 2018.
Reason for consultation: Skin rash, with numbness and cramping on the right leg and foot that has slowly and progressively spread over an 8 year period.
Clinical Description: The patient presents with a large well-defined plaque with somewhat scaly and granular erythematous edges and smooth atrophic center. The lesion was non-painful nor pruritic. The center was anhidrotic, light brown in color with absence of hair follicles with loss of sensation to pain and deep touch. The plaque was located from the lower 1/3 of the right leg to the heel, covering part of the foot. The lesion was localized and did not present on any other location on the patient.
Tuberculoid leprosy (TT) located in the right leg and foot, left side.
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 1
Tuberculoid leprosy (TT) located in the right leg and foot, right side.
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 2
Complementary tests for the Diagnosis
Sensitivity tests were performed: cold-heat, (temperature), thick touch with cotton (protopathic) and fine touch with the tip of a needle (epicrithic), all of which were positive (the patient could not discern between cold and hot in the skin lesion, neither the tip of the needle nor the touch with cotton).
On physical exam, thickening of the hemi-lateral popliteal nerve of the affected limb was palpated.
The patient was referred for skin biopsy, lymph node study, nasal secretion and intradermal reaction (Mitsuda test) to confirm or rule out the presumptive diagnosis of tuberculoid leprosy. A biopsy was taken of the central area of the lesion and the edge.
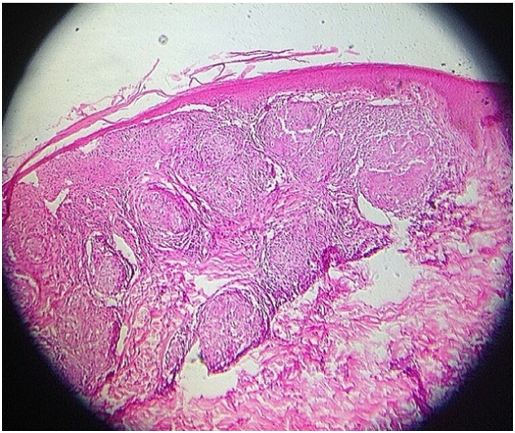
Biopsy of the central area towards the edge of the lesion: rectification of the dermal epidermal junction, thinning of the epidermis, absence of skin appendices, mainly hair follicles and the formation of granulomas, with inflammatory infiltrate. Hematoxylin Eosin stain
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 23
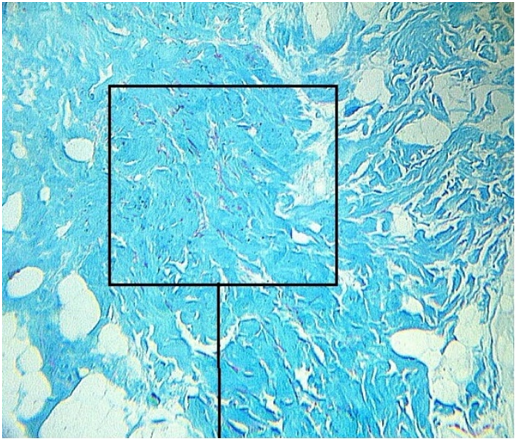
Faraco Fite coloration: Shows infiltration of elongated red acid-fast bacilli in the deep dermis area, which are framed in the central box. This confirmed the presence of Mycobacterium leprae.
Source: Office for skin diseases. Dr. José Lapenta.
Figure No. 4
Diagnostic Criteria
Clinical: Cutaneous lesion on the lower limb with anesthesia, atrophy, anhydrosis and functional disability. Thickening of the right popliteal nerve.
Tests of sensitivity: To cold, heat, and to the epicritic (fine) and protopathic (thick) touch: positive, (inability to discern between cold and heat and to the touch with a needle and cotton swab).
Lymph (auricular pavilions) and nasal secretion: Absence of acid-fast alcohol bacilli.
