Pediatric Sepsis
Krishan Kumar , Anthony Boutin
Affiliation
- 1Division of Allergy Immunology, Department of Medicine, Nassau University Medical Center, New York
- 2Division of Pediatric, Department of Emergency Medicine, Nassau University Medical Center, New York
- 3Division of Adult Emergency Medicine, Department of Emergency Medicine, Nassau University Medical Center, New York
Corresponding Author
Marianne Frieri, Nassau University Medical Center, Department of Medicine, 2201 Hempstead Turnpike, East Meadow, New York, 11554; E-mail: mfrieri@numc.edu
Citation
Frieri, M., et al. Pediatric Sepsis. (2017) J Palliat Care Pediatr 2(1): 60-62.
Copy rights
© 2017 Frieri, M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Pediatric sepsis; Protein C deficiency; Neonatal sepsis; Innate: Immunity
Abstract
The purpose of this article is to understand pediatric sepsis, activation of the innate immune system and a synergistic relationship between the loss of organ functions and sepsis pathophsiology. Many complex factors such as genetics, physical agents, mediators and effectors are involved in the development of organ failure both in sepsis in children and neonates. The patient’s immune surveillance could fail to eliminate the pathogens with a release with inappropriate activation. These topics are very important for pediatricians, immunologists, and neonatologists.
Introduction
Sepsis
Injury due to trauma can induce immune function changes, which can lead to both pro inflammatory activation known as Systemic Inflammation Response Syndrome (SIRS) and an anti-inflammatory reaction with immune suppression known as Compensatory Anti-Inflammatory Response Syndrome (CARS). SIRS with proven infection is referred to as sepsis, however clinically it is often difficult to isolate the microbial inoculum, making the differential diagnosis between SIRS and sepsis difficult[1]. This differential diagnosis is in turn crucial for further therapeutic decisions: is an antimicrobial therapy and aggressive search for a septic focus with all its side-effects necessary or is a focused symptomatic therapy of the SIRS the adequate treatment concept[1]?
Previous reports on Emergency Medical Services (EMS) transportation of pediatric patients have demonstrated a high rate of overutilization. However, there is also a concern that pediatric patients may underutilize EMS for emergencies that might benefit from EMS. This article compares EMS utilization rate between adult and pediatric patients for high-acuity patients and for the most common reasons for transport[2]. As compared with adults, pediatric patients are less likely to utilize EMS for transport to the hospital for both routine and emergent complaints. The definition of inappropriate utilization of EMS for pediatric transport, which has largely focused on inappropriate overutilization, should also incorporate the potential of underutilization for critical patients[2].
Prediction models for neonatal health care-associated sepsis have been studied[3].
Systemic Inflammation Response Syndrome and Sepsis
Systemic Inflammation Response Syndrome (SIRS) vital signs are common among medical pediatric patients presenting to an ED, and critical illness is rare. The majority of patients with SIRS vital signs were discharged without IV therapy and without readmission. Patients with SIRS vital signs had a statistically significant increased risk of critical care requirement, ED IV treatment, ED laboratory tests, admission, and readmission[4].
However, SIRS vital sign criteria did not identify the majority of patients with mortality or need for critical care. SIRS vital signs had low sensitivity for critical illness, making it poorly suited for use in isolation in this setting as a test to detect children requiring sepsis resuscitation[4].
Plasma gelsolin levels in premature infants at 72 hours and were significantly lower in patients with respiratory distress syndrome and in patients who were administered surfactant therapy and in patients who developed sepsis[5] Plasma gelsolin levels at 28 days were significantly lower in patients who developed bronchopulmonary dysplasia and retinopathy of prematurity (P < 0.05). Thus, low plasma gelsolin levels in the first postnatal month may be associated with poor outcomes in premature infants[5].
Low Circulating Protein C (PC) levels have been observed in sepsis, especially in patients with Neisseriae Meningitides infections[6] Poor clinical outcome and high limb amputation rates have been associated in infected patients with low circulating PC levels. Published studies using activated PC replacement therapy patients with sepsis have shown reduced mortality rates; however, its use has been associated with severe bleeding events. Pediatric sepsis studies using non-activated plasma-derived PC ( Ceprotin®) are lacking[6]. The authors present a retrospective study in children with sepsis who were treated with Ceprotin® focusing on amputation rate post treatment. The median time between admission to intensive care and Ceprotin® administration was 10 hrs. Limb amputation rate was reduced (16 - 23% versus 30 - 50% from previous studies) and there were no haemorrhagic events observed. This study demonstrates the safe administration of non-activated plasma-derived PC concentrate in patients with sepsis who are coagulopathic and it associated with a reduction in amputation rates[6].
