PREVALENCE OF HYPERTENSIVE DISORDERS IN PREGNANCY AT KORLE-BU TEACHING HOSPITAL IN GHANA
Kwame Adu-Bonsaffoh1,3*, Michael Y Ntumy2, Samuel A Obed2, Joseph D Seffah2
Affiliation
- 1Department of Obstetrics and Gynaecology, Korle Bu Teaching Hospital, Accra, Ghana.
- 2Department of Obstetrics and Gynaecology, School of Medicine and Dentistry, University of Ghana, Accra, Ghana.
- 3Department of Physiology, School of Allied and Biomedical Science, University of Ghana, Accra, Ghana.
Corresponding Author
Kwame Adu-Bonsaffoh, Department of Obstetrics and Gynaecology, Korle Bu Teaching Hospital PO Box KB783, Korle Bu, Accra, Ghana, Tel: +2332244295763; E-mail: bonsaffoh@yahoo.com
Citation
Adu-Bonsaffoh, K., et al. Prevalence of Hypertensive Disorders in Pregnancy at Korle-Bu Teaching Hospital in Ghana. (2017) J Gynecol Neonatal Biol 3(1): 8-13.
Copy rights
© 2017 Adu-Bonsaffoh, K. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Prevalence; Preeclampsia; Eclampsia; Gestational Hypertension; Chronic Hypertension; Hypertensive Disorders; Ghana.
Abstract
Background: The true burden of Hypertensive Disorders in Pregnancy (HDP) has been difficult to determine with significant accuracy globally as a result of considerable inconsistencies regarding their prevalence due to lack of definite terminologies and classification.
Objective: To determine the current prevalence and relative contribution of the various categories of HDP to the burden of maternal hypertension at Korle Bu Teaching Hospital (KBTH) using the recent globally acknowledged consensus classification by the International Society for the Study of Hypertension in Pregnancy (ISSHP).
Methods: A cross sectional study conducted between January and February 2013 at the KBTH in Accra, Ghana.
Results: There were a total of 398 women with HDP among 1856 deliveries during the study period resulting in prevalence of 21.4%. The proportions of the various types of HDP include 184 (50.0%), 140 (38.0%), 23 (6.3%) and 21 (5.7%) representing gestational hypertension, preeclampsia, chronic hypertension and superimposed preeclampsia respectively. Eclampsia occurred in 58 (15.8%) women. The prevalence of gestational hypertension, preeclampsia chronic hypertension, chronic hypertension with superimposed preeclampsia with respect to the total singleton deliveries were 10.4%, 7.9%, 1.3% and 1.2% respectively. Parity-specific prevalence of HDP showed an increasing trend with the lowest and highest relative proportions occurring in women who had parity of one and 5 or more respectively. Age-specific prevalence showed a steep decline after maternal age of 19 years followed by a general rise after 25 years with highest rate occurring after maternal age of 35 years.
Conclusion: There is a significant burden of HDP in the Ghanaian population as evidenced by a high prevalence of 21.4% at the largest tertiary hospital in the country. Gestational hypertension represented the largest proportion followed by preeclampsia, chronic hypertension and superimposed preeclampsia on chronic hypertension. Parity-specific prevalence was highest among women with grand multiparity whereas age-specific prevalence was highest after maternal age of 35 years.
Introduction
Hypertensive disorders in pregnancy (HDP) remain a major clinical challenge in contemporary obstetric practice due to the associated burden of high maternal and perinatal adversities[1-4]. They are common medical conditions in pregnancy responsible for approximately 14% of maternal deaths globally[5]. In Ghana, maternal mortality ratio remains excessively high and HDP are responsible for about 9% of maternal deaths[6]. However, recent clinical studies in Ghana have indicated that HDP are the leading cause of maternal deaths in the major tertiary institutions[7,8] with similar findings reported in other African countries[9,10].