Mitsuda Test: +++ (right forearm intradermal reaction). Strongly positive
Biopsy (Hematoxylin Eosin and Faraco Fite stain): Histopathological changes with a diagnosis of tuberculoid leprosy (TT)
Clinical case no. 2
A 25 year old male patient from Palo Negro, State of Aragua, presented to our office in 2017.
Reason for consultation: Numbness and decreased mobility of the right hand with a skin rash that has slowly expanded over a 10 year period.
Clinical description: The patient presents with skin lesions located on the right hand and forearm characterized by being a single plaque with raised erythematous edges, with a verrucous quality and central smoothness, hypopigmented patches, and loss of hair follicles (forearm) on hand and forearm. The lesions are only present on forearm and right hand, and absent elsewhere.
Borderline Tuberculoid Leprosy (BT) located in the right hand and forearm.
Source: Office for skin diseases. Dr. José Lapenta,
Figure No. 5
Borderline Tuberculoid Leprosy (BT) located on the right forearm.
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 6
Complementary tests for the diagnosis
Sensitivity tests were performed: Cold-heat, (temperature), to the thick tact with cotton (protopathic) and to the fine tact with the tip of a needle (epicritic), being all positive (the patient could not discern between cold and heat and identify the tip of the needle in the lesion, or the tact with cotton).
The thickening of the hemilateral ulnar nerve of the affected limb was found by palpation. The patient was referred to the Civil Hospital of Maracay State Aragua with the presumptive diagnosis of tuberculoid leprosy. There a biopsy was taken of skin and lymph node; nasal secretion, and Mitsuda test were performed.
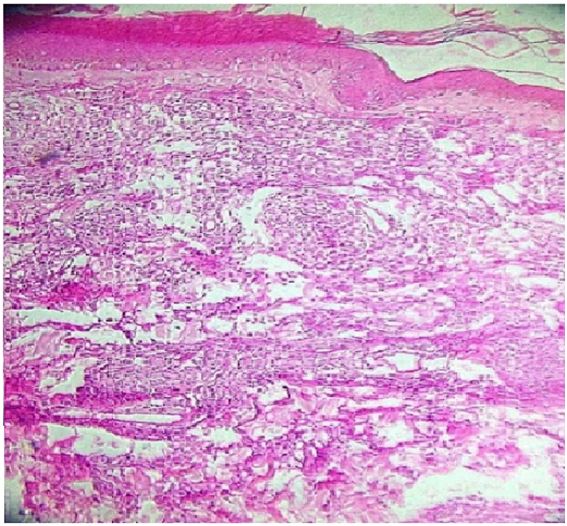
Biopsy taken in the central area of one of the lesions: thinning of the epidermis is observed, rectification of the dermal epidermal junction, absence of adnexa (hair follicles, absence of cells in the upper and middle dermis, inflammatory infiltrate around blood vessels and nervous fillets, and in some areas tendency to form granulomas. It is noted greater disorganization of the epidermal dermo layer and greater inflammatory infiltrate. Hematoxylin Eosin Stain.
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 7
Faraco fite stain: presence of elongated reddish rods around the skin adnexa and in the deep dermis, which correspond to acid-fast bacilli, this confirmed the presence of Mycobacterium leprae and the diagnosis of tuberculoid leprosy.
Source: Office for skin diseases. Dr. José Lapenta
Figure No. 8
Diagnostic Criteria
Clinical: Several cutaneous plaques with raised borders, central hair loss and decreased sensitivity, discoloration, atrophy that extended from the right forearm to the hand, causing functional disability. Thickening of the right ulnar nerve by palpation. The remainder of the skin exam was normal.
Tests of sensitivity to cold, heat, and to the epicrithic (fine) and protopathic (thick) tact: positive, (inability to discern between cold and heat and to tact (touch) with a needle and cotton swab).
Lymph (auricular pavilions) and nasal secretion: presence of acid-fast bacilli.
Mitsuda: Weakly positive (right forearm intradermal reaction).
