Surgical Evacuation of First Trimester Missed Miscarriage with & without use of Transabdominal Ultrasound: A Randomized Clinical Trial
Essam R. Othman1, Ahmed M. Abbas1*, Mohamed K. Ali1, Mahmoud Abdel-Reheem1, Diaa Eldeen M. Abd El Aal1, Gamal H. Sayed1
Affiliation
1Department of Obstetrics & Gynecology, Women Health Hospital, Faculty of Medicine, Assiut University
Corresponding Author
Dr. Ahmed M. Abbas, MD, Department of Obstetrics and Gynecology, Assiut University, Egypt, Women Health Hospital, 71511, Assiut Egypt; Tel: +20 88 2414616/ Cell: +20 10033851833, Fax: +20 88 9202503; E-mail: bmr90@hotmail.com
Citation
Abbas, A.M., et al. Surgical Evacuation of First Trimester Missed Miscarriage With & Without Use of Transabdominal Ultrasound: A Randomized Clinical Trial. (2016) J Gynecol Neonatal Biol 2(1): 5-8.
Copy rights
©2 016 Abbas, A.M. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Gestational diabetes mellitus; American Diabetes Association; Impaired fasting glucose; Impaired glucose tolerance; HbA1c; Dysglycaemia
Abstract
Background: Surgical evacuation is one of the most popular methods of termination of pregnancy in cases of missed miscarriage. The current study aims to compare the improvement of surgical evacuation of first trimester miscarriage when done with and without transabdominal ultrasonographic guide.
Materials and methods:
Setting: Women Health Hospital, Assiut University, Egypt.
Design: A randomized clinical trial conducted on 200 pregnant women with 1st trimester miscarriage who scheduled for surgical evacuation. It carried out in the period between the 1st of May 2014 and the 30th of April 2015. The women were randomly assigned to either undergone surgical evacuation blindly (group I) or under ultrasound guidance (group II). The main outcome measures were achievement of complete miscarriage, operative time and blood loss during the procedure.
Results: Two-hundred participants were recruited in the study. The mean amount of blood loss during the procedure was significantly higher in group I when compared with group II (P = 0.002). Also there was a statistical significant difference in the operative time between both groups, group I showed longer time than in group II (P = 0.0001). After surgical evacuation, 14 cases (14%) in group I and 3 cases (3%) in group II were reported to have remnants of conception. No cases of uterine perforation occurred in both groups.
Conclusion: The use of intraoperative ultrasound during surgical evacuation is associated with a significant reduction in its complications, however; the cost of using ultrasound needs further investigations.
Introduction
The miscarriage considers the most common cause of fetal demise all over the world[1]. The majority of cases occur in the first trimester[2]. The termination of miscarriage may be by medical or surgical methods. However, the surgical methods represents the greater part of termination[3]. Therefore, the safety of this procedure is a worldwide public health concern[4]. Many clinical studies have been reported the safety of surgical evacuation in the first trimester[5].
The suction-aspiration or vacuum aspiration is the most common surgical methods of induced miscarriage. This consists of removing the fetus, embryo, placenta, and membranes by suction using a manual syringe or electric pump. However; these technique always need cervical dilation before aspiration[6]. The menstrual extraction does not require cervical dilation and can be used in very early pregnancy[7].
The surgical evacuation is generally considered safe, however; short-term complications are reported due to need of dilatation of the cervix and incomplete evacuation because the surgeon is the only one who can decide the end of the operation depending on his subjective sense[8].
However; with continuous ultrasound guidance, the process could be almost complete because the ultrasound can accurately identify the direction and size of the uterus, position of the gestational sac, observe the insertion of surgical instruments and the advancement of the operation especially when the configuration of the uterus is distorted[9].
At present ultrasound is not considered to be an essential pre-requisite for abortion in all cases[10], so our study aims to detect if complete evacuation can be achieved by ultrasonographic assistance or not. We also tried in this study to compare the operative time, amount of blood loss and the occurrence of accidental uterine perforation during the procedure with and without use of ultrasound.