Inflammatory and coagulation processes are both affected in meningococcaemia[7]. Severe acquired protein-C deficiency in meningococcaemia is usually associated with substantial mortality: in survivors, skin grafts, amputation, and end-organ failure are not uncommon. Protein C is a natural anticoagulant and also has important anti-inflammatory activity. These authors assessed the effects of early replacement therapy with protein-C concentrate together with continuous veno-venous haemodiafiltration and conventional treatment in meningococcaemia[7].
Twelve patients aged between 3 months and 27 years with meningococcaemia and severe acquired protein-C deficiency (mean 0.20 IU/mL) were studied. All patients had septic shock, widespread purpura, skin necrosis, and disseminated intravascular coagulopathy. After a test dose of protein-Cconcentrate, patients received a continuous infusion with the dose adjusted daily to keep the plasma concentration between 0.8 and 1.2 IU/mL[7]. The acquired severe deficiency of protein C in meningococcaemia contributes to the pathogenesis of the thrombotic necrotic lesions in the skin and other organs and probably has an important role in the inflammatory response. Protein-C therapy is merely one approach to improve the host response in this syndrome. These authors suggested that a double-blind, randomised, controlled multicentre trial is needed to confirm their results[7].
Newborn Hypoxia and Reactive
Oxygen Species
A review on hypoxia inducible factor (HIF) signaling and experimental persistent pulmonary hypertension of the newborn was conducted[8]. Mitochondrial Reactive Oxygen Species (ROS) levels and nuclear factor kappa-light-chain-enhancer of activated B cells (NFB) activity are increased in an animal model of Persistent Pulmonary Hypertension of the Newborn (PPHN). These events can trigger Hypoxia Inducible Factor (HIF) signaling in response to hypoxia and complex physiological and biochemical processes facilitate the fetal to newborn transition, and abnormal lung development and/or vascular dysfunction may disrupt these events[8].
The authors stated increased HIF signaling in PPHN is triggered by stretch, via mechanisms involving mitochondrial ROS and NFκB. Hypoxia substantially amplifies HIF activity in PPHN vascular cells. Targeting these signaling molecules may attenuate and reverse pulmonary vascular remodeling associated with PPHN[8,9]. This study identified components of the HIF signaling pathway that may contribute to the pathogenesis of PPHN and further studies are warranted in vivo and in vitro to investigate the mechanisms involved to improve current detection and treatment strategies for babies with PPHN[8].
Innate Immunity and Sepsis
The cell-regulated innate immune system often contributes to posttraumatic multiple organ dysfunctions or even multiple organ failure. With a cell fraction of 50 – 60% of all leukocytes, polymorphonuclear leukocytes have been shown to be key effector cells within the innate inflammatory immune reaction[9].
The innate immune system is an immune monitor and has a very prominent role in organ failure after trauma. Polymorphonuclear phagocytes and monocytes are the main effector- cells of the innate immune system that are involved in organ failure and are controlled by cytokines.
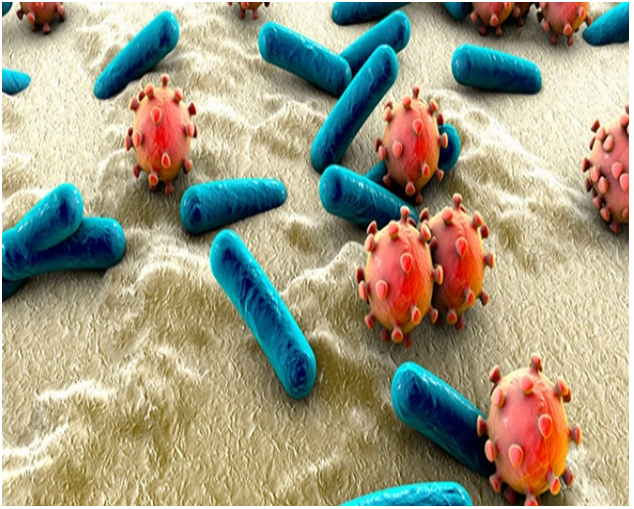
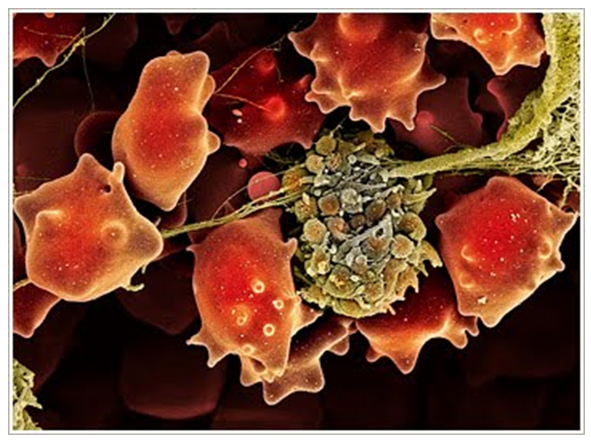
Neutrophils play an essential role in the body’s innate immune response to infection. To protect the host, these phagocytic cells possess an impressive array of microbicidal weapons that can be brought to bear on an invading pathogen, including a variety of toxic oxygen radical species and proteolytic enzymes[10]. Figure 1 illustrates the pathophysiology of sepsis in two different stages.