Biopsy (Hematoxylin Eosin and Faraco Fite): Histopathological changes in accord with the diagnosis of Tuberculoid Leprosy variant borderline (BT).
Discussion
Leprosy is a biblical ailment described in Leviticus 13: verse 3 and 12, which read as follows:
“And the priest will look at the infection on the skin of the body, and if the hair on the infection has turned white, and the infection seems deeper than the skin of his body, it is a leprosy infection, when the priest has examined it. He will declare it impure.”
“... And if the leprosy sprouts and spreads on the skin, and the leprosy covers all the skin of the one who had the infection, from his head to his feet, as far as the priest can see ...” [1]
But if we examine the history of Indians of the sub-continent, where the first cases of Leprosy were described, and first skeletal findings of the disease discovered, dating to 2,000 years BC[2-4].
But it was not until the year 1873 in Norway, when the German scientist Armauer Hansen, discovered the causal agent of this disease, the bacterium Mycobacterium Leprae. The disease took on his name, Hansen’s disease[5]. Due to the spread of this disease in practically all of the world, the governments of that time created the so-called “Leprocomium”, “Leproserías” or “Lazarettos” (by Lázaro the patient of Leprosy who healed Jesus Christ). That Leproseries were eliminated in the early 70’s when appeared highly effective medicines against Leprosy[1-6].
Two-hundred and five years passed, and another species of Hansen’s disease- causing Mycobacterium was discovered in the year 2008, Mycobacterium Lepromatosis[7].
Currently, India has highest rate of leprosy (60 %) followed by Brazil (19%) and Indonesia (9%)[5]. The most important leprosarium in Venezuela were two (2): one located in the State of Zulia called Providencia Island[8] and the main one located in the Vargas State called Leprocomium of Cape White[9], in both Dr. Pedro Lapenta was Director for 15 to 20 years, working together with Dr. Convit and other colleagues and publish fourteen (14) papers on the subject[10-23].
Clinical Manifestations and Classification of Leprosy
Leprosy presents as hypopigmented macules, well-defined plaques with erythematous borders, subcutaneous nodules, thickening of the ulnar nerves, peroneal and superficial plexus, leonine facies, loss of the tail of the eyebrows, enlargement of the lobes in the ears, functional incapacity for the march and movement of the hands, and in some cases there may be ulcerative reactions: Ulcerated reactive Tuberculoid Leprosy[23], and Lucio’s Phenomenon, or diffuse leprosy of Lucio and Latapi. This ulcerative type lesion occurs in diffuse non-nodular lepromatous leprosy, first described by Rafael Lucio Najera in 1852, also called Necrotizing Erythema, identified by José Fernando Latapi and Zamora in 1948[24].
In 1953, at the Madrid Congress on Leprosy, two major clinical manifestations were adopted for leprosy: Severe or lepromatous leprosy (LL-multibacillary) and resistant or Tuberculoid (TT-paucibacillary). In 1966, this scheme of two manifestations (TT) and (LL) was maintained, later a third intermediate manifestation was added, which was called “dimorph”, having characteristics of both. In 1966, Ridley and Jopling proposed a new classification that was related to the research of Kensuke Mitsuda[30-32].
In 1923, Kensuke Mitsuda discovered the Lepromin test, an intradermal delayed hypersensitivity reaction to sterile, dead leprosy bacilli. The test could differentiate between infected and non-infected persons. The test was called the Lepromin Test[30-32].
In 1962, Ridley and Jopling introduced a classification of leprosy based on the immunity of patients, and categorized it into 5 types. This was adopted by the World Health Organization (WHO)[33]. Type 1. Undetermined, (Initial phase- (LI), Tuberculoid (TT or paucibacillary), Type 2. Borderline or Borderline (BB), with two variants: Type 3. Borderline Tuberculoid (BT, paucibacillary) and Type 4. Borderline Lepromatous (BL, multibacillary), Type 5. Lepromatous or diffuse (LL, Multibacillary). In general 2 large groups: Paucibacillary (few or moderate amount of bacilli) and Multibacillary (numerous number of bacilli)[33,34].
