Lupus: The Great Pretender, Breast Manifestations of SLE
Angelica Robinson, Sarfaraz Sadruddin, Candace Bailey, Uzoma Igboagi, Suimin Qiu, Quan Nguyen
Affiliation
- Department of Radiology and Pathology, UTMB, University Boulevard, Galveston, TX, USA
Corresponding Author
Stephen Herrmann, MD/MS, Department of Radiology and Pathology, UTMB, 301 University Boulevard, Galveston, TX-77555, USA. Tel: 832-723-0206; E-mail: saherrma@utmb.edu
Citation
Herrmann, S., et al. Lupus: The Great Pretender, Breast Manifestations of SLE. (2015) Intl J Cancer Oncol 2(3): 1-3.
Copy rights
© 2015 Herrmann, S. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Breast manifestations; Systemic Lupus Erythematosus (SLE); Lymph nodes
Abstract
Lupus mastitis is an infrequent sequela of the autoimmune disease Systemic Lupus Erythematosus (SLE) which can be confounding to both clinicians and diagnosticians due to its similar appearance to an infectious or even neoplastic process. This case demonstrates a patient who presented with a painful and edematous breast that was initially concerning for mastitis or underlying abscess on the initial clinical examination. After a trial of antibiotics, the patient’s symptoms minimally approved with subsequent work up using mammogram and ultrasound concerning for a possible malignancy. Ultrasound guided needle and core biopsies eventually led to the diagnosis of lupus mastitis. This report discusses the clinical, radiological and histological presentation of lupus mastitis. This is importation for clinicians so they can have a better understanding of this unique presentation of SLE and can prevent unnecessary invasive procedures which may further increase inflammation involved with lupus mastitis. While SLE has a multitude of clinical presentations this case report demonstrates another unique way that SLE can be encountered.
Introduction
In October 2014, a 39 year old female with PMH of Crohn’s disease, Systemic Lupus Erythematosus (SLE), Chronic Heart Failure (CHF) and Hypertension (HTN) was admitted to our hospital due to a progressively painful and edematous right breast. The symptoms lasted for approximately 2 weeks and they were concerning for mastitis with possible abscess formation. She also complained of an enlarged right axillary lymph node that that was subjectively larger in size. She reported that a prior breast ultrasound and mammogram had “normal” results when they were obtained the year before at an outside facility. Of note, the patient did not remember the name of the outside facility, so these images were not available for comparison. She denied any recent breast laceration, trauma, nipple discharge or fever. She also denied any history of breast surgery or family history of any type of cancer. She was gravida 3, para 3 with her first live birth at age 17; she was currently using the Depo-Provera shot for birth control.
On physical exam, her right breast was asymmetrically enlarged as compared to the left breast, mildly tender to palpation, and firm with associated skin thickening. Pertinent negatives included no nipple discharge or lacerations. A mobile right axillary lymph node, measuring approximately 2x2 cm, was mildly tender to palpation. These findings were initially concerning for cellulitis or an underlying breast abscess, so oral antibiotic treatment was initiated. Subsequently, a minimal decrease in the amount of her right breast swelling was noted.