However, the true burden of HDP has been difficult to determine with accuracy as a result of significant inconsistencies regarding the prevalence of HDP globally. This is generally due to lack of definite consensus relating to the optimal classification and diagnostic criteria for these disorders. In the year 2000, the definitions and the classifications were streamlined by the International Society for the Study of Hypertension in Pregnancy (ISSHP)[11]. Based on the ISSHP consensus classification HDP was classified into preeclampsia, gestational hypertension, chronic hypertension and preeclampsia superimposed on chronic hypertension. The ISSHP consensus statement regarding the definitions and the classification was based mainly on the propositions by the National High Blood Pressure Education Program and the Australasian Society for the Study of Hypertension in Pregnancy (ASSHP)[12,13]. More recently, the ISSHP has published another consensus statement on HDP with the inclusion of white coat hypertension in the classification system. However, the controversy is not fully resolved especially for preeclampsia which has attracted both clinical and research definitions[14]. The lack of definite terminologies and classification has resulted in controversies regarding the prevalence and optimal management of these high risk obstetric disorders.
The prevalence of HDP has therefore been variously described depending on the population, definition and classification used with resultant effect of under or over-estimation due to the lack of global consensus on these controversies. In KBTH, where the current study was undertaken, the morbidity and mortalities associated with HDP have previously been reported[7,15,16] although the prevalence has not yet been adequately studied indicating a significant knowledge gap regarding the epidemiology of HDP. The main objective of this study was to determine the current prevalence of HDP among the obstetric population and the relative contribution of the various categories of HDP to the burden of this clinical syndrome at KBTH via a prospective data collection, using globally acknowledged consensus classification by the International Society for the Study of Hypertension in Pregnancy (ISSHP). The findings of this study would provide a gross overview of the prevalence HDP in tertiary hospitals in Sub-Saharan Africa.
Materials and Methods
This was a cross sectional study conducted between 1st January and 28th February 2013 at the Department of Obstetrics and Gynaecology of Korle Bu Teaching Hospital (KBTH), in Accra, Ghana. This was part of a larger study that determined the maternal and perinatal outcomes of HDP at the hospital[15]. Korle Bu Teaching Hospital is situated in the capital city, Accra, where it serves as a tertiary referral centre for most of the peripheral health facilities. In the hospital, the National Health Insurance (NHI) free delivery scheme covers all the pregnant women who access the maternity services. The maternity unit of the hospital conducts over 10,000 deliveries annually with a caesarean rate of about 35%[17]. Antenatal care is offered on daily basis from Monday to Friday at Maternity unit and about 200 pregnant women attend antenatal clinic daily. The pregnant women reporting for ANC are usually weighed; have their urine tested for glucose, ketones and protein after which their blood pressures are measured before seeing a doctor. This routine screening is necessary in early detection and management of pregnant women whose pregnancies have been complicated by HDP in the hospital.
In this study, we included all pregnant women who developed HDP and gave birth at KBTH. The study excluded women who delivered in a peripheral health institution prior to their referral to KBTH for further management. An initial baseline data collection was done consisting of daily identification of all women who gave birth at the two labour wards of the Maternity unit over the past 24 hours. The initial screening involved extraction of data from admission and discharge books at the labour and recovery wards of the hospital. After the baseline data collection on all women who had recently delivered at the hospital, those with HDP were identified and their folder numbers recorded. These selected parturient with HDP were traced to the maternity wards where they had been admitted following delivery. The study protocol was explained to them individually and those who gave informed consent were included in the study. Each participant was informed that her participation in the study was purely voluntary and that she had the right to withdraw for the study at anytime. They were also informed that non participation or withdrawal from the study would not affect the standard management of their respective medical treatment at the hospital.The informed consent was obtained from next of kins or guardians of study participants who could not give informed consent because of their health status and those who were below 18 years of age. The study protocol was approved by the Ethical and Protocol Review Committee of the School of Medicine and Dentistry, University of Ghana.