Materials and Methods
The current study is a clinically registered single blinded, parallel, RCT (NCT02580175) compassing the effect of ultrasound guidance during surgical evacuation of 1st trimester miscarriage. The ethical review board of the Faculty of Medicine of the Assiut University approved the study. The participants were recruited from the Outpatient Obstetrics Clinic of the Assiut Women’s Health Hospital. It was carried out in the period between the 1st of May 2014 and the 30th of April 2015. All study participants signed a written informed consent before enrollment in the study. This trial was designed and reported according to the revised recommendations of ClinicalTrials.gov for improving the quality of reporting RCTs.
Eligible participants
All study participants had a clinical history taken and general physical examination performed in the antenatal clinic. An initial ultrasound examination was performed to confirm presence of non-viable intrauterine pregnancy, to determine the gestational age, and number of gestational sacs and fetuses.
All women with confirmed non-viable first trimester intrauterine pregnancy with no contraindication to surgical evacuation under general anesthesia were included in the study. We had excluded cases with gestational age more than 13 weeks, hemo dynamically unstable, or if there is suspicion of an ectopic pregnancy.
Randomization
Randomization was done using a computer-generated random table. Eligible patients who consented were randomly assigned to blind evacuation or sonographic guided evacuation. Allocation concealment was done using serially numbered closed opaque envelopes. Each envelope was labeled with a serial number and had a card showing the intervention type inside. Allocation was never changed after opening the envelopes.
Intervention
Eligible participants were randomly assigned to one of two groups: group I (blinded evacuation); which ring evacuation was performed in the conventional way without use of ultrasound followed by sharp gentle curettage until complete evacuation. Group II (evacuation under ultrasound guidance); which ring evacuation was performed under ultrasound guidance using real-time ultrasound by 3.5 MHz convex transabdominal probe (Mindray-6600, China) followed by sharp gentle curettage until complete evacuation. The probe was placed longitudinally on the patient’s abdomen and the uterus scanned longitudinally from the cervix to the fundus. The surgery was considered complete when the endometrial cavity appeared as a regular echogenic line. The operation was performed as a day case under general anesthesia.
Study outcomes
The primary outcome was to detect if complete evacuation was achieved by ultrasound guidance or not. Secondary outcomes included the operative time, amount of blood loss and the occurrence of accidental uterine perforation during the procedure.
Follow-up schedule
All study participants were followed at the end of the operation. We evaluated the blood loss: by subtracting the dry weight of absorbing materials (pads, sponges, etc) from the weight of blood containing materials (using sensitive balance) and using the conversion 1 gm weight = 1 mL to quantify the blood volume contained in the materials (the weight of the pad used is 50 gram) then added this with the amount of blood loss in graduated container. We also assessed the hemoglobin level for all patients before and after evacuation. In addition to operative time which calculated from introduction of the ring till the end of the procedure. As regard the assessment of the retained parts of conception; transvaginal ultrasound was done for all cases 4hours after evacuation, presence of thick endometrium more than 15 mm is indicative of presence of retained parts of conception[7].
Sample size calculation
Sample size was calculated using Epi Info software version 7. A sample of 200 women attending Women’s health Hospital (100 cases in each arm) was needed to detect an effect size of 0.3 between the two group regarding the efficacy of ultrasound guidance during uterine surgical evacuation, with a p value < 0.05 and 95% power.
Data collection and analysis
The data were collected and entered on Microsoft access database to be analyzed using the Statistical Package for Social Science (SPSS Inc., Chicago, version 18). Comparisons between the groups were done using Student’s t-test to compare the mean values between groups in scale variables. However, χ² test was used to compare the dichotomous and ordinal variables in the groups. For analysis P-Value < 0.05 was considered significant.
Results
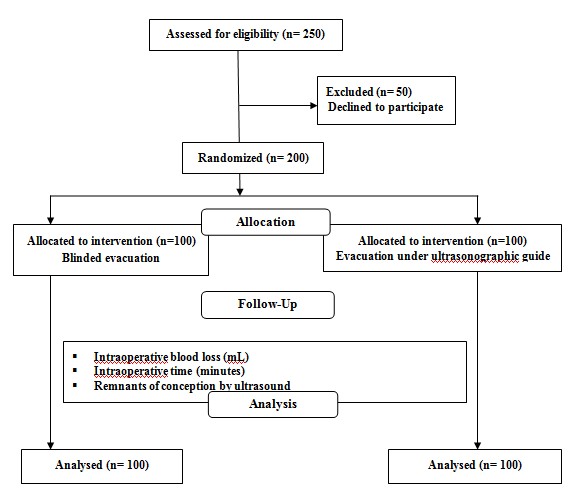
Two-hundred participants with proven first trimester miscarriage were approached to participate in this study (study flow chart, Figure 1). Table 1 shows the demographic characteristics of the study participants. No significant differences were found between the two study groups as regards patients’ age, parity, gestational age and number of previous abortions or cesarean deliveries.