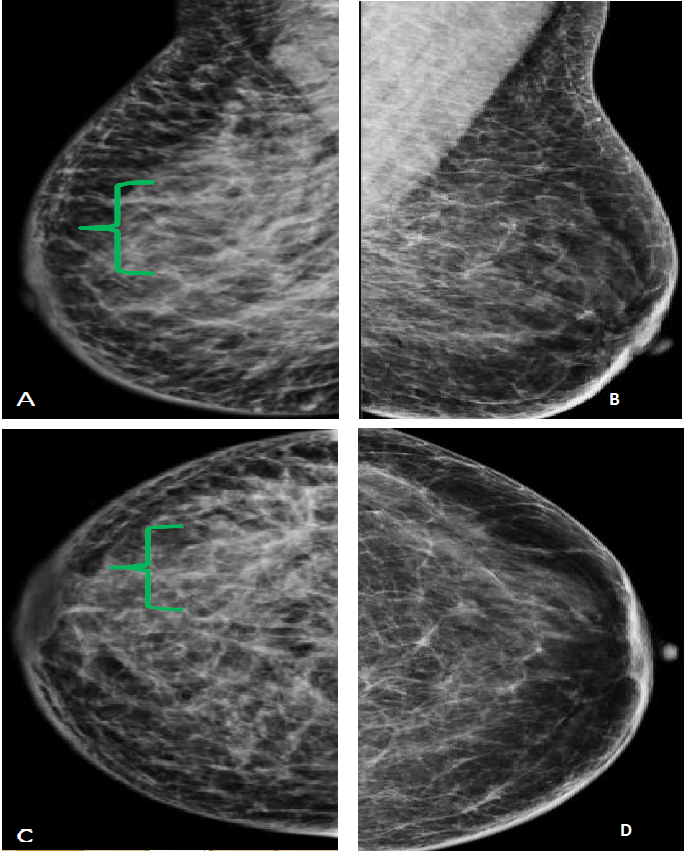
Bilateral CC and MLO mammographic views were obtained (Fig 1) and showed a heterogeneously breasts with right breast diffuse skin (red arrow) and trabecular (green bracket) thickening (Fig 1a/c).
Figure 1: (a). RMLO (b). LMLO (c). RCC (d). LCC. Bilateral MLO and CC views show increased skin and trabecular thickening throughout the right breast as compared to the left
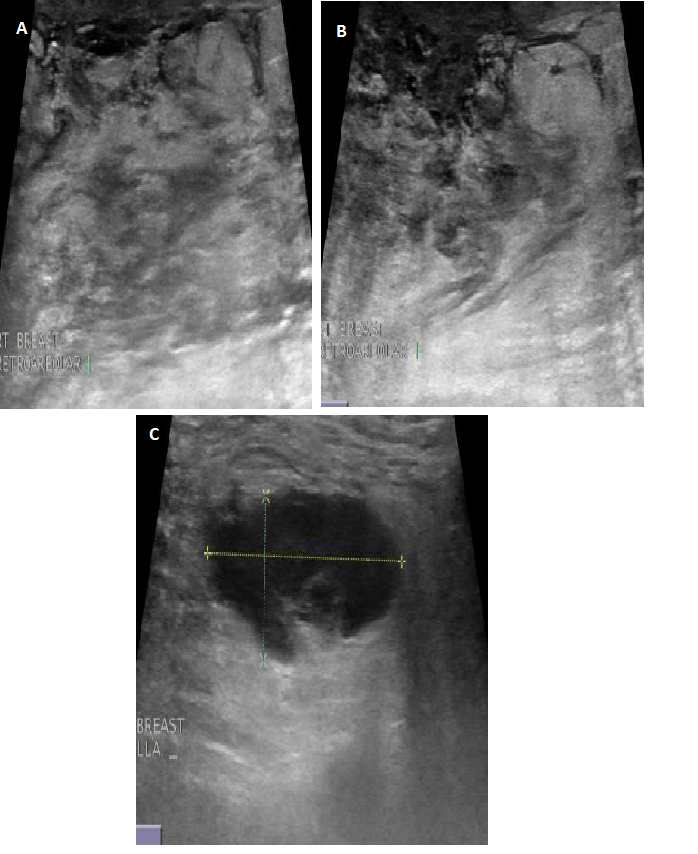
Targeted right breast ultrasound demonstrated diffuse edematous breast tissue (Fig 2a) with a questionable solid component (Fig 2b, red arrow) and right axillary lymphadenopathy (Fig 2c).
Given that these findings persisted with antibiotic treatment, an underlying malignancy was included in the differential diagnosis, and the examination was given a BIRADS 4 rating which warranted a biopsy.