Socio-demographic characterisitics such as age, educational status, marital status and obstetric data such as gravidity, parity, gestational age at booking, gestational age at delivery, blood pressure at booking, blood pressure at the time of admission were obtained using a structured questionnaire and by reviewing the medical records of the participants. The study participants were followed up at the postnatal clinic at one or two weeks and at six weeks following delivery to identify those whose hypertension had not resolved. This was done to properly classify the women into the appropriate categories of hypertensive disorders in pregnancy based on definition by the International Society for the study of hypertension in pregnancy[9].
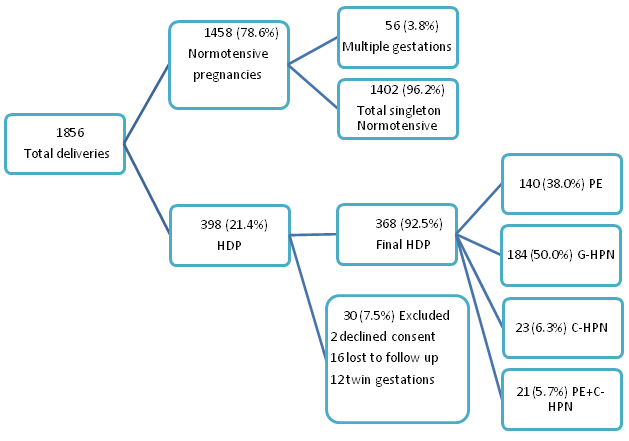
In this study, hypertensive disorders in pregnancy were classified according to the classification system described by the International Society for the study of hypertension in pregnancy including preeclampsia, gestational or transient hypertension, chronic hypertension and preeclampsia superimposed on chronic hypertension[9]. Hypertension in pregnancy was defined as systolic Blood Pressure (BP) ≥ 140 mmHg and/or a diastolic BP ≥ 90 mmHg respectively. The women with gestational hypertension or preeclampsia who were lost to follow up after delivery were excluded from the analysis since their blood pressures could not be measured to determine if their blood pressures had resolved during the postpartum period. The flow chart indicating the identification of the study participants is shown in Figure 1. Proteinuria was determined using a semi-quantitative dipstick testing. The sample size was determined using the Cochran’s formula[18].
Figure 1: Flow chart showing the distribution of hypertensive disorders in pregnancy at Korle Bu Teaching Hospital.
HDP: hypertensive disorders in pregnancy; PE: pre-eclampsia; G-HPN: gestational hypertension, C-HPN: chronic hypertension; PE+C-HPN: Pre-eclampsia superimposed on chronic hypertension
The data obtained was entered into an Excel spread sheet (Microsoft company, USA) and analyzed using SPSS version 20. Descriptive analysis was performed and appropriate measures of centrality (mean) and dispersion (standard deviation) were calculated as well as percentages and graphical display (bar chart) where appropriate.
Results
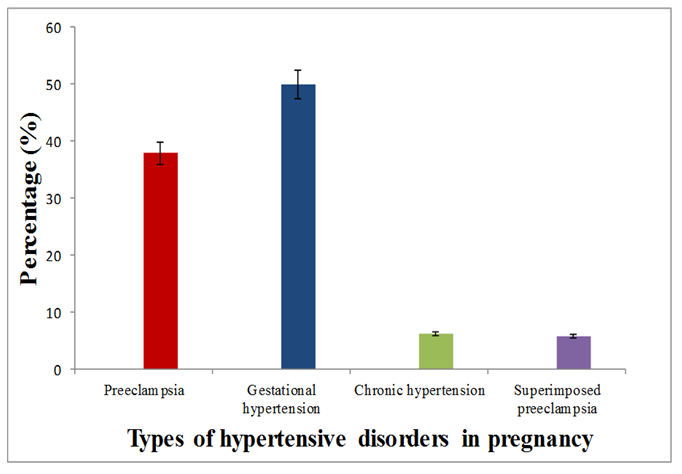
There were a total of 398 women with hypertensive disorders in pregnancy among 1856 deliveries during the study period resulting in prevalence of 21.4%. Two women with hypertensive disorders in pregnancy declined to take part. Sixteen women were lost to follow up after delivery and could not be appropriately classified into the specific types of hypertensive disorders and were excluded from the analysis. Twelve women with multiple gestations and HDP were further excluded from the analysis to better understand burden of hypertension among singleton pregnancies resulting in 368 women with HDP. The proportions of the various types of hypertensive disorders of pregnancy are shown in Figure 2 with 184 (50.0%), 140 (38.0%), 23 (6.3%) and 21 (5.7%) women having gestational hypertension, preeclampsia, uncomplicated chronic hypertension and superimposed preeclampsia respectively. The proportions of uncomplicated chronic hypertension and superimposed pre-eclampsia on Chronic hypertension were 6.3% (23/368) and 5.7% (21/368) respectively.
