Rapid Vision Loss in Idiopathic Intracranial Hypertension: A Case Report
Sourya Acharya , Samarth Shukla
Affiliation
- 1Resident, Department of General Medicine, JNMC, Sawangi [Meghe], Wardha, India
- 2Professor, Department of General Medicine, JNMC, Sawangi [Meghe], Wardha, India
- 3Professor, Department of Pathology, JNMC, Sawangi [Meghe], Wardha, India
Corresponding Author
Nabeel Hashmi, Yashodha PG Hostel, room no S-19, Sawangi [Meghe], Wardha, India, Tel: 9689323925; E-mail: nabhas88@yahoo.in
Citation
Hashmi, N., et al. Rapid Vision Loss in Idiopathic Intracranial Hypertension: A Case Report. (2017) Clin Trials Case Stud 2(1): 58- 60
Copy rights
© 2017 Hashmi, N. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Idiopathic intracranial hypertension; Cranial nerve; Papiloedema; Headache
Abstract
Idiopathic Intracranial Hypertension [IIH] formerly knowns as pseudotumour cerebri is a condition characterized by elevated intracranial pressure with normal Cerebro Spinal Fluid [CSF] findings and without a demonstrable evident cause for the same in neuroimaging or other evaluation. The clinical features can be headache, papilloedema, cranial nerve palsies. Vision loss can rarely occur in severe raised intracranial pressure. We present a case of 25 year old female who presented with bilateral rapidly progressive vision loss due to IIH.
Introduction
Idiopathic Intracranial Hypertension [IIH] is a condition where CSF is under high pressure in absence of a brain tumour or other primary cause, therefore earlier it was known as pseudotumour cerebri. Pathologically there is no structural obstruction to the CSF flow; there is defective re-absorption of CSF at the level of arachnoid granulations without evidence for excessive CSF production. Differential diagnoses are shown in table 1.
Table 1: Differential Diagnosis of Idiopathic Intracranial Hypertension.
| 1. Scarring from previous inflammations [meningitis, sequel to subarachnoid haemorrhage] |
| 2. Venous sinus thrombosis |
| 3. Hypercoaguable states |
| 4. Arachnoiditis |
| 5. Hypervitaminosis A |
| 6. Autoimmune conditions[eg, Systemic Lupus Erythematous] |
| 7. Drugs [tetracyclines, oral contraceptives, sudden withdrawal of steroids] |
It predominantly affect females, usual age of presentation is around third decade of life.
History of sudden weight gain is a known predisposing factor. Evidence showed that losing weight around 5 to 10% improves symptoms of IIH.
Case Report
A 25 year old unmarried obese female presented to us with the complaints of headache on/off since 1 month, rapid diminision of vision since 4 days. There was no history of vomiting, diplopia, convulsions, fever, disorientation. The headache was generalized and was worse in the morning hours until three days prior she used to take tablet acetaminophen or ibuprofen as advised by her family physician. Fifteen days before the visual complaints she visited another hospital for headache where Computed Tomography [CT] scan was done which was normal and she was prescribed anti migraine drugs without any relief. She was an engineering student.
Three days prior while attending lecture she was not able to see the words on blackboard clearly, this visual loss develop rapidly till she could not see completely. She reached stage of near total blindness for which she reached hospital.
On general examination she was obese [32 kg/m²], pulse: 62/min regular. BP-140/96 mm hg, JVP: normal, there was no oedema, CNS examination: higher functions were normal.
Cranial nerve examination revealed visual acuity in the right eye was present only for the hand movements and left eye: pl/pr present. Pupils-normal size reacting to light, there was slight lateral rectal palsy on the left.
Other cranial nerves motor and sensory examination were normal, no signs of meningeal irritation.
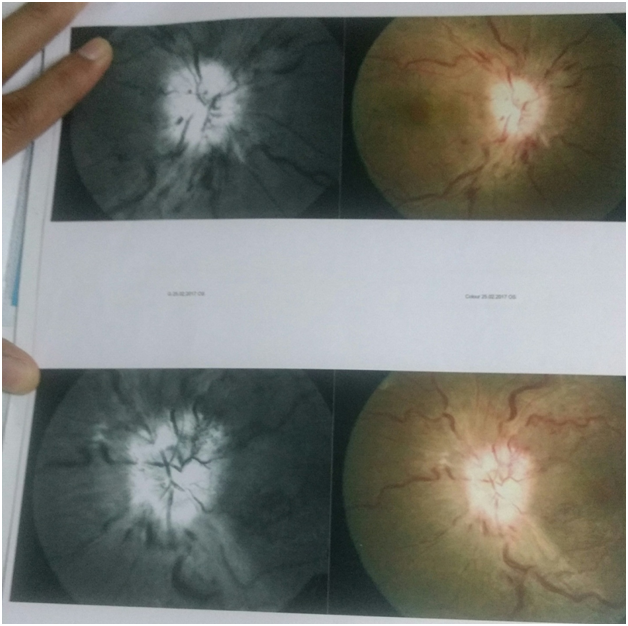
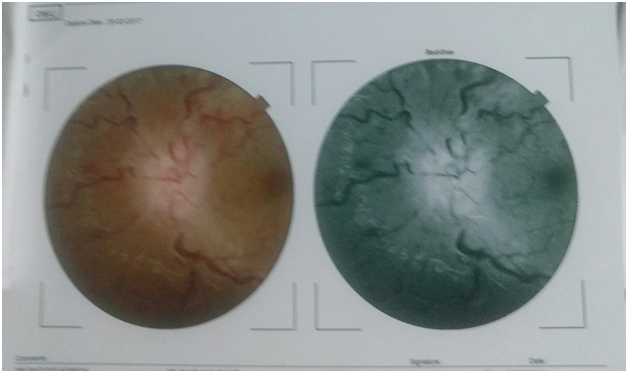
Jolt accentuation maneuver was negative. Repeat CT scan was normal, Magnetic Resonance Imaging [MRI], MR Venogram were normal. Fundus examination revealed [Figure 1,2. Table 2]:
• Complete Blood Counts [CBC], Kidney Function Test [KFT], Liver Function Test [LFT] were normal
• ECG was normal
With view of above findings diagnosis of intracranial hypertension was made.