Diagnosis
The diagnostic criteria to identify a case of leprosy positively are
Clinical: hypopigmented macules, well-defined plaques with well-defined borders and absence of skin adnexa, hair follicles (alopecia), sweat glands (anhidrosis), central atrophy, subcutaneous nodules, in some cases ulcerations, leonine facies, enlarged ear lobes, thickening of peripheral nerves, mainly ulnar and popliteal. Fundamental characteristic of the lesions: anesthesia[33-35].
Sensitivity test: loss of sensitivity to fine and thick touch (tact): it uses a syringe with a needle (fine touch), and a cotton swab (thick touch). Loss of sensitivity to the temperature in the area of lesions, which is done with 2 test tubes (one with hot water, another with ice or cold water). The failure of sensitivity in Leprosy is called “toponaesthesia”, a word that comes from the Latin, topo, place and anesthesia, without sensitivity. Topoaesthesia is due to the fact that the main “target” of Mycobaterium Leprae is the Schwann cell, the main component of the nervous system[33-35].
Lymph and nasal secretion: sample of lymph taken from ear lobes and mucus or nasal discharge with a swab, which is stained with Giemsa staining: the bacterial forms of isolated or grouped Mycobacterium Leprae called “Globis” appear.”[33-35]
Lepromine test and fernandez reaction: as explained above, 0.5 - 1ml of a sterile solution containing dead Mycobacterium Leprae bacilli is injected into the forearm and read at 48 hours based on the erythematous halo (10 millimeters or more of induration at the injection site is a positive Fernandez test).[33-35]
The Mitsuda or Lepromin test is read at 21 days after the test is placed, and is measured by the appearance of indurated papules at the site of the injection. Based on these two aspects, Ridley and Jopling, together with the results of the Biopsy classify leprosy:
Ridley and Jopling classification in 1962.
| LEPROSY TYPE | TEST OF LEPROMINE | MYCOBACTERIAS IN LYMPH OR NOSE SECRETION |
|---|---|---|
| TT=Tuberculoid | 2 or 3 + | Absence of mycobacterias |
| BT = Borderline Tuberculoid | 1 or – (negative) | 0 – 2 + |
| BB= Borderline Borderline | - (negative) | 2 – 5 + |
| BL=Borderline lepromatous | - (negative) | 4 – 5 + |
| LL=Lepromatous | - (negative) | 5 – 6 + |
| LI=Undetermined | Negative, occasional 1+ | (negative), occasional 1 + |
Source: Int j Lepr Other Mycobact Dis. 1966 Jul-Sept; 34(3): 255-73
Histamine test: a drop of histamine is placed on the outskirts of the leprosy lesion in healthy skin, it is scarified with a needle and the reaction is expected, which in this case is immediate: an erythema appears around the scarification but this one “stops” when reaching the lesion of leprosy because the nerve fillets, the main “target” of the Mycobacterium leprae, are damaged. Histamine is a neurotransmitter; if the nerves are damaged the skin reaction stops before reaching the lesion.[33-35]
Skin biopsy: skin biopsy is done of the central area and / or edge of the lesions. Based on histopathological findings, the definitive diagnosis is made. A constant is the thinning of the epidermis, the rectification of the dermal epidermal junction, the formation of granulomas, the absence of epidermal appendages such as sebaceous glands, hair follicles and sweat glands, epithelioid and foam cells and undoubtedly the presence of the bacterium Mycobacterium leprae, which may be absent or scantly present in the Indeterminate and Tuberculoid Leprosy.