Figure 2: Frequency of the various types of hypertensive disorder in pregnancy at KBTH.
Chronic hypertension constituted 12% of HDP (44 out of 368) with 21 (47.7%) developing superimposed preeclampsia and 23 (52.3%) remaining uncomplicated. Fifty eight women (15.8%) out of the 368 with HDP developed eclampsia with 50 (86.2%) cases resulting from pre-eclampsia. The prevalence of gestational hypertension, preeclampsia chronic hypertension, chronic hypertension with superimposed preeclampsia with respect to the total singleton deliveries were 10.4%, 7.9%, 1.3% and 1.2% respectively. Among the 1856 deliveries, 1458 were normotensives out of which 56 had multiple gestations which were also excluded from the analysis resulting in 1402 normotensive women with singleton deliveries.
Among the study population 220 (12.4%) had not had any form of formal education comprising 37 (10.1%) and 183 (13.1%) of hypertensive and normotensive women respectively. Similarly, 228 participants comprising 42 (11.4%) and 177 (12.6%) of hypertensive and normotensive women had had tertiary level education respectively. Regarding marital status, 1334 (75.4%) were married comprising 1039 (77.9%) and 295 (22.1%) of hypertensive and normotensive women respectively, whereas 436 (24.6%) were unmarried comprising and single 73 (16.7%) and (83.3%) hypertensive and normotensive women respectively. There were significant differences between women with hypertension in pregnancy and normotensive pregnant women regarding maternal age, parity, gravidity, number of antenatal visits, gestational age at booking and at delivery (Table 1).
Table 1: Demographic data and clinical characteristics of women with hypertensive disorders in pregnancy at KBTH.
| Group parameters | HDP mean ± SD | Normotensive mean ± SD | P value |
|---|---|---|---|
| Age in years | 30.03 ± 5.95 | 28.58 ± 5.62 | 0.001* |
| Gravidity | 3.03 ± 1.85 | 2.67 ± 1.65 | 0.001* |
| Parity | 1.49 ± 1.53 | 1.25 ± 1.31 | 0.002* |
| Number of Antenatal visits | 6.48 ± 2.97 | 6.51 ± 3.30 | 0.902 |
| Gestational age at booking (weeks) | 16.43 ± 6.53 | 17.54 ± 6.88 | 0.005* |
| Systolic BP at delivery (mmHg) | 160.08 ± 17.13 | 119.68 ± 12.34 | 0.001* |
| Diastolic BP at delivery (mmHg) | 106.63 ± 10.73 | 69.22 ± 10.73 | 0.001* |
| Gestational age at delivery (weeks) | 37.41 ± 3.34 | 38.98 ± 2.34 | 0.001* |
*Significant (p < 0.05), SD = Standard Deviation, BP = Blood Pressure, HDP = Hypertensive Disorders in Pregnancy The results in the table are presented as Mean ± Standard Deviation (SD)
The proportion of HDP was highest among nulliparous women (35.3%) with most of them having preeclampsia and gestational hypertension. Women with parity of 5 or more represented 4.6% of the HDP population, with chronic hypertension and superimposed preeclampsia contributing the highest relative proportions. Generally, parity-specific prevalence of HDP showed an increasing trend with the lowest and highest rates occurring in women who had parity of one and 5 or more respectively (Table 2).