Figure 1: Pathophysiology Sepsis.
Stage I: Bacteremia Fibrin.
A recent paper by one of the authors stated marked increase in serum procalcitonin during the course of a septic process often indicates an exacerbation of the illness, and a decreasing level is a sign of improvement[11]. Integrating use of procalcitonin into pediatric practice in the early golden hours of sepsis diagnosis and antibiotic stewardship program would be beneficial[12].
During sepsis, there is an increase in CALC-1 gene expression which causes a release of procalcitonin and, more importantly, their levels persist for relatively long periods of time and correlate with sepsis severity and mortality[12].
State II: Macrophages Responses if the Host Coagulation, Complement, Organ Dysfunction and Death.
Septic children aged between 28 days and 14 years were divided into sepsis and septic shocks. CRP and Procalcitonin (PCT) were measured at admission. CRP levels were not statistically different for groups and time points.PCT was better than CRP for diagnosing sepsis and septic shock, mainly at admission, and is related to disease severity[13].
Conclusion
Sepsis, protein C deficiency, biomarkers to identify neonatal sepsis were reviewed in this article. Defense mechanisms and physiological functions of the immune system were also covered and the pathophysiology of sepsis. These areas are very important for pediatricians, neonatologists and immunologists on the floor and in the hospital.
References
- 1. Novotny, A.R. Biomarkers in SIRS and sepsis: Quo Vadis? (2010) J Emerg Trauma Shock 3(1): 36-38.
Pubmed || Crossref || Others - 2. Richards, M.E., Hubble, M.W., Zwehl-Burke, S. “Inappropriate” pediatric emergency medical services utilization redefined. (2011) Pediatr Emerg Care 27(6): 514-518.
Pubmed || Crossref || Others - 3. Verstraete, E.H., Blot, K., Mahieu, L., et al. Prediction Models for Neonatal Health Care-Associated Sepsis: A Meta-analysis. (2015) Pediatrics. 135(4): e1002-e1014.
Pubmed || Crossref || Others - 4. Novotny, A.R., Reim, D., Assfalg, V., et al. Mixed antagonist response and sepsis severity-dependent dysbalance of pro- and anti-inflammatory responses at the onset of postoperative sepsis. (2012) Immunobiology 217(6): 616–621.
Pubmed || Crossref || Others - 5. Kose, M., Elmas, T., Gokahmetoglu, S., et al. Predictive value of gelsolin for the outcomes of preterm neonates: a pilot study. (2014) Pediatr Int 56(6): 856-859.
Pubmed || Crossref || Others - 6. Piccin, A., O' Marcaigh, A., Mc Mahon, C., et al. Non-activated plasma-derived PC improves amputation rate of children undergoing sepsis. (2014) Thromb Res 134(1): 63-67.
Pubmed || Crossref || Others - 7. Smith, O.P., White, B., Vaughan, D., et al. Use of protein-C concentrate, heparin, and haemodiafiltration in meningococcus-induced purpura fulminans. (1997) Lancet 350(9091): 1590-1593.
Pubmed || Crossref || Others - 8. Wedgwood, S., Lakshminrusimha, S., Schumacker, P.T., et al. Hypoxia inducible factor signaling and experimental persistent pulmonary hypertension of the newborn. (2015) Front Pharmacol 6: 47.
Pubmed || Crossref || Others - 9. Hietbrink, F., Koenderman, L., Rijkers, G.T., et al. Trauma: the role of the innate immune system. (2006) World J Emerg Surg 1: 15.
Pubmed || Crossref || Others - 10. Swain, S.D., Rohn, T.T., Quinn, M.T. Neutrophil priming in host defense: role of oxidants as priming agents. (2002) Antioxid Redox Signal 4(1): 69-83.
Pubmed || Crossref || Others - 11. Frieri, M., Shiferaw, B., Kumar, K., et al. Role of Harmful Molecules in the Pathogenesis of Sepsis: A Review. (2015) J Natur Sci (JNSCI) 1(8): e142.
Pubmed || Crossref || Others - 12. Decembrino, L., De Amici, M., Pozzi, M., et al. Serum Calprotectin: A Potential Biomarker for Neonatal Sepsis. (2015) J Immunol Res 2015: 147973.
Pubmed || Crossref || Others - 13. Fioretto, J.R., Martin, J.G., Kurokawa, C.S., et al. Comparison between procalcitonin and C-reactive protein for early diagnosis of children with sepsis or septic shock. (2010) Inflamm Res 59(8): 581-586.
Pubmed || Crossref || Others