Figure 2: (a/b). Edematous retroareolar tissue in the right breast with heterogeneous echotexture, and a questionable solid component. (c). Right axilla demonstrating an enlarged and abnormal appearing lymph node.
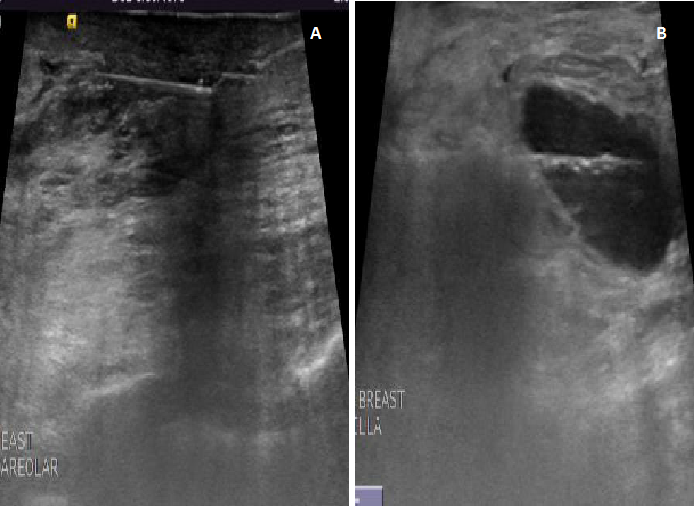
Ultrasound guided biopsies were performed targeting the solid component noted in the edematous breast tissue (Fig 3a) and right axillary lymphadenopathy (Fig 3b).
Figure 3: (a). Right breast biopsy. (b) Right axillary lymph node biopsy.
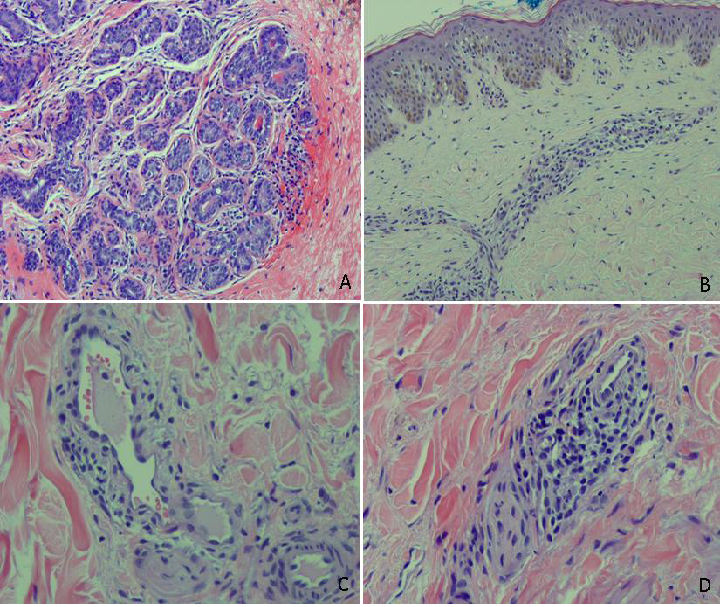
The pathology results from the ultrasound guided biopsy of the right breast were reported as: benign breast parenchyma with fibrocystic changes including ductal dilatation, stromal fibrosis, sclerosing adenosis and mild perilobular and intralobular lymphoplasmacytic infiltrate (Fig. 4a). No acute inflammatory changes or malignant cells were noted. The right axillary lymph node showed reactive benign lymphadenopathy. These pathology results were considered discordant since the radiographic findings were still concerning for an underlying inflammatory breast cancer. Consequently, a skin punch biopsy was recommended for a definitive diagnosis.
The skin punch biopsy (Fig 4) demonstrated superficial and deep perivascular lymphoplasmocytic infiltrate (Fig 4b), consistent with a history of systemic lupus involvement with perivascular and periadnexal lymphoplasmacytic infiltrate (Figure 4c/4d); no malignant cells were visualized.