Table 2: Prevalence of hypertensive disorders in pregnancies based on maternal parity distribution.
| Parity | PE | G-HPN | C-HPN | PE+C-HPN | Total HDP | Normotensive pregnancies | Total pregnancy population | Parity-specific prevalence (%) |
|---|---|---|---|---|---|---|---|---|
| 0 | 57 (40.7) | 63 (34.2) | 4 (17.4) | 6 (28.6) | 130 (35.3) | 498 (35.5) | 628 (35.5) | 20.7 |
| 1 | 27 (19.3) | 44 (23.9) | 5 (21.7) | 2 (9.5) | 79 (21.5) | 442 (31.5) | 520 (29.4) | 15.2 |
| 2 | 29 (20.7) | 31 (16.8) | 8 (34.8) | 4 (19.0) | 72 (19.6) | 217 (15.5) | 289 (16.3) | 24.9 |
| 3 | 17 (12.1) | 23 (12.5) | 4 (17.4) | 4 (19.0) | 48 (13.0) | 149 (10.6) | 197 (11.1) | 24.4 |
| 4 | 7 (5.0) | 13 (7.1) | 0 (0.0) | 3 (14.3) | 23 (6.3) | 61 (4.4) | 84 (4.7) | 27.4 |
| ≥ 5 | 3 (2.1) | 10 (5.4) | 2 (8.7) | 2 (9.5) | 17 (4.6) | 35 (2.5) | 52 (2.9) | 32.7 |
| Total | 140 (100) | 184 (100) | 23 (100) | 21 (100) | 368 (100) | 1402 (100) | 1770 (100) | 20.8 |
HDP: Hypertensive Disorders in Pregnancy; PE: Pre-Eclampsia; G-HPN: Gestational Hypertension; C-HPN: Chronic Hypertension; PE+C-HPN: Pre-Eclampsia Superimposed on Chronic Hypertension
The prevalence of HDP regarding age group distribution showed the highest proportion among women aged between 25 and 29 years with most of them having preeclampsia and gestational hypertension. The lowest proportion occurred among women who were 40 years and above with the highest relative prevalence occurring in the chronic hypertensive group. Age group-specific prevalence showed a steep decline after maternal age of 19 years followed a general rise after 24 years with highest relative prevalence occurring after maternal age of 35 years (Table 3).
Table 3: Prevalence of hypertensive disorders in pregnancies based on maternal age distribution.