Figure 1:
Figure 2:
Table 2: Fundus examination revealed.
| RIGHT EYE | LEFT EYE | |
|---|---|---|
| OPTIC DISC | Disc Oedema++ | DISC Oedema++ |
| FUNDUS | Dialated tortouos veins Retina on | Dialated tortuous veins Retina on |
She was prescribed, tablet acetazolamide, tapering course of tablet prednisolone. She was subjected to lumboperitoneal shunt, after which there was significant visual recovery within five days. She was discharged on tablet acetazolamide 250 mg tds and is awaiting follow up.
Discussion
The incidence of IIH is approximately 1/ 100000 per year and it has risen to 13/ 100000 per year in obese females in their second to fourth decade of life[1-3]. German physician Heinrich Quinck first described it in 1893. In 1904 Max Nonnes gave the name pseudotumour cerebri. Because the condition was actually benign later on a new nomenclature by the name of benign intracranial hypertension became popular but contrary to this the current name discarded the word benign because upto 25% of cases can present with blindness if not treated properly. Hence the final term IIH prevails. The current diagnostic citeria for IIH is modified dande criteria Table 3[4].
Table 3: Clinical Definition of Idiopathic Intracranial Hypertension [Modified Dandy Criteria].
| 1. Signs and symptoms of increased intracranial pressure. |
| 2. No localizing neirologic findings [Cranial nerve VI palsies are allowed]. |
| 3. Normal neuroimaging [with the exception of an empty sella]. |
| 4. Opening pressure of lumbar puncture of greater than 250 mm water, with normal CSF. |
| 5. No other cause of increased intracranial pressure present. |
The common clinical presentations are headache which is vague, poorly localized, worsens in the morning, can be exacerbated by coughing, sneezing and valsalva maneuver, common cranial nerve involved are third and sixth cranial nerve and presents with horizontal diplopia, rarely a pulsatile tinnitus, which is exacerbated by supine or bending is present.
Severe vision loss is a dangerous complication and it may lead to permanent blindness by causing secondary optic atrophy. Our case presented with rapidly progressive vision loss that would have lead to permanent blindness if not would have intervened early. The patient who present with rapid vision loss or ophthalmoplegia needs urgent management for preservation of vision, modalities available are medical and surgical. CSF diversion procedure like ventroperitoneal shunt or optic nerve fenestration are usually done, optic nerve fenestration is superior to ventroperitoneal shunting. It is done by partial unroofing of the orbit and incising dural arachnoid sheaths surrounding optic nerve relieving the pressure.
The complication of fenestration is vascular obstruction and permanent visual loss that puts this procedure in moderately high risk category. Lumboperitoneal shunt is a new method adapted by some surgeons; medical managemament is usually an adjuvent. Drugs like mannitol, carbonic anhydrase inhibitior [acetazolamide] and corticosteroids are used.
Conclusion
IIH is a common condition with several risks. Vision loss is a catastrophic complication. Management is holistic and starts with lifestyle modification in the form of weight loss, drugs and ultimately wherever required optic nerve fenestration and shunt surgeries.
References
- 1. Durcan, F.J., Corbett, J.J., Wall, M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. (1988) Arch Neurol 45(8): 875-877.
Pubmed || Crossref || Others - 2. Radhakrishnan, K., Ahlskog, J.E.,et al. Idiopathic intracranial hypertension (pseudotumor cerebri). Descriptive epidemiology in Rochester, Minn, 1976 to 1990. (1993) Arch Neurol 50(1): 78-80.
Pubmed || Crossref || Others - 3. Gordon, K. Pediatric pseudotumor cerebri: Descriptive epidemiology. (1997) Can J Neurol Sci 24(3): 219-221.
Pubmed || Crossref || Others - 4. Smith, J.L. Whence pseudotumor cerebri? (1985) J Clin Neuroophthalmol 5(1): 55-56.
Pubmed || Crossref || Others