Special stains: Hematoxylin - Eosin, Giemsa; Ziehl Neelsen, Grocott, Faraco Fite and methylene blue.[17,19]
Contagium mode: The mechanism of fundamental contagion of Leprosy is nasal drops that disseminate in the air and penetrate the body of nearby individuals. The incubation period can last between 5 and 20 years, with a minimum of 6 months to 2 years. It was always considered a transmission disease clearly from human to human, but in 2011, a study demonstrated human infection of Mycobacterium leprae by nine-banded armadillo (Dasypus novemcinctus)[36]; a chimpanzee in Sierra Leone; 2 Mangabey monkeys in Nigeria[37]; and red squirrels of the British Isles and Scotland[38-40]. There are no reported transplacental transmission or blood transfusion cases[36-43].
Treatment
The first known treatment for leprosy was introduced by the Egyptian Tortoulis Bey in 1894,[48] called Chaulmoogra Oil, and it was not until the discovery of the Sulfones in the 40s and later antibiotics, which made the World Health Organization, decree the closure of Leproseries in all the World[40-42].
It is interesting to remember that the first drug effectively synthesized against leprosy, was the DDS (DAPSONE) with the commercial name of PROMIN, chemical component SODIUM GLUCOSULPHONE (laboratory Parke Davis) in the year 1940[43-45]. The commercial presentation of the medicine PROMIN was as a solution in bottles for intravenous injection.
The effectiveness of PROMIN against leprosy was discovered for the first time by Guy Henry Faget and his co-workers in 1943 in Carville, Louisiana, and then used in the different Leproseries of the world[44-54].
DIAMINODIFENILSULFONE (DDS) was then synthesized in commercial presentation of 100 mg tablets. Then appeared RIFAMPICIN (1965) and the CLOFAZIMINE or Lamprene (1971) and the so-called MTD (Multi Drugs Therapy) was established with these three medicines. This event is what decrees the closure of Leproseries in the world, keeping patients under strict control of their medications. In fact, patients already outside the leprosarium went to the epidemiological control centers monthly and were educated how to take the medications and their possible adverse reactions[44-54].
Conclusion
• We present two cases of Leprosy diagnosed in 2017 and 2018 that were present for 8 and 10 years, respectively. We alert the local health authorities to search contacts in the zones of these two patients in order to identify other infected or exosed individuals.
• Today, thousands of years have passed and we can even say that “Leprosy 2,000 years later”[55] is a disease that continues to exist throughout the world, and as an example of this we present these two cases who attended our private clinic. They meet the criteria to classify them within the tuberculoid leprosy spectrum, one of them “migrating” to the Borderline pole. The male case was referred to Caracas (Capital City of the Venezuela’s Republic), the division of Leprosy, for treatment, and the female case decided to go to another country to seek treatment.
• Leprosy as a disease has not been eliminated from the world and much less from Venezuela, where it is said that our great researcher, Convit in 1987 discovered “a cure or vaccine against Leprosy”.[56] Dr. Convit discovered an “immunotherapy” for leprosy. His invaluable work earned him the Prince of Asturias Award, but I repeat, his is not the definitive cure against Leprosy.[57]
• Convit died in 2014 and for 2015 The World Health Organization (WHO) reports 215,000 thousand new cases of leprosy in the world. India accounts for the largest number of cases, followed by Brazil and Indonesia.[5]
• Dr. Pedro Lapenta, our mentor and a great Dermatologist and Leprologist, published 14 works on Leprosy 12 together with Convit[10-23].
• We hope to raise awareness in the medical and non-medical society that this biblical plague still persists throughout the world. Its incidence has diminished but still exists, despite the advances in medicines. It is worth noting that even in a private practice setting, Hansen’s disease patient (eg, pt No.1) could present with a simple lesion which might be confuse with other pathologies like granuloma annulare or tinea corporis.
Commentary
Anecdotally we can tell you that in 1948, Dr. Lapenta and Convit, were studying a case of Leprosy, type diffuse Lepromatous in the Leprocomium of Cape White, located in the State Vargas, Venezuela and surprisingly found in the biopsy of skin lesions, “amastigotes” forms of Cutaneous Leishmaniasis, both proceeded to publish the case and became the first to describe this “New” finding on Cutaneous Leishmaniasis under the name of Diffused Anergic Cutaneous Leishmaniasis, and they remained in the history of dermatology as the discoverers of this entity[58].