| Age group | PE | G-HPN | C-HPN | PE+C-HPN | Total HDP | Normotensive pregnancies | Total pregnancy population | Age group-specific prevalence (%) |
|---|---|---|---|---|---|---|---|---|
| < 20 | 9 (6.4) | 11 (6.0) | 0 | 0 | 20 (5.4) | 74 (5.3) | 94 (5.3) | 21.3 |
| 20-24 | 17 (12.1) | 27 (14.7) | 0 | 1 (4.8) | 45 (12.2) | 283 (20.1) | 328 (18.5) | 13.7 |
| 25-29 | 53 (37.9) | 43 (23.4) | 9 (39.1) | 1 (4.8) | 106 (28.8) | 430 (30.7) | 536 (30.3) | 19.8 |
| 30-34 | 40 (28.6) | 52 (28.3) | 6 (26.1) | 7 (33.3) | 105 (28.5) | 400 (28.5) | 505 (28.5) | 20.8 |
| 35-39 | 19 (13.6) | 39 (21.2) | 6 (26.1) | 11 (52.4) | 75 (20.4) | 175 (12.5) | 250 (14.1) | 30.0 |
| ≥ 40 | 2 (1.4) | 12 (6.5) | 2 (8.7) | 1 (4.8) | 17 (4.6) | 41 (2.9) | 58 (3.3) | 29.3 |
| Total | 140 (100) | 184 (100) | 23 (100) | 21 (100) | 368 (100) | 1402 (100) | 1770 (100) | 20.8 |
HDP: Hypertensive Disorders in Pregnancy; PE: Pre-Eclampsia; G-HPN: Gestational Hypertension; C-HPN: Chronic Hypertension; PE+C-HPN: Pre-Eclampsia Superimposed on Chronic Hypertension
Discussion
Hypertensive disorders in pregnancy remain a major public health issue world¬wide, and their prevalence varies from one country to another and from one institution to the other. In this study the prevalence of HDP was 21.4% among all the women who delivered at Korle Bu Teaching Hospital during the study period. The prevalence of HDP determined in the current study is obviously high although it is consistent with the reported incidence of 12 - 22% of all pregnancies depending on the population and the definitions used[3]. More recently, Singh et al reported a prevalence of 17% in a tertiary hospital in Nigeria which is grossly consistent with the finding of the current study[19]. However, some other studies have reported relatively lower prevalence rates such as a recent study from a teaching hospital in Nigeria that reported an incidence of 6.2%[20]. Similarly, Wolde et al determined the prevalence of hypertensive disorders in pregnancy at a teaching hospital in Ethiopia as 8.48%[10] which is also lower than the rate obtained in the current study.
The high prevalence of HDP determined in our study might be attributed to the tertiary status of the study site where most of the high risk obstetric cases and emergencies referred from primary and secondary health facilities are managed. It is most probable that majority of the uncomplicated cases of pregnancies are managed at level of the primary and secondary facilities whilst the complicated ones including HDP are referred to the tertiary centre for specialized multidisciplinary care. This was a hospital-based study conducted in a purely African environment with different socio-economic characteristics and this might partly account for the higher prevalence of hypertensive disorders of pregnancy compared to a population based study.
A previous retrospective review in the same hospital reported the incidence of HDP as 7.6%[7] which is far lower than the figure obtained in the current study. However, the current study consisted of prospective data collection design involving baseline daily review of all the parturient who had delivered just over the previous 24 hours to accurately identify those women whose pregnancies had been complicated with hypertension. The current study design is obviously more advantageous in determining the true prevalence in the hospital compared to a retrospective review. The significantly different prevalence rates reported by various studies, with wide variations, might partly be due to the different terminologies and definitions used in the study methodologies. For instance, the use of the term Pregnancy Induced Hypertension (PIH) has resulted in significant controversies with resultant distortion of the prevalence of HDP. The term PIH is outdated and not recommended globally in current literature[3]. Globally, the issue of inconsistent terminologies and definitions continue to impact negatively in the study of hypertensive disorders in pregnancies with resultant controversies regarding obstetric outcomes as well as appropriate investigations and optimal management. Recently, these concerns and their implications on clinical management were proactively discussed and finally addressed partly by a consensus statement published by the ISSHP with evidence based proposition of new definitions and diagnostic criteria for HDP[14].
This study also determined the frequencies of the various types of hypertensive disorders in pregnancy at KBTH. The proportion of gestational hypertension among all the women with hypertensive disorders was 50.0% which was the highest, followed by preeclampsia (38.0%), chronic hypertension (6.3%) and superimposed preeclampsia on chronic hypertension (5.7%). The findings from this study concur with a recent study from Nigeria by Olusanya and Solanke who reported the frequency of 4.6% for chronic hypertension, 55.6% for gestational hypertension and 39.8% for preeclampsia[20]. The findings from our study indicate that chronic hypertension account for 12% of all the women with hypertensive disorders with 47.5% of them developing superimposed preeclampsia. This finding concurs with the rate of 11.37% reported by Yucesoy et al in 2005[21]. Al-Ghamdi et al reported the incidence of chronic hypertension as 8.7% with 47% developing superimposed preeclampsia[22] which is also consistent with the 47.7% determined in the current study. The prevalence of gestational hypertension, preeclampsia, chronic hypertension and chronic hypertension with superimposed preeclampsia with respect to the total singleton deliveries were 10.4%, 7.9%, 1.3% and 1.2% respectively. The prevalence of preeclampsia determined in the current study concurs with the incidence of 7.03% reported by Obed and Anyeteye in the same hospital in 2006[16].