Table 1: Characteristics of the study participants
| GROUP I (Blind evacuation) n = 100 |
GROUP II (Ultrasound guided evacuation) n = 100 |
P-value | |
|---|---|---|---|
| Age (years) mean ± SD | 25.70 ± 4.94 | 25.21 ± 5.25 | 0.498 |
| Parity mean ± SD | 2.5 ± 0.98 | 2.3 ± 0.77 | 0.26 |
| Gestational age (weeks) mean ± SD | 9.49 ± 1.67 | 9.48 ± 1.55 | 0.965 |
| Previous abortion, n | 51 | 46 | 0.392 |
| Previous cesarean, n | 46 | 39 | 0.317 |
SD standard deviation
Figure 1: Flow Chart of the study participants
The mean amount of blood loss during the procedure was significantly higher in group I when compared with group II (P = 0.002), but no statistically significant difference between both groups as regard the hemoglobin level before and after evacuation. Also there was a statistical significant difference in the operative time between both groups, group I showed longer time than in group II (P = 0.0001) (Table 2).
Table 2: Comparison of the study outcomes between the two groups
| Characteristics | GROUP I (Blind evacuation) n = 100 |
GROUP II (Ultrasound guided evacuation) n = 100 |
P-value |
|---|---|---|---|
| Blood loss (ml) mean ± SD | 58.70 ± 18.57 | 51.00 ± 16.65 | 0.002* |
| Preoperative hemoglobin (gm/dl) mean ± SD | 10.23 ± 1.11 | 10.30 ± 0.91 | 0.593 |
| Postoperative hemoglobin (gm/dl) mean ± SD | 9.42 ± 1.16 | 9.49 ± 0.95 | 0.623 |
| Operative time (minutes) mean ± SD | 5.23 ± 1.05 | 4.08 ± 1.09 | 0.0001* |
| Presence of remnants, n (%) | 14 (14) | 3 (3) | 0.0001* |
SD standard deviation
(*) statistical significant difference
After surgical evacuation, the failure rate in the ultrasound guided group was 3 cases (3%) compared to 14 cases (14%) of the group without ultrasound guidance with statistical significant difference (P = 0.0001) (Table 2). No cases of uterine perforation occurred in both groups.
Discussion
In the current RCT we had compared the outcome of surgical evacuation in first trimester missed miscarriage with and without ultrasound guidance. Ultrasound guided evacuation had a significant beneficial effect in reducing blood loss, operative time of the procedure with the advantage of complete evacuation.
Our study was in agreed with Say et al who compared seven randomized trials in a Cochrane review and concluded that the rate of incomplete evacuation is more in medical methods compared to vacuum aspiration and the duration of bleeding was more in medical method than vacuum aspiration[11].
Another randomized study conducted by Fait et al. who compared the results between the suction evacuation with or without ultrasonographic guidance as we did. However; they reported no significant difference between both groups in the amount of blood loss, operative time which differs from our results. But they reported 7 cases with retained parts of conception without need for re-evacuation[12].
Acharya conducted another randomized controlled trial comparing the surgical evacuation of missed miscarriage cases with or without ultrasound and we found that the operative time is shorter and blood loss is fewer during the evacuation when ultrasound was used. However; no retained products of conception while were reported when using the ultrasound[13].
The most recent randomized study was done by Elsayed in 2013. He supported our results and concluded that surgical evacuation under ultrasonographic guidance is beneficial because there are significant cases with missed miscarriage which can be incompletely evacuated without the use of the ultrasound guidance[14].