Conflicts of Interest
We declare no conflicts of interest of any kind, in relation to countries, governments, institutions and individuals.
Thanks
To my Father and grandfather of my son Dr. Pedro Lapenta (1921-2011), a great Dermatologist and Leprologist, who practiced Dermatology for 55 years and trained me very well in this art of Dermatology and Leprology. Apart from that, he is in the history of medicine as one of the discoverers of Diffuse Anergic Cutaneous Leishmaniasis.
To Dr. Jacinto Convit who together with my Father formed the master key in Venezuela against Leprosy, in the years 40-65s, and inventor of the “Immunotherapy” against Leprosy.
To my son, Dr. José Miguel Lapenta, Doctor graduated from the University of Carabobo, who is part of the DERMAGIC EXPRESS team, and is my new great machine and co-author in most of the works.
To the Ommega Team who always suggest interestings facts about our works.
References
- 1. Sagrada Biblia: Levítico 13:3; 13:12.
Pubmed|| Crossref|| Others
- 2. Monot, M., Honoré, N., Garnier, T., et al. On the origin of leprosy. (2005) Science 308 (5724): 1040-1042.
- 3. Robbins, G., Tripathy, V.M., Misra, V.N., et al. Ancient skeletal evidence for leprosy in India (2000 B.C.). (2009) PLoS One 4(5): 5669.
- 4. Robbins Schug, G., Blevins, K., E., Brett, C., et al. Infection, Disease, and Biosocial Process at the End of the Indus Civilization. (2013) PLoS ONE 8(12): 84814.
- 5. Global leprosy update, 2016: accelerating reduction of disease burden. (2017) Weekly epidemiological record WHO: 501-520.
Pubmed|| Crossref|| Others
- 6. Irgens, L.M. The discovery of the leprosy bacillus. (2002) Tidsskr nor Laegeforen 122 (7): 708-709.
Pubmed|| Crossref|| Others
- 7. New Leprosy Bacterium: Scientists Use Genetic Fingerprint to Nail ‘Killing Organism’. University of Texas M. D. Anderson Cancer Center. Science Daily. (2018)
Pubmed|| Crossref|| Others
- 8. Lapenta, J. Lepra en la Isla de Providencia. Universidad de Carabobo. Dermatología y Bibliografía. Dermagic Express.
Pubmed|| Crossref|| Others
- 9. Lapenta, J. Lepra en Cabo Blanco. Universidad de Carabobo. (2018) Dermatología y Bibliografía. Dermagic Express.
Pubmed|| Crossref|| Others
- 10. Convit, J., Lapenta, P., Ilukevich, A., et al. Experimental Inoculation of Human Leprosy in Laboratory Animals. (1964) Int J Lepr 32: 136-149.
- 11. Ilukevich, A., Convit, J., Imaeda, T., et al. Comments on the stautus of Mycobacteria in modern Taxonomy. (1964) Rev Venez Sanid Asist Soc 29: 98-110.
Pubmed|| Crossref|| Others
- 12. Convit, J., Lapenta, P., Ilukevich, A., et al. Experimental Inoculation of Laboratory animals with Human Leprosy. (1964) Rev Venez Sanid Asist Soc 29: 65-74.
Pubmed|| Crossref|| Others
- 13. Imaeda, T., Convit, T., Lapenta, P., et al. Electron Microscopic study of Borderline Leprosy. (1963) Int J Lepr 31: 389-417.
- 14. Imaeda, T., Convit, J., Ilukevich, A., et al. Experimental inoculation of human leprosy in laboratory animals. II. Electron microscope study. (1962) Int J Lepr 30: 395-413.
Pubmed|| Crossref|| Others
- 15. Convit, J., Lapenta, P., Ilukevich, A., et al. Experimental inoculation of human leprosy in laboratory animals. (1962) Int J Lepr 30: 239-253.