In this study, nulliparity was associated with the highest proportion of HDP (35.3%) which is consistent with a prevalence of 27.7% reported by Singh et al recently in Nigeria[19]. The lowest prevalence was recorded in women who had parity of one which differs from that Singh et al who determined the lowest prevalence among women with who had parity of 2 and 3. However, parity specific prevalence was highest and lowest among women with grand multiparity (parity of 5 or more) and parity of one respectively. This is a significant finding indicating that most women who had HDP were generally nulliparous, however, the risk of developing HDP among grand multiparous women was highest in this study. This might be attributed to the lower number of women who were multiparous and the tertiary referral status of the study site.
Similarly, age group-specific prevalence showed a steep decline after maternal age of 19 years followed by a general increase with the highest rate occurring after maternal age of 35 years in this study. However, the proportion of HDP with respect to age group distribution showed the peak rate in women aged between 25 and 29 years with most of them having preeclampsia and gestational hypertension. The lowermost proportion occurred among women who were 40 years and above with the highest relative proportion occurring in women with chronic hypertensive. It is interesting to note that there were significant differences between women with hypertension in pregnancy and normotensive pregnant women regarding maternal age, parity, gestational age at booking and at delivery. Further studies may be needed to further explore the characteristics of women whose pregnancies are complicated with hypertension especially in our sub-region.
The limitations of our study rely in the small numbers included in the study coupled with the short duration of the study. However, the findings of this study are generally applicable to clinical practice in our sub-region and more specifically Ghana as this represents baseline prevalence study in the country. Based on the findings reported in the current study, we recommend a larger longitudinal study with adequate power to better understand the relative prevalence and incidence of hypertensive disorders in pregnancy in Ghana and Sub-Saharan Africa as a whole. In the near future, we intend to scale up this study to involve the community to determine the population based prevalence to provide a true reflection of the burden of HDP in the country.
Conclusion
There is a significant burden of HDP in the Ghanaian population as evidenced by a high prevalence of 21.4% in the largest tertiary hospital in the country. Gestational hypertension represented the largest proportion (50.0%) of hypertensive disorders followed by preeclampsia (38.0%), chronic hypertension (6.3%) and superimposed preeclampsia on chronic hypertension (5.7%). Although nulliparity was associated with the highest proportion of HDP (35.3%), parity-specific prevalence was highest among grand multipara. Also, there was a steep decline in age-specific prevalence of HDP after maternal age of 19 years followed a general increase with highest relative prevalence occurring after maternal age of 35 years.
We recommend accurate data collection and management (Registry for hypertensive disorders in pregnancy) especially in Sub-Saharan Africa using the globally recognized ISSHP classification to enable intra and inter facility or international comparison of relevant information regarding hypertensive disorders in pregnancy. Accurate data management is crucial in estimating the true burden of HDP in the subregion and this will enhance and direct appropriate preventive and treatment strategies with subsequent improvement in maternal health.
Conflict of interest:
We declare no conflict of interest.
References
- 1. Duley, L. The Global Impact of Pre-eclampsia and Eclampsia. (2009) Semin Perinatol 33(3): 130-137.
- 2. WHO Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia. (2011) Geneva: World Health Organization.
- 3. ACOG Practice Bulletin No. 33: Diagnosis and management of preeclampsia and Eclampsia. American College of Obstetricians and Gynecologists. (2002) Obstet and Gynecol 99 (1): 159-167.