We found that the presence of retained products of conception post evacuation was more common in blind evacuation group (14 cases) than ultrasound guidance group (3 cases) with shorter operative time. Although; the blood loss was less with ultrasound guidance, there was no significant difference between both groups as regard the hemoglobin level.
Our explanation to these results may be due to; firstly the ultrasound allows the surgeon to see the uterine cavity and its contents well and to be targeted directly on product of conception which he wants to evacuate. Secondly, the surgeon can decide at which time to end the evacuation therefore less operative time and less the amount of blood loss is associated with ultrasound use. Thirdly, he can see the uterine cavity well so the presence of remnants is rare with relatively low incidence of perforation.
The explanation of that hemoglobin level before and after evacuation as indicator of blood loss between the two groups is not significant may be attributed to that the amount of blood loss between the cases before reaching the emergency unit was different and the amount of blood loss intraoperative is small (measured in ml) in a way that not affect the hemoglobin level significantly.
Conclusion
The study concluded that the use of intraoperative ultrasound during surgical evacuation is associated with a significant reduction in its complications, however; the cost of using real time ultrasound guidance during evacuation needs further research.
Conflict of Interest:
We have no conflict of interest to declare.
References
- 1. Abbasi, S., Jamal, A., Eslamian, L., et al. Role of clinical and ultrasound findings in the diagnosis of retained products of conception. (2008) Ultrasound Obstet Gynecol 32(5): 704-707.
- 2. Chambers, D.G., Mulligan, E.C. Treatment of suction termination of pregnancy retained products with misoprostol markedly reduces the repeat operation rate. (2009) Aust N Z J Obstet Gynecol 49(5): 551-553.
- 3. Farquharson, R.G., Jauniaux, E., ESHRE Special Interest Group for Early Pregnancy (SIGEP), et al. Updated and revised nomenclature for description of early pregnancy events. (2005) Hum Reprod 20(11): 3008–3011.
- 4. Kulier, R., Kapp, N. Comprehensive analysis of the use of pre-procedure ultrasound for first- and second-trimester abortion. (2010) Contraception 83(1): 30–33.
- 5. Mulayim, B., Celik, N.Y., Onalan, G., et al. Sublingual misoprostol after surgical management of early termination of pregnancy. (2009) Fertil Steril 92(2): 678–681.
- 6. Sedgh, G., Henshaw, S., Singh, S., et al. Induced abortion:estimated rates and trends worldwide. (2007) Lancet 370(9595): 1338–1345.
- 7. Ustunyurt, E., Kaymak, O., Iskender, C., et al. Role of transvaginal sonography in the diagnosis of retained products of conception. (2008) Arch Gynecol Obstet 277(2): 151-154.
- 8. Bennett, I., Baylson, M., Kalkstein, K., et al. Early abortion in family medicine: clinical outcomes. (2009) Ann Fam Med 7(6): 527–533.
- 9. Blumenthal, P., Clark, S., Coyaji, K.J., et al. Providing medical abortion in developing countries: An introductory guidebook. In: Abuabara K, Blum J, editors. (2004) Gynuity Health Projects.
- 10. Sawyer, E., Ofuasia, E., Ofili-Yebovi, D., et al. The value of measuring endometrial thickness and volume on transvaginal ultrasound scan for the diagnosis of incomplete miscarriage. (2007) Ultrasound Obstet Gynecol 29(2): 205–209.
- 11. Say, L., Brahmi, D., Kulier, R., et al. Medical versus surgical methods for first trimester termination of pregnancy. (2002) Cochrane Database of Syst Rev (4) :CD003037.
- 12. Fait, G., Amster, R., Tugendreich, D., et al. Use of ultrasonography to guide first-trimester pregnancy terminations obviates the need for sharp curettage. (2004) Fertil Steril 78(5): 1131-1132.
- 13. Acharya, G., Morgan, H., Paramanantham, L., et al. A randomized controlled trial comparing surgical termination of pregnancy with and without continuous ultrasound guidance. (2004) Eur J Obstet Gynecol Reprod Biol 114(1): 69-74.
- 14. Elsayed, M.A. Routine ultrasound guided evacuation of first trimester missed abortion versus blind evacuation. (2014) MEFSJ 19(3): 171–175.