Pubmed|| Crossref|| Others
- 16. Mendoza, S.J., Lapenta, P., Arvelo, J.J., et al. Treatment of leprosy with DPT in the Cabo Blanco sanatorium. (1961) Rev Sanid Asist Soc 26: 397-406.
- 17. Convit, J., Lapenta, P., Mendoza, S.J. The methylene blue test in the exploration of the leprosy patient. (1961) Rev Sanid Asist Soc 26: 392-396.
Pubmed|| Crossref|| Others
- 18. Convit, J., Ilukevich, A., Lapenta, P., et al. Experimental inoculation of animals with Mycobacterium leprae. (1961) Rev Sanid Asist Soc 26: 388-389.
Pubmed|| Crossref|| Others
- 19. Convit, J., Lapenta, O., Mendoza, S.J. The methylene blue test in leprosy. (1960) Int J Lepr. 28: 233-238.
- 20. Convit, J., Sisiruca, C., Lapenta, P. Some observations on borderline leprosy. (1956) Int J Lepr 24: 375-81
Pubmed|| Crossref|| Others
- 21. Siriruca, C., Lapenta, P. Contribution to the study of dimorphous leprosy. (1955) Gac Med Caracas 63: 308-10
Pubmed|| Crossref|| Others
- 22. Convit, J., Lapenta, P., Jorgersen, J. The Mantoux and Mitsuda reactions in hamsters and guinea-pigs before and after vaccination with BCG. (1955) Int J Lepr 23(2): 162-166.
- 23. Reyes, O., Lapenta, P. Lepra Tuberculoide reaccional Ulcerada. (1962) Rev sovderma 3: 1-2
Pubmed|| Crossref|| Others
- 24. Pereira, A.C. Hanseniase de Lucio. (1993) An. Bras. Dermatol 68: 33-40.
Pubmed|| Crossref|| Others
- 25. Vargas-Ocampo, F. Diffuse leprosy of Lucio and Latapí: a histologic study. (2007) Lepr. Rev 78(3): 248-260.
- 26. Saúl, A., Novales, J. Lucio-Latapí leprosy and the Lucio phenomenon. (1983) Acta Leprol. 1(3): 115-132.
Pubmed|| Crossref|| Others
- 27. Latapi, F., Zamora, A.C. La lepra “manchada” de Lucio (estudio inicial clinico e histopatológico). (1948) In: Memoria do V Congreso International de la Lepra – Havana : 410-413.
Pubmed|| Crossref|| Others
- 28. Latapi, F., Zamora, A.C. The “spotted” Leprosy of Lucio (La lepra “manchada” de Lucio); an introduction to its clinical and histological study. (1948) Int. J. Lepr. 16(4): 421-429.
Pubmed|| Crossref|| Others
- 29. Lapenta, J. Lepra y Fenomeno de Lucio. (2017) Universidad de Carabobo. Dermatología y Bibliografía. Dermagic Express.
Pubmed|| Crossref|| Others
- 30. Mitsuda, K. The significance of skin tests using leprosy nodule extracts. (1919) Jpn J Dermatol Urolog.
Pubmed|| Crossref|| Others
- 31. Sato, S Outlook of The Third International Leprosy Congress, Papers on Leprosy (2) by Kensuke Mitsuda. (1950) Int J Leprosy 62(3): 412-419.
Pubmed|| Crossref|| Others
- 32.Hayashi, F. Mitsuda’s skin reaction in leprosy. (1933) Intern J Lepr 1: 31-38.
Pubmed|| Crossref|| Others
- 33. Ridley, D.S., Jopling, W.H. Classification of leprosy according to immunity. A five-group system. (1966) Int. J. Lepr. Other Mycobact. Dis 34(3): 255-273.
- What Is Leprosy? (2010) Consultado.