- 4. Hypertension in pregnancy: the management of hypertensive disorders during pregnancy. (2010) NICE clinical guideline 107.
- 5. Say, L., Chou, D., Gemmill, A., et al. Global causes of maternal death: a WHO systematic analysis. (2014) The Lancet Global Health 2(6): e323-e333.
- 6. Ghana Maternal Health Survey 2007. (2009).
- 7. Adu-Bonsaffoh, K., Oppong, S.A., Binlinla, G., et al. Maternal deaths attributable to hypertensive disorders in a tertiary hospital in Ghana. (2013) Int J Gynaecol Obstet 123(2): 110-113.
- 8. Lee, Q.Y., Odoi, A.T., Opare-Addo, H., et al. Maternal mortality in Ghana: a hospital-based review. (2012) Acta Obstet Gynecol Scand 91(1): 87-92.
- 9. Oladapo, O.T., Lamina, M.A., Fakoya, T.A. Maternal deaths in Sagamu in the new millennium: a facility-based retrospective analysis. (2006) BMC Pregnancy and Childbirth 6: 6.
- 10. Wolde, Z., Segni, H., Woldie, M. Hypertensive disorders of pregnancy in Jimma University specialized hospital. (2011) Ethiop J Health Sci 21(3): 147-154.
- 11. Brown, M.A., Lindheimer, M.D., de Swiet, M., et al. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the international society for the study of hypertension in pregnancy (ISSHP). (2001) Hypertens Pregnancy 20(1): ix–xiv.
- 12. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. (2000) Am J Obstet Gynecol 183(1): S1-S22.
- 13. Brown, M.A., Hague, W.M., Higgins. J., et al. The detection, investigation and management of hypertension in pregnancy. (2000) Aust N Z J Obstet Gynaecol 40(2): 139-155.
- 14. Tranquilli, A.L., Dekker, G., Magee, L., et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. (2014) Pregnancy Hypertens 4(2): 97-104.
- 15. Adu-Bonsaffoh, K., Obed, S.A., Seffah, J.D. Maternal outcomes of hypertensive disorders in pregnancy at Korle Bu Teaching Hospital, Ghana. (2014) Int J Gynecol Obstet 127(3): 238-242.
- 16. Obed, S.A., Aniteye, P. Pregnancy Following Eclampsia: A Longitudinal Study at Korle-Bu Teaching Hospital. (2007) Ghana Med J 41(3): 139-143.
- 17. Tuncalp, O., Stanton, C., Castro, A., et al. Measuring Coverage in MNCH: Validating Women’s Self-Report of Emergency Cesarean Sections in Ghana and the Dominican Republic. (2013) PLoS one 8(5): e60761.
- 18. Cochran, W.G. Sampling Techniques. 2nd Ed. (1963) John Wiley and Sons, Ltd.
- 19. Singh, S., Ahmed, E.B., Egondu, S.C., et al. Hypertensive disorders in pregnancy among pregnant women in a Nigerian Teaching Hospital. (2014) Niger Med J 55(5): 384-388.
- 20. Olusanya, B.O., Solanke, O.A. Perinatal outcomes associated with maternal hypertensive disorders of pregnancy in a developing country. (2012) Hypertens Pregnancy 31(1): 120-130.
- 21. Yucesoy, G., Ozkan, S., Bodur, H., et al. Maternal and perinatal outcome in pregnancies complicated with hypertensive disorder of pregnancy: a seven year experience of a tertiary care center. (2005) Arch Gynecol Obstet 273(1): 43-49.
- 22. Al-Ghamdi, S.M., Al-Harbi, A.S., Khalil, A., et al. Hypertensive Disorders of Pregnancy: Prevalence, classification and adverse outcomes in Northwestern Saudi Arabia. (1999) Ann Saudi Med 19(6): 557-560.