Figure 4: Ultrasound-guided breast core needle biopsy histology 100X (a), Skin punch biopsy histology (b)100X (c) 200X (d) 400X
Lupus mastitis typically presents as a tender mass on clinical exam. This disease is not a neoplastic process, but rather, an infrequent sequela of the autoimmune disease systemic lupus erythematosus (SLE). SLE has the potential to involve a variety of organs secondary to complications associated with wide spread inflammatory changes of the connective tissues. A subset of SLE, lupus profundus or panniculitis, affects approximately 2-3% of SLE patients and causes an inflammatory reaction of the panniculus, or subcutaneous adipose tissue. First described in 1971 by Tuffanelli, lupus mastitis is the clinical correlate of lupus panniculitis within the breast tissue and usually, but not always, presents with a single tender breast mass in a previously diagnosed SLE patient. Similar to most autoimmune diseases, lupus mastitis predominately affects women of childbearing age, with 37 years as the mean age at presentation. The overlying skin can be asymptomatic, or may show signs of erythema, ulceration, hyperkeratosis or poikilothermic changes[1]. Although, lupus mastitis can look and feel similar to a neoplastic tumor, this disease has a benign course. Management includes medical treatment to subdue the amount of inflammation and avoidance of surgery and other invasive procedures in order to prevent aggravation of the underlying inflammation. The physician may need to acquire imaging or tissue samples of the mass in order to confirm the diagnosis, however, a past history of SLE and a high level of clinical suspicion is often needed in order to include this rare breast finding on a differential diagnosis of a breast mass[2]. On imaging, lupus mastitis typically follows a pattern which can aid in making an accurate diagnosis. Mammographic findings in lupus mastitis generally include a poorly defined, heterogeneous mass of dense tissue with irregular borders and coarse calcifications, suggesting fat necrosis. Ultrasonography shows a hyperechoic, poorly defined mass with irregular borders and heterogeneity. Dermal thickening with increased vascularity can also be seen. With magnetic resonance imaging (MRI), a post-contrast peripheral rim of inflammatory enhancement has been noted. Serial MRI’s may serve as a useful marker for response to therapy as indicated by reduced intensity and thickness of the enhancing rim[3].
Tissue findings prove to be the most definitive way to confirm a diagnosis of lupus mastitis. Lymphocytic infiltration, occasional germinal centers and marked hyaline fat necrosis with sclerosis are considered pathognomonic findings. Lupus mastitis is a chronic inflammatory disease with remissions and recurrences being a common presentation. First line therapy includes oral hydroxychloroquine, an anti-malarial agent, with remission usually occurring in 3-6 months. More complicated cases may also require treatment with systemic steroids for an overall improvement in the patient’s symptoms. Cyclophosphamide has shown varying degrees of effectiveness as a steroid sparing treatment option. In severe cases, mastectomy may be indicated for symptom control[4].
References
- 1. Warne, R.R., Taylor, D., Segal, A., et al. Lupus Mastitis: a Mimicker of Breast Carcinoma. (2011) BMJ Case Rep 2011: 5066.
- 2. Summers, T.A., Jr, Lehman, M.B., Barner, R., et al. Lupus mastitis: a clinicopathologic review and addition of a case. (2009) Adv Anat Pathol 16(1): 56-61.
- 3. Mosier, A.D., Boldt, B., Keylock, J., et al. Serial MR Findings and Comprehensive Review of Bilateral Lupus Mastitis with an Additional Case Report. (2013) J Radiol Case Rep 7(1): 48-58.
- 4. Kinonen, C., Gattuso, P., Reddy, V.B. Lupus Mastitis: An Uncommon Complication of Systemic or Discoid Lupus. (2010) Am J Surg Pathol 34(6): 901-906.