Pubmed|| Crossref|| Others
- 35. Lapenta, P. Conversatorio sobre Lepra y su diagnostico (1984-1987). (2018)
Pubmed|| Crossref|| Others
- 36. Truman, R.W., Singh, P., Sharma, R., et al. Probable Zoonotic Leprosy in the Southern United States. (2011) N Engl J Med 364(17): 1626-1633.
- 37. Walsh, G.P., Meyers, W.M., Binford, C.H., et al. Leprosy as a zoonosis: an update. (1988) Acta Leprol 6(1): 51-60.
Pubmed|| Crossref|| Others
- 38. Meredith, A., Del Pozo, J., Smith, S., et al. Leprosy in red squirrels in Scotland. (2014) Vet Rec 175 (11): 285-286.
- 39. Avanzi, C., Del-Pozo, J., Benjak, A., et al. Red squirrels in the British Isles are infected with leprosy bacilli. (2016) Science 354(6313): 744-747.
- 40. Carole, R. Leprosy in Medieval England (2009).
Pubmed|| Crossref|| Others
- 41. Francisco, J.L.A. Diagnóstico y tratamiento de la lepra. (1998) salud pública de México 40(1): 1-10.
Pubmed|| Crossref|| Others
- 42. Suzuki, K., Akama, T., Kawashima, A., et al. (February). Current status of leprosy: epidemiology, basic science and clinical perspectives. (2012) J Dermatol 39(2): 121–129.
- 43. Leonard, R., Ernest, M., Leprosy. (1946) Int lep Ass: 22.
Pubmed|| Crossref|| Others
- 44. Ravina, E., Kubinyi, H. The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. (2011) Wiley: 528.
Pubmed|| Crossref|| Others
- 45. Wozel, G. The Story of Sulfones in Tropical Medicine and Dermatology. (1989) Int J Dermatol 28(1): 17-21.
- 46. Jacobsen, P.L., Levy, L. Mechanism by which hydnocarpic acid inhibits mycobacterial multiplication. (1973) Antimicrobial Agents Chem 3(3): 373-339.
- 47. Simpkin, A. The Treatment of Leprosy. (1928) British J Nursing: 313–314.
Pubmed|| Crossref|| Others
- 48. Sengupta, A., Gupta, J., Dutta, J., et al. The component fatty acids of chaulmoogra oil. (1973) J Sci Food and Agriculture. 24(6): 669-674.
- 49. Convit, J., Browne, S.G., Languillon, J., et al. Therapy of leprosy. (1970) Bull World Health Organ 42(5): 667-672.
Pubmed|| Crossref|| Others
- 50. Sensi, P. History of the development of rifampin. (1983) Rev Infect Dis 5(3): 402–406.
Pubmed|| Crossref|| Others
- 51. Faget, G.H., Pogge, R. C., Johansen, F. A., et al. The Promin Treatment of Leprosy. (1943) Public Healt Rep 58(40): 1729-1741.
Pubmed|| Crossref|| Others
- 52. Dougall, A.C. Dapsone. (1979). Clin. Exp. Dermatol. 4(2): 139–142.
Pubmed|| Crossref|| Others
- 53. Desikan, K. V. Multi-drug Regimen in Leprosy and its impact on Prevalence of the Disease. (2003) Med J Armed Forces India 59(1): 2-4.
- 54. Fischer, M. Leprosy - an overview of clinical features, diagnosis, and treatment. (2017) J Dtsch Dermatol Ges 15(8): 801-827.
- 55. Lapenta, J. La Lepra 2000 Años después. Bibliografía Dermatología DERMAGIC EXPRESS. (2017)
Pubmed|| Crossref|| Others
- 56. Isla de providencia. (Venezuela). (2018).
Pubmed|| Crossref|| Others
- 57. Jacinto Convit, y Pablo Rudomin. (1987).
Pubmed|| Crossref|| Others
- 58. Convit, J., Lapenta, P. Sobre un caso de leishmaniasis tegumentaria de forma diseminada. (1948) Rev. Policlínica Caracas: 153-158.
Pubmed|| Crossref|| Others